![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
278 Cards in this Set
- Front
- Back
|
The group fungi include what organisms?
|
• Yeasts
• Molds • Mushrooms |
|
|
What are aflatoxins?
|
naturally occurring mycotoxins that are produced by many species of Aspergillus
One of the strongest carcinogens known |
|
|
What is the significance of ergot alkaloids?
|
They come from moldy grains and rye and can cause severe health issues. they are a type of mycotoxicosis
|
|
|
What does it mean for a fungi to be opportunisitc?
|
It means they result from a secondary infection.
|
|
|
What patients are most suseptible to opportunisitc mycoses?
|
cancer (leukemia, lymphoma)
transplant AIDS autoimmune (lupus, arthritis) diabetes long-term hospital |
|
|
What risk factors increase mycoses?
|
broad spectrum antibiotics
radiation chemotherapy corticosteroids surgery catheterization Hormones |
|
|
What mycoses colonized quickly after birth can become opportunistic if not heald in check by the body?
|
Candida albicans (thrush or cheilitis)
Pityrosporum ovaled (druff-producing microbe) |
|
|
What is Cheilitis?
|
is a medical condition involving inflammation of the lip
Often seen with oral candidiasis patietns |
|
|
What is an example of a primary fungal pathogen? (they aren't vary common)
|
Coccidiomycosis
Most considered environmental |
|
|
Are fungi eukaryote of prokaryotes? What other cellular features do they have?
|
Eukaryotes
Contains erogosterol and zymosterol (in cell membrane) Cell wall with chitin, glycan and mannin (but no peptidoglycan) |
|
|
What is Thermal dimorphic conversion?
|
The ability of some fungi to grow as yeast at 37*C but as a mold at 25*C.
|
|
|
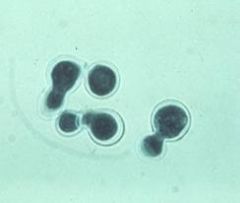
How do yeast reproduce? What is their structure?
|
(1) Single oval to round cell that buds to reproduce.
(2) Pseudohypha or an elongated yeast cell. |
|
|
What is a germ tube?
|
(1) Elongated appendage (ie, hypha) growing from a yeast cell.
(2) Virulence factor that has adhesive and invasion functions. |
|
|
What is the structure of mold?
|
Multicellular filamentous colony with potential for hyphae
|
|
|
What is a hypha?
|
long filament or strand of cells, which are often defined by
septa |
|
|
What organisms are classically know to have hyphe? Which do not?
|
Aspergillus is septate hyphe, Rhizopus and Mucor are not hyphe-nated
|
|
|
What is the name for a mat of hyphae?
|
Mycelium
|
|
|
What yeast is know to be polysaccharide encapsulated?
|
Crypyococcus neophormins
|
|
|
What is the significance of a germ tube?
|
It adds virulemce bby its adherence qualities and it also has proteases which penetrate surfaces (tissues) making it hard to get rid of. can be used to identify candida
|
|
|
Where do you see the following structures: germ tube
pseudohypha? |
Yeast! A budding structure
|
|
|
Where do you see the features: mycelium
hypha septum sporangiophore sporangium sporangiospore conidiophore conidia? |
In MOLD
|
|
|
What are the two asexual spore types?
|
Sporangiospore
Conidium (Conidiospore) |
|
|
Describe a Sporangiospore
|
Sporangium is the sack that the sporangiospores are held in. Like ballons in a bag that sits on a stalk
|
|
|
Describe a Conidium (Conidiospore)
|
Conidiophore: hyphal branch that bears conidia. Not in a "bag" like the sporingiospores. Tree like branching: Hypha to condidophore to phialide to conidium
|
|
|
What fungi produce conidiospores?
|
Penicillium and Aspergillus
|
|
|
What is the appearance of athroconidium?
|
Fragmented hypha of jointed spores
ex: ringworms, Coccidioides |
|
|
What is the appearance of a bloastoconidium?
|
it is budding
|
|
|
What does as Chlamydoconidia look like
|
It has swollen hypha
|
|
|
How does Microcondium appear?
Example: |
Unicellular
Trichophyton (dermatophyte) |
|
|
How does Macrocondium appear? Example:
|
Multicellular: Looks like a banana or fusiform shape
Microsporum (Dermatophyte) |
|
|
What two fungi are nonseptate?
|
Rhizopus, Mucor— assocaited with DM and ketoacidosis
|
|
|
What are the three fungal pathogenicity typpes?
|
granulomas,
hypersensitivities, or mycotoxicoses |
|
|
What fungus is responsible for Systemic or endemic mycoses (extremely serious)?
|
coccidioidomycosis
|
|
|
What fungi are responsible for Superficial infestations?
|
thrush and dermatophytes
|
|
|
What ate the two dermatophytes learned and their classifciation?
|
Macroconidia—Microsporum
Microconidia—Trichophyton |
|
|
What fungi are responsible for Subcutaneous mycoses?
|
sporotrichosis and mycetoma.
|
|
|
What are the main opportunisitc mycoses?
|
candidiasis and cryptococcosis.
|
|
|
What are candidias virulence attributes
|
Adherence to tissue & prosthesis (biofilms)
Form germ tubes & hyphae (tissue invasion) Extracellular enzymes (break down tissue) |
|
|
What mycoses is an Encapsulated pathogen?
|
Cryptococcus neoformans
|
|
|
What yeast could you see living inside a macrophage?
|
Histoplasma capsulatum
|
|
|
What type of respiration do most yeast use?
|
Most are obligate aerobes (some are facultative but none are anaerobes)
|
|
|
What is the difference between working with mold and yeast in the lab?
|
Yeasts can be safely handled on the bench in the laboratory but working with molds usually require an isolation safety cabinet (ie, never smell a mold culture because spores may become airborne).
|
|
|
What are the most common isolation media for fungi that do not readily support the growth of bacterial contaminants?
|
Sabouraud and potato dextrose agars
|
|
|
What are the growth rates of molds and yeasts
|
• Yeasts grow rapidly
• Molds may require weeks to mature |
|
|
What stains can be done easily on yeasts?
|
Gram stain & Chlorazol Black
(India ink & KOH) 10% KOH—direct observation |
|
|
What therapy might you use for Candida?
|
Ketoconazole-itraconazole - it inhibits ergosterol synthesis
|
|
|
what therapy might you use for systemic fungi and why?
|
amphoteracin B
Targets ergosterol, causing membrane damage |
|
|
What therapy is used for dermatophytes because it tragets micrtubules interfering with mitosis?
|
Griseofluvin
|
|
|
how does Flucytosine work
|
Interferes with DNA & protein synthesis in fungal organisms
|
|
|
What therapy for dermatophytes inhibits ergosterol synthesis and targets the cell membrane?
|
Terbinafine
|
|
|
What antifungal can be used for both candida and spergikkus that inhibits glycan synthesis (targets cell wall)?
|
Caspofungin
|
|
|
What are the most common and invasive candida species?
|
C. albicans
C. dubliniensis |
|
|
What is unique about Candida glabrata?
|
is the only species that
forms only yeast cells (not able to form pseudohyphae or hyphal structures) It is resistant to AZOLES! |
|
|
When are pseudohyphae formed?
|
produced when budding cells
fail to detach from each other |
|
|
What is a true hyphae?
|
A germ tube formed in serum and at 37*C
Seen in (C. albicans, C.dubliniensis) |
|
|
How can you distinguish between differenf species of candida?
|
Grow it on chrome argar and they grow different colors
|
|
|
eWhat are the asexual reproductive features of candidia?
|
Chlamydospores or
Blastocinidia |
|
|
What are the pathogenic factors of candida/
|
They are great attachers if they use their germ tubes!
The secreteproteases Phospholipases and heat shock proteins |
|
|
True or False: Candidiasis is communicable
|
FALSE
|
|
|
When would you see chronic mucocutaneous candidiasis?
|
With a genetic defect that impaired cellular immunity. Persons would present in early child hood and experience infections in the skin and mucous membranes
|
|
|
What areas would you test for candida based on where it can infect?
|
– Blood-systemic candidiasis
– CSF – Materials from removed catheters – Tissue samples NOT SPUTUM as it is a normal flora |
|
|
How does candidiasis stain?
|
gram positive even though they aren't really gram positive organisms
|
|
|
What newly emerging fungal pathogen is able to infect immuocompetient hosts?
|
Cryptococcus neoformans
|
|
|
What is resivoir for Cryptococcus neoformans?
|
Natural reservoir Soil, bird droppings
Must be inhaled |
|
|
What mycoses lives CSF?
|
Cryptococcus neoformans
It can result in meningeoencepalitis which contributes to its lethality |
|
|
What are the general gross and microscopic features of Cryptococcus neoformans?
|
mactoscopically it forms creamy mucoid colonies
microscopically it shows encapsulated |
|
|
What are the pathogenicity factors of cryptococcus neoformans?
|
Capsule
Diphenol Oxidase that forms melanin from phenol cotainging substances Its ability to grow at 37*C |
|
|
What mycoses is isolated in mixed ifections by growing it on birdseed agar?
|
CRYPTOCOCCOSIS
|
|
|
How can you distinguish between CRYPTOCOCCOSIS gatti and CRYPTOCOCCOSIS neoformans in the lab?
|
Grow them on CGB agar. Neoformans will stay yellow, gatti will turn blue
|
|
|
What is the treatment for Cryptococcosis?
|
Amphotericin B and Fluconazole (it can cross CNS!)
|
|
|
What are the risk factors and pathogenisis of Aspergillosis?
|
Immunosuppressed and DM
Spores inhaled Can contain mycotoxicosis that cans hepatocellualr and colon carcinomas |
|
|
What mycoses forms a powdery moled that produces many small cinidia that aerosilize that can cause sever allergic reactions?
|
Aspergilliosis
|
|
|
What are the microscopic features of aspergillus?
|
septate, hyaline hyphae (dichotomous branching), vesicule,
microconidia |
|
|
What are the pathogenicity factors of Aspergillus?
|
Hyphae
Phospholipase |
|
|
Describe allergic aspergillosis
|
Two Types:
1. Asthma (Type I) 2. Allergic bronchopulmonary aspergillosis (Types I, III) |
|
|
Describe An aspergilloma
|
It is a fungus ball that forms in the lungs or paranasal sinuses by conidia that enter the cavity, germinate and produce hyphae in the cavity. They must be surgically removed.
|
|
|
Besides the lungs, where else can you commonly find aspergillosis infections?
|
Otomycosis (external otitis)
Onychomycosis Eye inf. (conjunctival, corneal, intraocular) |
|
|
What is invasive aspergillosis?
|
FATAL IF UNTREATED
Starts in the heart and disseminates to GI, brain, liver, kidney, skin and eye. |
|
|
What is the best way to diagnose Aspergillosis?
|
Sputum or tissue samples
|
|
|
What are the treatments for
Allergic Aspergillioma Superficial and Invasive Aspergilliosis infections? |
Allergic: Steroids
Aspergillioma: surgery and amphotericin B Superficial: Nystatin Invasive Aspergilliosis: Dibridnment and posaconazole |
|
|
What is the main cause of Pneumocystic Pneumonia? What is the resivoir?
|
Pheumocyctis jirovechi
No know resivoir |
|
|
What are the 2 morphologies of Pneumocystis jiroveci?
|
– Trophozoite (Thin walled)
– Cysts (Sphericules with thiick wall that is multinucleated) |
|
|
Describe the life cycle of pneumocystis jiroveci
|
1) Mature cyst has 8 intracyystic bodies
2) Cyst ruptures releasing the bodies 3) Bodies develop into trophozoites 4) Trophozoites divide 5) Each trophozoites develop into a mature cyst |
|
|
What are the sx of Pneumocystis Pneumonia?
|
– Fever
– Non-productive cough – Shortness of breath – Weight loss – Night sweats – CXR shows diffuse bilateral infiltrates |
|
|
Is pneumocystis pneumonia communicable?
|
Yes, we think so
|
|
|
how do you make a dx od PCP?
|
CXR shows widespread infiltrated
Can finf in lung biopsy and sputum |
|
|
What is the tx for PCP
|
TMP-SMZ (Trimethoprim-Sulfamethoxazole)
and possible steroids for inflammation |
|
|
When does PCP show disease?
|
When humoral and cell mediated immunity fails
|
|
|
Where is Coccidioidomycosis seen regionally? Where is it found?
|
Southwest USA - in Soil
|
|
|
Coccidioides immitis is known by what other names?
|
Valley fever
San Juaquin Valley fever and "the great imitator" |
|
|
What is the morphology of Coccidioides immiti?
|
• Dimorphic spherule and mold
• Spherule w/ endospores • Arthroconidium |
|
|
How does Coccidioides immitis look cultured?
|
• White, gray, or brown colony
• Powdery or wooly colony |
|
|
Waht two antigenic factors can be usedul for immunodiagnosis of coccidiodes?
|
Coccidioidin
Spherulin |
|
|
Describe the pathogenicity of coccidioides imitis
|
Primay pulmonary involvement, but can look like flu or pneumonia
persons can be asymptomatic most infections are self limited |
|
|
What is the phase like manner coccidioises crosses though after inhilation?
|
Upon inhalation, the arthroconidia are transformed into
pulmonary spherules (contain endospores). Endospores are released from spherules, and then, endospores produce new spherules. Septate hyphae and arthroconidia are sometimes associated with the spherules in the pulmonary cavities. |
|
|
What is Erythema Nodosum?
|
Allergic response that is marked by tender red cutaneous nodules. Delayed hypersensitivit that develops abotu 1 month after coccidiodes immitans infection. Indicator of a good prognosis because the cell-
mediated immunity is functional. |
|
|
How is Coccidioides spread?
|
Not communicable (ie, no person-to-person transmission).
Airborne transmission |
|
|
What does it mean to have Disseminated coccidioidomycosis?
|
systemic infection in which 15-20% of people develop skin lesions
|
|
|
Waht groups are at greater risk forDisseminated
Coccidioidomycosis |
American Indians, Asians,
African Americans, & Hispanics Preggers Immunodificient |
|
|
What is the best way to identify Coccidioides immitis?
|
• KOH for fresh samples (Athrocondia culture)
• PAS for fixed tissue (pathology lab) • Microscopic – spherical form • Culture – mold 25°C • Caution – arthrospores • IgM/IgG to coccidioidin/spherulin |
|
|
What is the treatment for Coccidioides immitis?
|
• DOC – fluconazole or amphotericin B (IV for months in priary or disseminated)
Supportive care |
|
|
What is the best way to control Coccidioides immitis?
|
• Dust protection
• Pave roads • Plant vegetation • No vaccine available :( |
|
|
What is the morphology of Histoplasma capsulatum?
|
Dimorphic:
Yeast is Uninucleate budding cells Mold is Microconidium and also shows Tuberculate macroconidium. Microconidium (infective stage) Mold is White or brown cottony colony that is Slow growing – up to 12 wk |
|
|
What is the antigen for immunodiagnosis for Histoplasma capsulatum
|
Histoplasmin
Produced in broth in which mycelium grows |
|
|
What it the pathogenicity/phases that Histoplasmin goes through once inhaled?
|
Inhaled microconidia convert to a yeast cells. Yeast cells may be phagocytosed by alveolar macrophages and transported deeper into the body.
Often described as an intracellular mycosis of the reticulo-endothelial system. |
|
|
What are the virulence factors of Histoplasma/
|
Yeast releases urease to raise pH
Interferes w/ phagolysosome killing activity of phagolysosome |
|
|
Where is Histoplasma capsulatum seen most frequently regionally?
|
Ohio & Mississippi River Valleys
|
|
|
What is the best way to ID Histoplasma capslatum?
|
• Microscopic – intracellular yeast
• Isolation – site of infection • Serologic – latex agglutination |
|
|
What is the DOC for Histoplasma capslatum?
|
DOC – itraconazole or amphotericin B
• Supportive |
|
|
What is the best way to control Histoplasma capslatum?
|
• Dust protection
• Formaldehyde soil spraying |
|
|
What mycosis is known for its lung and cutaneous granuloma formation
|
Blastomyces dermatitidis
|
|
|
What is the morphology of Blastomyces dermatitidis in tissue or exudate?
|
it appears as a multinucleate, budding cell (1 broad-based bud each cell).
|
|
|
What is the morphology of Blastomyces dermatitidis in culture?
|
hyphae bear conidia
Production of chlamydospores is possible. |
|
|
How does one get infected with Blastomyces dermatitidis?
|
inhaling the microconidia soil
|
|
|
What is the best way to diagnose Blastomyces dermatitidis?
|
Direct microscopic examination: wet mount may show
broadly attached buds on thick walled cells (KOH smear of sputum, pus, exudate, urine, skin, and biopsy material). |
|
|
What is the DOC for Blastomyces dermatitidis?
|
DOC: itraconazole or amphotericin B.
|
|
|
Where is Paracoccidioides brasiliensis prevalent?
|
Predominant systemic mycosis in Latin America
|
|
|
What does Paracoccidioides brasiliensis look like??
|
Dimorphic.
Resembles B dermatitidis. Yeast is characterized with thick walls and multiple buds. |
|
|
Cultures of Paracoccidioides brasiliensis at 25°C produce?
|
conidia and chlamydospores.
|
|
|
What it the pathogenicity of Paracoccidioides brasiliensis?
|
Basically a chronic, granulomatous disease that begins in
the lungs (infective stage is inhaled) but is usually benign and self-limited in the young. Can disseminate |
|
|
What is the virulence factor of Paracoccidioides brasiliensis?
|
Virulence factor: cell wall α-glucan stimulates granulomas.
|
|
|
How is Paracoccidioides brasiliensis transmitted and what is the resivoir?
|
Not communicable (transmission is airborne) hides out in soil
|
|
|
What is the DOC for Paracoccidioides brasiliensis
|
DOC: itraconazole or amphotericin B for up to2 years
|
|
|
What are dental caries caused by?
|
Localized destruction of the teeth due to ACIDS produced during bacterial
fermentation of carbohydrates |
|
|
A high incidence of caries is associated with?
|
High carb intake
low SES Meth use (causes dry mouth) |
|
|
Describe Early Childhood Caries
(Baby Bottle Tooth Decay) |
Predominantly affects the front
teeth Repeated ingestion of sweetened liquids sugar sticks to teeth |
|
|
What Plaque Microorganisms is blamed as being an initiator of caries? Why?
|
Streptococcus mutans
It has Glucosyltransferase which changes sugar to glucan which sticks strongly to teeth |
|
|
How does Lactobacillis contribute to caries
|
Small part of normal flora (~1%) but when the ph is reduced by s. mutans it is able to grow even better.
Know PROGRESSOR of caries |
|
|
What is the role of Actinomyces viscosus in dental disease.
|
Role is still unclear, but currently
implicated in root surface caries |
|
|
How does lactobacillis gram stain?
|
Postive as do many of the other dental caries related bacteria
|
|
|
What bacteria that is part of the normal mouth flora is anticarigonetic?
|
Veillonella spp.
it RAISES pH in the mouth |
|
|
What is the most cariogenic sugar?
|
Sucrose
It is what s. mutans uses |
|
|
What is the progression of tooth decay?
|
White spot which is first sign of
demineralization Sticky lesion Demineralization Fracture |
|
|
What four factors must come to together for caries to form?
|
Microorganism
Diet Host Factors Time |
|
|
What two organisms can be used to measure/diagnose caries?
|
S. mutans
Lactobacillus spp. |
|
|
What are the new preventative treatments for dental caries and what bug are they direct for?
|
– Vaccination against dental caries
– Passive immunization – Replacement therapy (probiotic therapy) Directed at s. mutans |
|
|
What are the stages of periodontal disease?
|
Healthy
Gingivitis/Periodontitis Advanced Periodontitis |
|
|
What is the morphology of the flora in a healthy mouth?
|
Mainly gram + cocci with few
spirochetes or motile rods Predominantly facultative |
|
|
What is the morphology of the flora in a mouth with Chronic gingivitis?
|
About 55% of the cells are gram + with
occasional spirochetes and motile rods |
|
|
What is the morphology of the flora in a mouth with Chronic periodontitis?
|
About 75% are gram –
90% are strict anaerobes Motile rods and spirochetes present |
|
|
What is the morphology of the flora in a mouth with aggressive periodontitis?
|
About 65-75% are gram – bacilli. Few spirochetes or motile rods are present.
May be associated with cellular immune or genetic defects |
|
|
Describe Chronic gingivitis
|
Inflammatory response limited to the marginal gingiva without bone loss or deep periodontal pockets
_REVERSIBLE _Halitosis Patients asymptomatic |
|
|
What specific organism changes do you see in ginigivits?
|
Increase in Actinomyces (+),
Capnocytophaga (-), gram – obligate anaerobes |
|
|
What specific bug changes do you see in Periodontitis?
|
Increase in
Porphyromonas gingivalis (-) and Prevotella intermedia (-) |
|
|
What is Periodontitis?
|
Progression of gingivitis to include loss of collagen attachment to the tooth and bone, loss of bone, and to deep periodontal pockets
– Cause of most tooth loss in adults |
|
|
What are the two types of Periodontitis?
|
Chronic periodontitis (95%_
Aggressive periodontitis (rare, may be inherited) |
|
|
What percentage of adults have periodontitis?
|
70-80% of adults
|
|
|
What is Porphyromonas gingivalis associated with?
|
Chronic Periodontitis
|
|
|
how does Porphyromonas gingivalis look stained and what does it need to grow>
|
• Gram negative coccobacilli
• Black-pigmented anaerobe Requires hemin to porphyrin pigment vitamin K and peptides |
|
|
What are the virulence factors of Porphyromonas gingivalis?
|
Fimbriae
Hemagglutinins Hemolysins Proteases Polysaccharide capsule (K antigen) Outer membrane vesicles |
|
|
What is the respiration of Porphyromonas gingivalis?
|
anaerobe
|
|
|
What are the organisms of Chronic periodontitis? (4)
|
Porphyromonas gingivalis
Prevotella intermedia Tannerella forsythia Capnocytophaga spp. |
|
|
What treatment may be necessary for patients with chronic periodontitis?
|
– Removal of plaque by scaling or planing
– Surgical removal of inflamed tissue Antimicrobial agents like: – Mouthwashes – Antibiotics |
|
|
When do you see Aggressive periodontitis?
|
Teens usually present and more females than males. genetic/autoammunte component
|
|
|
Aggressive periodontitis usually presents how?
|
– Associated with bone loss around teeth
Often does NOT present with inflammation, bleeding, or plaque accumulation |
|
|
Aggregatibacter actinomycetemcomitans is associated with what disease?
|
Aggressive periodontitis
Looks like a star fish |
|
|
What is another name for Acute Necrotizing Ulcerating Gingivitis (ANUG)?
|
Trench Mouth
|
|
|
How does (Acute) Necrotizing Ulcerating Gingivitis present?
|
– Gingivae that are red, inflamed, shiny, bleeding, with ulcers
– Lesions are painful and covered by a pseudomembrane – Halitosis – Patient may notice a metallic taste – Usually no lymph node involvement, fever, or malaise |
|
|
What bacteria contribute to trench mouth?
|
Fusobacterium nucleatum
Treponema spp. both obligate anerobes Both gram negative |
|
|
What three factors are needed to diagnose trench mouth?
|
– Fusobacteria
– Spirochetes – Leukocytes |
|
|
What is the treatment for trench mouth (ANUG)?
|
– Removal of plaque and local debridement
– Improvements in oral hygiene, use of antiseptic mouth rinses - Antibiotics |
|
|
What is Noma?
|
Cancrum oris, gangrenous stomatitis
Basically Extremely severe form of ANUG |
|
|
When/where do you see NOMA
|
– Severe malnourishment
– Recent infection, usually viral infection or TB Young kids under 10 in developing countries |
|
|
What are dentoalveolar infections?
|
Pyogenic infections of the teeth and
supporting structures |
|
|
What is Ludwig’s angina?
|
A type of dentoalveolar infection that is a swelling of the tissue at the front of the neck accompanied by fever
Bullneck appeareance Must make sure airway remains open |
|
|
What is a Periodontal abscess?
|
type of dentoalveolar
Painful! Polymicrobial infection |
|
|
What are the features of Cervicofacial Actinomycosis?
|
Associated with trauma or invasive oral procedures. Common for actinomycosis
"Lumpy jaw" Swelling is fibrosed and Pus is gritty/sand-like and contains visible, yellow granules (called “sulphur granules,” but do not contain sulphur) |
|
|
What bug causes Cervicofacial Actinomycosis?
|
Actinomyces israelii
Look grains look like teeth |
|
|
What is candicia-associated denture stomatitis?
|
Common in full-time denture wearers or other orthodontic appliances,
Erythema and edema of mucosa in contact with surface of upper denture |
|
|
What is Gentian Violet used for?
|
OTC treatment for candida
|
|
|
What is the HSV Epidemiology?
|
NO season
Humans only reservoir - fluid spread 80% have HSV1 20% have HSV2 |
|
|
What are the HSV Characteristics?
|
Linear dsDNA genome
Large, enveloped virus with an icosadeltahedral capsid Envelope contains: – Attachment proteins – Fusion proteins – Structural proteins Persistant infections in neurons Lytic infections in epithelial cells/fibroblasts |
|
|
What is a HSV finger lesion called?
|
Herpetic whitlow
Primary lesion on finger |
|
|
VZV Reactivation presents how?
|
Herpes virus (HHV-3)
May show sharp lines of demarcation, especially at midline |
|
|
Coxsackie A causes what problems?
|
Herpangina
Hand-foot-and-mouth disease Aspetic meningitis |
|
|
Coxsackie A Characteristics (morphology, genome,etc.)
|
Enterovirus—also includes poliovirus
+ssRNA genome Small, non-enveloped Icosahedral capsid Totall opposite of HSV |
|
|
What is the epidemiology of Coxackie?
|
Infections highest in the summer
Seen mainly in children Associated with areas of poor sanitation and crowding Humans are the only reservoir Spread primarily by fecal-oral route |
|
|
What virus associated with infant/childhood diarrhea?
|
rotavirus
adenovirus |
|
|
What virus associated with feces contaminated food?
|
Norovirus
|
|
|
What is the makeup of Rotaviruses?
|
ds RNA
nonenveloped, icosahedral capsid Segmented genome |
|
|
Does Rotavirus have seasonality?
|
Yes. Winter outbreaks expected in
temperate zones called “winter vomiting disease” |
|
|
How would a patient with Rotavirus present?
|
They would be an INFANT
5-7 day course of fever, vomiting, diarrhea 10-20 diarrhea episodes per day |
|
|
What is the Rotavirus Enterotoxin?
|
NSP4
It is seccteted form infected cells and binds to neighboring cells causing Ca++ to be released which stimulates secretion |
|
|
What are the ways to detect rotavirus?
|
ELISA screen for presence
of viral antigens in stool Latex agglutination test is available for type A rotaviruses |
|
|
Describe the Rotasheild vaccine
|
Live, attenuated preparation for infants administered at 2, 4, and 6 months of age from
Tetravalent |
|
|
Which rotavirus was voluntarily withdrawn from the market
|
Rotasheild due to intussusception
|
|
|
Describe the Rotarix vaccine
|
Live, attenuated monovalent G1 strain
2 doses over 2 months (~80% efficacy) |
|
|
Describe the RotaTeq Vaccine
|
Live, oral vaccine containing
5 reassortant viruses derived from human and bovine viruses – Express human virus serotype proteins G1-4 and P1A – Three doses starting at 6-12 weeks – Licensed in US |
|
|
Describe the structure of Enteric Adenoviruses
|
Double stranded DNA virus
Acid resistant capsid |
|
|
What population get Enteric Adenoviruses?
|
Endemic diarrhea of infants
Extended period 5-12 days of diarrhea, fever, and vomiting |
|
|
What are the two Caliciviruses? Where are they found?
|
Sapporovirus
Noroviruses marien environmetns |
|
|
Describe the structure of norovirus?
|
ssRNA genome
These viruses are small |
|
|
What population gets noroviruses? How does it present?
|
Older children and adults
Epidemics of diarrhea and vomiting, Typically mild and self-limited 24-48 hours Associated with food/shellfish |
|
|
Why is it difficult to trace a norovirus outbreak?
|
because not only is it transferd by food, but also many secondary cases from person to person
|
|
|
Which viruses are unculturable, and extraordinarily resistant to inactivation?
|
norovirus
|
|
|
Describe the structure os astrovirus
|
ss RNA genome, star-
shaped aspect on capsid visible by EM |
|
|
Does astrovirus have a seasonal link?
|
No
|
|
|
Where are tou most likley to see an epidemic of astovirus?
|
young children, pediatric
wards, day care centers, and nursing homes |
|
|
What is cholera?
|
Cholera -- acute diarrheal disease due to Vibrio cholerae infection.
Cauess massive morbitity and mortality |
|
|
What is the main feature of cholera?
|
Acute and massive watery diarrhea is the main feature
“Rice water” stools |
|
|
What is the cardinal sign of cholera
|
Abrupt Massive volume watery diarrhea (1 liter /hour)
|
|
|
Describe the morphology of cholera
|
• Gram negative, bent rod shaped (vibrio) bacterium
• Nonspore-former • Facultative anaerobe • Motile, polar flagellum • Classified by O (somatic) antigens |
|
|
What is the significance of Serogroup O-1 cholera?
|
It is the one seen in classic cholea epidemics - contains Biotype El Tor
(1930s pandemic) |
|
|
What is the significance of the cholera Serogroup O-139?
|
Seen in India in 1992
O-139 can cause disease in individuals who have recovered from a previous O-1 infection |
|
|
What disease is a frequent attender of disasters?
|
Cholera
|
|
|
What is interesting about how cholera colinizes?
|
The colonized mucosa shows
NO change in physical integrity |
|
|
What is choleragen?
|
Cholera toxin
Phage encoded AB toxin |
|
|
Describe the AB toxin mechanism for cholera
|
B Binds
A causes cAMP to inctrease causing hyper secretion of water and electrolytes causing the diarrhea |
|
|
Besides cholera toxin, what is the other main virulence factor?
|
toxin coregulated pilus gene product – needed for attachment to host.
|
|
|
How are cholera toxin genes aquired?
|
Lisogenic Conversion
CTX is a mobile genetic element, a filamentous virus related to M13. The CTX receptor is on the tcp gene. The ctx and tcp genes are in effect environmentally regulated |
|
|
How id cholera diagnosed
|
Direct microscopic examination of stool shows large numbers of vibro shaped bacteria that are motile
|
|
|
What strains of V. choleraemay cause diarrheal disease but not
cholera? |
O-1
|
|
|
What are some cholera suseptitbility factors
|
Type O
achlorohydria (High pH- they love acid!) |
|
|
What are the features of V. parahaemolyticus
|
, infection most common in summer
Consumption of raw or undercooked shellfish has been a recurrent source of human infection. Oxidase positive, will form green colonies on TCBS agar |
|
|
What are the features of V. vulnificus
|
frequently associated with oysters or exposure to seawater harboring oysters,
other shellfish or marine life more common when warm weather! The bacterium is a serious threat primarily to patients with underlying disease or immune compromise. |
|
|
What is the treatment of V. vulnificus?
|
Treat with tetracycline
|
|
|
Describe Shigellae morphology
|
• Gram negative rod
• Nonspore-former • Facultative anaerobe • Nonmotile (usually) • Lactose non-fermenter |
|
|
Describe Shigella clinical
|
the large bowel- Incubation 72 hours
Initial symptoms - fever, cramps, vomiting, watery diarrhea can progress to dysentary |
|
|
What allows shigella to be distinguised from e-coli?
|
It is a Lactose non-fermenter
|
|
|
What is the differnence bewteen diarrhea and dysentery?
|
dysentery is classic - blood,
mucous and PMN’s in stools, fever, cramps, tenesmus |
|
|
Describe the surface o antigen of shigellas virulence
|
Induce endocytosis into follicle-associated M (microfold) cells
Shigella will lyse phagosome and escape to cytoplasm on basolateral side allowing for cell to cell transmission |
|
|
What virulence factors does shigella have?
|
Surface O antigen
Actin binding protein (promotes movement) Shiga toxin |
|
|
Describe the shiga toxin
|
It causes Disruption of protein synthesis and damage to the intestinal epithelium
|
|
|
How do you diagnose shigelliosis
|
Microscopic examination of feces - Normal diarrhea wont have RBCs and PMNs
Culture Quickly so other species dont overgrow Look for blood tinged flecks of mucus to plate Immunoflourencesns Sigmid colon exam to look for ulcers |
|
|
What is the treatment of Shigelliosis?
|
This is a self-limiting disease
Fluid replacement Effective antibiotic therapy may shorten course, eliminate carriers (there are a lot of resistant strands though) |
|
|
What are the complications of shigella?
|
bacteremia is UNCOMMON however
Potential to become a carrier |
|
|
What is reiters syndrome
|
(urethritis, polyarthritis, inflammatory eye disease, skin lesions)
Nonspecific acute inflammatory arthritis that ranges from slight to severe Strong association with HLA B27 individuals and shigella |
|
|
What is Hemolytic uremic syndrome (HUS)
|
S. dysenteriae, type 1 infection (Shiga toxin production) but can be seen with others like ecoli and samonella that damage cells
Acute renal failure with poor prognosis |
|
|
How is shigella apread? What is the resivoir?
|
Humans
Person to person |
|
|
Does it take a lot of shegella to get sick?
|
Nope
|
|
|
What is the significance of the group types of shigella?
|
Groups A-D
A most severe. D least |
|
|
Where is Salmonella found naturally?
|
Normal gut flora of many birds and animals
|
|
|
how does Salmonella persent clinically?
|
Incubates for 12-48hrs
Sudden onset of disease - fever, chills, cramps, diarrhea, vomiting 2-3 days duration in normal host |
|
|
What host is samonella more sever in
|
infants and elderly
|
|
|
What is the morphology of Samonella
|
• Gram negative rod
• Nonspore-former • Facultative anaerobe • Motile • Lactose non-fermenter |
|
|
What is the proble with treating S. dysenteriae with antibiotics?
|
It may provoke hemolytic uremic symdrome
|
|
|
What age has the highest incidence of shigella?
|
kids 1-4
|
|
|
What are the four types of salmonella infection
|
1. Gastroenteritis
2. Bacteremia or septicemia without GI symptoms 3. Enteric fever 4. Carrier state |
|
|
What are the virulence factors of salmonella?
|
Enterotoxin
Mucosal invasion genes (enters both M and epithelial cells!) LPS Others: Resistance to serum killing Acid resistance phoPQ-controlled genes for intra-phagocyte survival Virulence plasmid factors (spv genes) |
|
|
How do you make the diagnosis for salmonella?
|
Microscopic-Fecal leukocytes
Culture FA tests Serological confirtmation |
|
|
What ate the reservoirs of salmonealla
|
Animal reservoirs
primarily Eggs Beef products and cattle Pigs and pork products Also dogs, cats, pet reptiles |
|
|
Does it take a lot of salmonella to get infected? How?
|
Yes
Usuall by contaminated food or water |
|
|
What is the hiset incidence range for salmonella
|
Infacnts and children 6 months to 5 years
|
|
|
Does salmonella have a seasonality?
|
Yes summer and fall
|
|
|
What is the best prevention of salmonella?
|
Animal reservoirs
primarily Eggs Beef products and cattle Pigs and pork products Also dogs, cats, pet reptiles |
|
|
What are the recent outbreaks from salmonella?
|
Tomatos
Alfalfa frozen rodents??? Eggs! Ground Turkey Cantaloupe |
|

What does the pink tube indicate?
|
Urease Activity
|
|
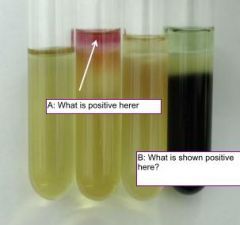
|
A: Indole Production
B: H2S Production shows as black percipitate |
|
What bugs can cause lactose fermenting as shown?
|
E-coli and Klebsellia
|
|

What is evidenced by the color change on the left? What organism from lab can do this?
|
Lactose fermentation on MacConkeys
Klebsellia and E.Colu |
|

What is being tested? Which side is positive?
|
Oxidase
the Right shows a positive result |
|
|
What does a RED slant on A TRIPLE SUGAR IRON AGAR indicate?
|
does not ferment either lactose or sucrose
|
|
|
What does a Yellow slant on A TRIPLE SUGAR IRON AGAR indicate?
|
ferments lactose and/or sucrose
|
|
|
What does a RED butt on A TRIPLE SUGAR IRON AGAR indicate?
|
no fermentation, the bacterium is an obligate aerobe
|
|
|
What does a YELLOW butt on A TRIPLE SUGAR IRON AGAR indicate?
|
some fermentation has occurred, acid has been produced, it is a facultative anaerobe.
|
|
|
What does a Black butt on A TRIPLE SUGAR IRON AGAR indicate?
|
H2S has been produced
|
|

What is know about the organism in tube a?
|
Yellow Slant: ferments lactose and/or sucrose
Wellow Butt: some fermentation has occurred, acid has been produced, it is a facultative anaerobe. It also makes gas |
|
|
What enterics make H2S?
|
Proteus and Salmonella
|
|
|
What enteric is positive for indole production?
|
E.Coli
|
|
|
What enterics are lactose non-fermenters?
|
Proteus and salmonella
|
|
|
What does the oxidase test distinguish between?
|
Enterobacteriaceae,
which are oxidase-negative, and members of the genus Pseudomonas, which are oxidase-positive. |
|
|
What is the Indole Production test looking at?
|
the ability to degrade the amino acid tryptophan to indole
E. Coli does this |
|
|
Alkaline slant (red) and alkaline butt (red) or no change (orange-red) indicates what?
|
No carbohydrate fermentation has occurred
|
|
|
What enteris are motile?
|
E. Coli, Proteus, Samonella
|
|
|
What does VPI mean?
|
Vibrio cholerae pathogenicity island
|
|
|
Where and what is the gene for the cholera toxin (CTX) virus receptor?
|
– The gene for the CTX virus receptor (tcp) is in the VPI
|
|
|
What are Two lysogenic conversions are required for cholera?
|
First converstion makes the receptor
Secondconversion makes the A-B CTX toxin that can now bind to the made receptor. This is cool because one virus is actually promoting an infection by another virus |
|
|
Scraping of a candida specimine under the microscope would show what formation?
|
Budding yeast and pseudohyphae
|
|
|
What are dermatophytes?
|
Ringworm Fungus
Microsporum & Trichophyton most common |
|
|
Which candida can from germ tubes?
|
albicans & dublinensis
(gabralta cannot!!!) |
|
|
what organism is found in bird droppings?
|
Cryptococcus neoformans
|
|
|
Cryptococcus serotypes a & d?
Cryptococcus serotypes b & c? |
neoformans
gattii |
|
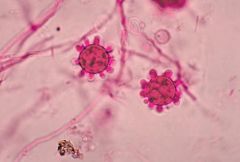
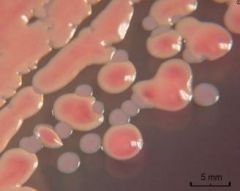
What organism is seen here?
|
histoplasma capsulatum
Classic Tuberculate macroconidium present |
|
|
Whose life cycle is illustrated?
|
Coccidioides immitis
Spherule and Athroconidia |
|
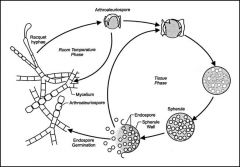
Whose life cycle is illustrated?
|
Coccidioides immitis
Spherule and Athroconidia |
|
|
What organism is associated with bat droppings?
|
Histoplasma capsulatum
|
|
What organism is shown here?
|
Blastomyces dermatitidis
note wide base and budding |
|

What organism is shown here?
|
Paracoccidioides brasiliensis
|

