![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
What causes pityriasis versicolor (tinea versicolor)?
How does it present? Dx? How do you treat it? |
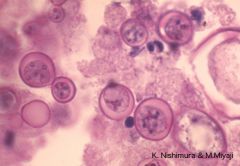
Malassezia furfur - lipophilic spherical yeast, hyphae
Discoloration (hypo/hyper-pigmentation) on skin, affected areas do not tan KOH prep, fluoresces golden green-yellow, spaghetti & meatballs Tx with keratolytic agents, topical ketoconazole |
|
|
What causes tinea nigra?
How does it present? Dx? Tx? |
Exophiala (hortaea) werneckii, branched septate hyphae, budding yeast
pdx melanin --> hyperpigmentation Microscopic view of fungi Tx: keratolytics, salicylic acid, azoles |
|
|
What causes black piedra?
How does it present? Dx? Tx? |
Piedraia hortai (tropical, underdevo countries)
Hard nodules along infected hair shaft Dx N/A Tx: hair removal, topical antifungals |
|
|
What causes white piedra?
How does it present? Dx? Tx? |
Genus trichosporon
Px: larger, softer, yellowish nodules on hairs Dx: N/A Tx: hair removal, topical antifungals |
|
|
What are the dermatophytes?
How does it reproduce? How does it infect? |
Skin, hair, nail fungal infections
Microsporum, trichophyton, epidermophyton Sexual reproduction, ascospores Infects with keratinase (secreted enzyme) --> digests keratin --> scaling of skin, loss of hair, crumbling of nails |
|
|
What is tinea pedis?
How does it present? Dx? Tx? |

Athlete's foot, most common infection, VIA CONTACT
T. rubrum: not viable for long post-shedding from host E. flocossum: not assoc w chronic infxn, but resistant conidia can stay in host a long time T. mentagrophytes: rodents in environment M. canis: colonized cat Px: itching vesicles and pustules, skin cracked, watery discharges, macerated, peeling Tx: E. flocossum, T. mentagrophytes: topical antifungal Tx: T. rubrum & other resistant strains: oral antifungals (griseofulvin, terbinafine, itraconazole) |
|
|
What is tinea cruris?
Px? Dx? Tx? |
Jock itch, tropics & men
T. rubrum, T. mentagrophytes, E. flocossum |
|
|
What is tinea corporis?
Px? Dx? Tx? |

Body/skin, tropics
Microsporum canis, T. rubrum, T. mentagrophytes Tiny red purple, itching --> spreads peripherally with actively inflamed vesiculo-pustular margin + healing scaly center TX: Uncomplicated infxns - creams/lotions/powders TX: T. rubrum & other resistant - griseofulvin, itra-/flu-conazole, terbinafine |
|
|
What is tinea barbae?
Px? Dx? Tx? |
Beard infection
T. rubrum (infrequent), T. verrucosum (cows), T. mentagrophytes (cows, dogs, horses) Via contact with animals in rural environment Circular margin --> invasion & spread --> nodules & abscesses (bumps) |
|
|
What is tinea capitis?
Px? Dx? Tx? |
Scalp
M. canis, T. tonsurans; severe: favus (T. schoenleini); kerion (tumor-like granuloma) Sx/Px: spreads peripherally, forming patches with broken hair stumps Ectothrix – outside hair shaft – anthropophilic, geophilic, zoophilic fungi Endothrix – inside hair shaft – anthropophilic fungi only – more difficult to treat Dx: microsporum fluoresces BRIGHT green, trichophyton fluoresces DULL green Tx: oral griseofulvin |
|
|
What is tinea manuum?
Px? Dx? Tx? |
Hands, associated with tinea pedis
T. rubrum Tx: oral antifungal |
|
|
What is tinea unguium?
Px? Dx? Tx? |
Nails
T. rubrum (most common), T. mentagrophytes, E. floccosum Onychomycosis – fungal infection of the nails Paraonychomycosis – fungal infection of nail bed (Candida can mimic these sx, more yellow) Tx: Oral systematic anti-fungal drugs – fluconazole, itraconazole, terbinafine PinPoint laser Most resistant to treatment |
|
|
What is fusariosis?
|
Cutaneous infections caused by Fusarium solani, Fusarium oxysporum
Disseminated in immunocompromised --> death Tx with voriconazole |
|
|
What is erythrasma?
|
~ tinea cruris, due to Corynebacterium minitussimum
Wood's light = coral red Tx with erythromycin |
|
|
What are the endemic mycoses?
Describe their structure and morphology. |
Dimorphic.
Histoplasma: hyphae/mycelia in environment, budding yeast in host Blastomyces: hyphae/mycelia in environment, budding yeast in host Cocci: hyphae/mycelia in environment, large endosporulating spherule in host |
|
|
What are the routes of infection for endemic mycoses? Who do they affect, typically?
|
Most common: respiratory
Sites of implantation (e.g., skin prick) --> cutaneous lesions Dissemination: meningitis, bone lytic granulomas, skin granulomas, other organs True pathogen of immunocompromised individuals |
|
|
Histoplasma capsulatum, structure/morphology.
|
Most common fungal infection in the world
Found in bird/bat droppings Environment: Multinucleated, branched hyphae; micro & macro conidia Host: 15-18 hours conversion to uni-nucleated oval budding yeast |
|
|
Histoplasma capsulatum, infection.
|
Microconidia inhalation --> bind CD2/CD18 integrins on macrophages --> engulfed into phagolysosome --> microconidia secrete CATALASE to interfere with lysosomal enzyme activation --> converts to yeast form --> replicates --> secretes Ca2+ BINDING PROTEIN --> Cellular immunity develops within 2 weeks to control infection (CD4+ cells) --> Secrete cytokines (IFN-γ) --> macrophages activated to a fungistatic state --> Caseating and/or noncaseating granulomas
|
|
|
Histoplasma capsulatum, most frequent result of infection.
|
Non-specific flu-like syndrome.
o fever, chest pain, dry/non-productive cough, headache, joint/muscle pain o Sx occur 10 DAYS after exposure o Resolution does not indicate eradication --> latent (inactive) infection occurs |
|
|
Histoplasma capsulatum, severe infections.
|
Less than 5% of cases
Pulmonary: coin lesions, caseating necrotic granulomas Acute pericarditis Dissemination Ocular histoplasmosis syndrome Cutaneous Fibrosing mediastinitis Severe histoplasmosis = HIV/AIDS |
|
|
Histoplasma capsulatum, dx & tx.
|
Dx: biopsy, serological Abs, PAS/GMS staining
Dx: histoplasmin skin-test immunological reactivity > 85% Tx: Antifungals used as therapeutic adjunct, itraconazole, amphotericin B |
|
Blastomyces dermatitidis aka Chicago Disease, Gilchrist’s Disease
|
Environment – uninucleate hyphae, microconidia
Host – multinucleate large budding yeast with broad bud neck |
|
|
Blastomyces dermatitidis, infection.
|
Inhalation of microconidia --> Transform at body temperature to yeast --> WI-1 surface protein binds to host macrophage integrins --> 4-6 week incubation after exposure --> BAD1 cell-wall protein – prevents complement C3 deposition onto yeast cells
Clinical infections – lobar or segmented pneumonias Trauma --> deep cutaneous infection |
|
|
Blastomyces dermatitidis, clinical syndromes & tx.
|
Benign and self-limiting infection
Chronic granulomatous and suppurative mycosis o Primary infection initiated in lungs o Pulmonary Blasto lesions rarely caseate or calcify Extra-pulmonary infections o Cutaneous infections (20-40%) – subcutaneous nodule or papule --> progress to a pustule --> irregular ulcer with wart-like elevations. Painless lesions o Bone (10-25%); urogenital tract (5-15%); CNS (5%) o Blastomycosis may occur coincident with bronchogenic carcinoma, Histoplasmosis, Tuberculosis, or other severe pulmonary disease Latent Infection/Reactivation – seems to be rare Antifungal Drug Therapy – itraconazole or amphotericin B |
|
|
Coccidioides immitis (CA San Joaquin Valley)
Coccidioides posadasii (SW, New Mexico) |
Most virulent fungal pathogen
Occupational – construction, ranchers, agriculture, archeologists Ethnic – dark-skinned populations Pregnant women are at high risk during 3rd trimester Depresses cellular Immunity – lymphoma, HIV/AIDS, transplants, high-dose corticosteroids --> higher likelihood of disseminated disease 3rd most common Opportunistic pathogen of AIDS (behind Pneumocystis, Cryptococcus) |
|
Cocci, structure.
|
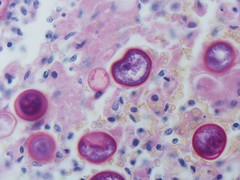
In host, spherules packed with endospores.
Environment, septate multicellular hyphae & arthroconidia |
|
|
Cocci, infection.
|
Acquisition by the respiratory route --> Conversion within 72 hours into large spherules containing numerous small endospores --> Spherule ruptures releasing endospores --> enlarge, internal septation to form new endospores
Immune system: Humoral immunity – IgM followed by IgG Cell-mediated immunity – key factor in determining recovery Pyogenic infection develops --> granulomatous respiratory infection Caseation without calcification may occur |
|
|
Cocci, clinical syndromes.
|
60% asymptomatic
Symptomatic: - Mild flu-like syndrome – fever, cough, headaches, rash, myalgias (devo 7-21 d post-exposure) - Acute severe pneumonia – cough, fever, chest pain - erythema nodosum - granulomatous inflammation with caseous necrosis |
|
|
Cocci, dx.
|

X-ray films: Sharply circumscribed pulmonary nodule – usually non-calcified, Patchy bronchopneumonia, Pleural effusion (hilar adenopathy is common)
Coccidioides Spherical Stains – Periodic Acid-Schiff (PAS); KOH + Calcofluor; Methenamine Silver Stain Coccidiodin hypersensitivity skin test |
|
|
Cocci, tx.
|
95% of acute episodes resolve without therapy (treat with bed rest)
Severe pulmonary and disseminated disease – tx Itraconazole or fluconazole |

