![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
94 Cards in this Set
- Front
- Back
|
Zoonotic Definition
|
An INFECTIOUS disease o fLower Animals that may be Transmitted to human.. Transmission may be direct, contact, animal vectors & or by formites
|
|
|
What is the zoonotic source for
1. Measles 2. Tuberculosis 3. Small pox 4. Influenza (2) 5. Pertussis (2) 6. Faliciparum Malaria (2) |
1. Cattle (rinderprest)
2. Catitle 3. Cattle (coxpox) 4. Pigs, Ducks 5. Pigs, Dogs 6. Birds (Chickens & Ducks) |
|
|
Name the Catogory "A" Bio Warfare/Terror Agents
1. Zoonotic (4) 2. Non-Zoonotic (2) |
1. Bacillus antracis, Yersina pestis, Francisiella tularensis & Viral haemorrhagic fevers
2. Clostridium botulinum toxin & variola major |
|
|
Name the Category "B" Bio Warfare/Terror Agents that are
1. Zoonotic (3) 2. Non-Zoonotic (3) |
1. Brucella species, Burkoholderia mallei & Coxieall burnetti
2. Clostridium perfringens Epsilon toxin, Ricinus communis toxin & Staph aureus enterotoxin B |
|
|
Most common zoonotic infection in the USA
|
1. Lyme disease (Boreilla burgdoferi)
|
|
|
Rickettsiae. Bame the 2 in the
1. Thyphus group (2) 2. Spotted Fever, Group A (2) 3. Spotted Fever, Group B (2) 4. Spotted Fever, Group C (2) 5. Scrub Thyphus |
1. prowazekii & thyphus
A. rickettsi & siberica B. conori & perkeri C. akari & australis |
|
|
What causes
1. Cat Scratch disease 2. Q Fever 3. Human Erlichosis 4. Special quality for each |
1. Rochakimaea henselae (& growin in artifical cultures)
2. Coxiella burnetii (& Survives in dust) 3. Erlicha chaffeensis (& invades Human WBC) |
|
|
Rickettsial Diseases
1. Common feature (3) |
1. STEADY high fever, Severe Retoorbital headache 7 rash
|
|
|
Define the following exanthems
1. Macule 2. Papule 3. Vescile |
1. Discolorred spot, darker than surrounding skin. LEAKAGE of blood into epithelium
2. ELEVATED spot, d/t INFLAMMATION. 3. Elevated small BLISTER. Surrounded by INFLAMED skin & loaded w/ INFECTIOUS material |
|
|
Define the following exanthems
1. Vesicle 2. Pustule 3. Crust |
1. Elevated small BLISTER. Surrounded by INFLAMED skin & loaded w/ INFECTIOUS material
2. Same as Vesicle, but filled with PUS (normally infectious) 3. DRIED, partially healed pustule. Infections organism (semi dormant) |
|
|
Rickettsia prowazekii
0. Causes 1. Primary Reservoie 2. Transmission via (2) 3, Secondary Reservoir & related vectors (2) |
1. Man
2. Body louse → Pediculus corporis/humanis & Crab louse → Pthirus pubis 3. Sheep, Cattle & Goats → Ambyloma (ticks) 4. Wild flying squirrel → Lice & Flies |
|
|
Pediculus corporis/humanis
1. Vector type 2. Perferred tempertatuere? Results in? 3. Attracted by (2) 4. Avoids parts of body 5. Prefers what clothing 6. Insect population in infected huma |
1. Human body louse (ectroparasite of Man)
2. 29⁰c -30⁰c. Leaves host once has fever 3. Odor & Own feces 4. Moisture 5. ROUGH surfaces 6. 10-20 instects |
|
|
Effects of R. prowazekii on Pediculus sp. vector
1. Louse infection (4) 2. Mean survival rate |
1.Midgut → Multiply in epithelial cells→Tissue destroyed & Lysed → Reelaces in to faeces
2. 10 days after infection |
|
|
R. prowazekii → Epidemic Thyphus
1. Incubation 2. Rash 3. Symptoms (2) 4. Complications (3) 5. Inoculation can also occur |
1. 7-14 dats afer bite
2. Centrifugal maculopapular rash 3. Rickettsial headache & STEADY high fever 4. Myocarditis, vascular collapse & CNS dysfunction 5. By swatting the Louse into your skin |
|
|
Epdimeci Thyphus
1. Diagnosis 2. Therapy (2) 3. Reach detectable levels |
1. Serological (retrospective)
2. Straight away, based on history & presentation 3. 6-8 weeks post infection |
|
|
Epidemic thyphus.. Prognosis
1. ↑ Fatality rate 2. Untreated fatality rate is % 3. ↑ Risk of mortality |
1. Delay of correct therapy in 2nd week of illness
2. 25% 3. Manutrition, Stress or Secondary Infection |
|
|
Rickettsia rickettsii
0. Causes 1. Region Tick responsible 2. Western states 3. Eastern States 4. Southwest 5. Name the 3 reservoirs |
0. RMSF (Rocky Mountain Spotted Fever)
1. Appalachian Mts (Gerogia, Oklahoma, Arkansas & Text) 2. Dermacentor adnersonii → Wood Tick 3. Dermacentor variabilis → Dog Tick 4. Ambylomma americnaum → Lone Star Tick 5. Dogs, Wild Rodents & Tick itself (trans-ovarial) |
|
|
RMSF
1. Incubation 2. Rash Type 3. Rash appears 4. Symptoms (5) 5. Complications (6) |
1. 2-6days
2. CentriPEDAL, Maculopapular, starting at palms & soles 3. 2nd or 3rd day 4. Rickettsial FEVER, Headache, Toxicity, Mental Confusion & Myalgia 5. DIC, Thrombocytopenia, Encephalitis, Vascular Collapse, Renal or Heart Faiulre |
|
|
RMSF
1. Diagnosis 2. Serology 3. Treatment 4. Contraindicated |
1. History & Symptoms
2. Retrospective 3. Straight away (Teracycline & Chloramphenicol) 4. SULFONAMIDES |
|
|
Coxiella burnetti
1. causes 2. Multiplies in 3. Prefers 4. Unique characteristic 5. Reservoir animals (2) |
1. Q Fever
2. Phagolysome 3. Low pH 4. Dry dust @ 40°C 5. Cattle Sheep & Goats |
|
|
Coxiella burnetii
1. Primary Exposure via 2. Secondary route (2) 3. Most human infections are 4. Geo Epi |
1. Inhalation of Dust
2. Ingestion of contaminated Meat or Dairy 3. In apparent symptoms (walking pneumoniae) 4. Hiking in the desert. Arid (dry) South West |
|
|
Coxiella burnetii
1. Incubation period 2. Rash 3. Symptoms (4) 4. Complications are (3) |
1. 7-21 dAYS
2. ABSENT 3. Fever, Chills, "usual" headache, Mild Dry Persistent Cough & Patchy interstitial pneumoniae 4. Endocarditis, Encephalitis & VERY RARE fatalities |
|
|
Coxiella burnetii
1. Diagnosis 2. Treatment (2) |
1. Retrospective
2. Supportive care, although most will resolve retrospectively |
|
|
Erlichosis canis & chafeensis
0. Goegraphy 1. Resembles 2. Causes 3 Transmitted by 4. Symptoms (2) 5. Severe cases (3) 6. Complications (3) |
0. Appalachian region
1. RMSF 2. Human Granulocytic Ehrlichiosis 3. Brown Dog Tick 4. Fever & GI abnormalities 5. Cough, Diarrhea & Lymphadenopathy 6. Respiratory & Renal Insufficiency & CNS abnormalities |
|
|
Anaplasma phagocytophilum
1. Causes what disease 2. Vector 3. In Host, targets (2) 4. Infection leads to 5. Geography |
1. Human Granulocytic Ehrlichiosis
2. Ticks 3. Neutrophils & Macrophages 4. Compromised immune system 5. Great lakes & COASTLINE of North East |
|
|
Psittacosis
0. Other name 1. Caused by 2. Reservoir 3. Main Symptom 4. Bacteria shed via (2) 5. Unique, sheddings can? |
0. Parrot Fever
1. Chlamydophila psattaci 2. Pet Birds 3. SEVERE pneumoniae 4. Feces & Nasal Discharges (Both in Bird) 5. Remain infectious for several months |
|
|
Cat scratch disease
1. Caused by (2) 2. 3-10 days later 3. 2-3 weeks later 4. Persistant for 5. Couse |
1. Rochalimaea (Bartonella) henselae 90% & Afipa felis
2. Papule/Pustule appears at site of scratch, then heals spontaneously 3. Regional lympadenopathy (HEAD, NECK & AXILLA) 4. 2-4 months 5. Self Limitng |
|
|
Rochalimae (bartonella) henselae
1. Also causes 2. Infections observed in 3. Symptoms 4. Other site |
1. Bacillary Angiomatosis
2.HIV patients 3. "Cranberry nodules" , multiple subcutaneous red papule. 4. Visceral |
|
|
Bacillus anthracis
1. Type of Bacteria 2. Reservoir 3. Spread by 4. In order for transmission, requires 5. On culture (3) |
1. Gram POSITVE rod
2. Hoofed & Grazing Animals 3. Grass 4. Death of organism 5. Long chain, with endospores on vegetative cells |
|
|
Bacillus anthracis
1. Type of bacteria 2. Pathogen 3. On culture 4. Spore? Motile? Hemolytic? 5. Type of capsuel |
1 Large, Strong Gram +ve
2. Facultative Anaerobe 3. Rods in Chains 4. Heat resistant Endospore, No & No 5. Glutamyl polypeptide |
|
|
Bacillus anthracis
1. Name the three virulence factors & roles |
1. Lethal factor → Tissue Necrosis
2. Edema Factor → Infiltration & Tissue Sweeling. Enhances distribution of Lethal Factor 3. Protective antigen → Carries the TWO factors (separately) across Cell membrane |
|
|
B. antracis
1. Name THREE manifestations & symptoms |
1. Cutaneous → Molst common, least fatal
2. Gastrointestinal → Rare in humans, high mortality. Most common in Animals 3. Pulmonary→ Highest mortality |
|
|
Cutaneous Anthrax
1. Primary infection as 2. Progresses to 3. Ends 4. Other symptoms (3_ 5. Incubation |
1. Papule
2. Vesicular Stage 3. ESCHAR (necrotic ulcer) 4. Edema, Redness & Necrosis w/o Ulcer 5. 1-12 days |
|
|
Cutaneous Anthrax
1. Diagnosis (3) 2. Blood Culture 3. Biopsy for Immunochemistry if |
1. Gram stain, PCR or Culture→VESCIULAR fluid, EXUDAGE or ESCHAR material
2. Retropsective 3. If taking antimicrobials |
|
|
Gastrointestinal Anthrax
1. Symptoms (3) 2. Followed by (2) 3. Other sites (3) 4. Develops after 5. Incubation 6. Fatality |
1. Abdominal Distress, Bloody Vomiting & Diarrhea
2. Fever & Septecemia 3. Oropharyngeal Ulcerations w/ Cervical adenopathy & Fever 4. Ingestion of poorly cooked meat 5.1-7days 6. 25-60% |
|
|
Inhalation Antrax
1. Initial 2. Followed by (2) 3. Complications (2) 4. Incubation 5. Fatality w/ AB treatment 6. W/O |
1. Flu-like prodrome symptoms
2. Hypoxia & Dyspnea 3. Meningitis (50%) & Rinorrhea 4. 1-7 days (rare up to 42) 5. 97% 6. 75% |
|
|
Inhalation Antrax Diagnosis
1. Chrest X-ray (4) 2. Immunochemistry with 3. Fluid for (3) |
1. Wiidened MEDIASTINUM, Pleural effusions, Infilitrates & Pulmonary CONGESTION
2. Affected tissue biopsy & Pleural flud cell block 3. Gram stain, PCR & Culture |
|
|
Name the Brucella species related to
1. Cattle 2. Goats 3. Swine Name the gram negative rods related to 4. Rodents 5. Rabbits 6. Cats, Dogs & Horses 7. Cattle & Horses |
1. B. abortus
2. B. melitensis 3. B. suis 4. Yersina pestis 5. Francisiella tularensis 6. Pasteurella multicoda 7. Burkholderia mallei |
|
|
B. spcies
1. Bacteria type 2. Pathogen type 3. Spore, Motie, Capsule 4. Unique feature 5. Nutritionally fastiduous (3) |
1. Gram negative Cocco-bacilli
2. Strict Aerobe (Facultative) 3. No, No, & Small Capsule 4. 2 chromosomes of unequal size, both needed for survival 5. Complex media, Capneic & Slow Growing |
|
|
Brucella soecies
1. In reservoirs 2. Patients normally (2) 3. Transmission via (4) 4. Organism killed by |
1. Venereal disease of Farm Animals
2. Butchers or Vets 3. Skin breaks, Mucous membranes, aerosols & dairy products 4. Pasteurization |
|
|
1. Brucella abortus reservoir
2. Brucella melitensis? 3. Brucella suis |
1. Cattle
2. Goats 3. Swine |
|
|
Brucella sp. Pathogenesis
1. Three steps 2. Only control 3. Failure of control leads (3 Steps) |
Penetrates Skins/Mucous Membranes → Carried to Lymphatics by PMS → MULTIPLY in PMNs
2. T Cell response 3. Bacterial Multiplication w./in RES → Waves of bacteria released → Reccuremnt Bacteremia |
|
|
Brucellosis
1. Incubation 2. Onset of symptoms 3. Present normally in 4. What may perist for months → Years 5. May present with (2) |
1. 7 → 21 days
2. Drencking Sweat w/ High Fever 3. Afternoon or Evening 4. Nocturnal Fever 5. Arthritis, Orchitis or HEPATOMEGALY |
|
|
Brucellosis
1. Definitive diagnosis (2)? 2. Specimen (4) 3. Special consideration for B. abortus (cattle) 4. Incubation |
1. Isolation & Culture
2. LYMPH node, Blood, Bone Marrow & Liver 3. Incubate in C02, then use blood agar 4. 2-4 weeks |
|
|
Brucellosis
1. Therapy 2. Issue 3. Treatment muse be 4. Relapses occur |
1. Chemotherapy
2. Slow results 3. Prolonged 4. up to 3 months |
|
|
Francisiella tularensis
1. Bacteria 2. Pathogen 3. Spore, Motile, Capsule 4. Fastiduous requires 5. Agar 6. Growth time on Agar |
1. Gram -ve Coccobacillus
2. Facultatitve 3. No 4. SULFYHYDRYL compounds 5. Cysteine-Glucose Blood agar (aerobic) 6. 2-10 days |
|
|
Francisiella tularensis
1. Reservoir (4) 2. Vectors (3) 3. Geography 4. Seasonality |
1. RABBITS, squirrels, muskrats & deer
2. Deer Flies, Ticks: Dermacentor sp. & Ixiodes sp. 3. North America, Canada & Mexico 4. Late Spring |
|
|
Francisiella tularensis
1. Entry via (3)? Which has highest mortality 2. Minimum infectios dose 3. Bactermic spread → (3) 4. If injected, what develops 5. Recovers confers 6. Patient History |
1. Inhalation (MOST severe) or Injection (LEAST)
2. <100 cells 3. Infects RES → Granuloma formation 4. Ulcer at injection site 5. Long lasting story 6. Random story involving rabbbits |
|
|
Francisiella tularensis
1. Incubation 2. Onset (3) 3. If Injection 4. Ingestion 5. Inhalation 6. All 3 progress to |
1. 2-5 days
2. ACUTE fever: Fever, Chills & Mailaise 3. Ulcero-Glandular formation 4. Thypodial 5. Pneumoniae (greatest mortality) 6. Systemic Infection |
|
|
Francisiella tularensis
1. Diagnosis Pasturella multicoda 2. Diagnosis 3. Difference in symptoms |
1. Fluroscent Anti-body along with careful history
2. Culture for apirated pus 3. DOES NOT become systemic |
|
|
Pasteurella multicoda
1. Type of bacteria 2. Pathogen 3. Ferments 4.Positive 5. Agar 6. Reservoir 7. Transmission 8. Symptoms (3) |
1. Gram -ve coccobacillus
2. Facultative 3. Carbohydrates 4. Oxidase positive 5. Enriched blood agar 6. Cats & Dogs 7. Bite or Scratch 8. Diffuse Cellulitis w/ Clear Border at Site of Infection |
|
|
Burkholderia mallei
1. Disease 2. Contracted from (3) 3. Endemic in (5) 4. Morle likely to cause B. pseudomallei 5. Disease 6. Vehicle 7. Reservoir (6) 8. Endemic in 9. Example 10 More likely to cause |
1. Glanders (a vet disease)
2. Horse, Donkeys & Mules 3. Asia, Middle East, Africa, Central & South America 4. Acute Local Infeciton 5. Meliodosis (Whitmore's disease) 6. Strangant Fresh water 7. Sheep, Cattle, Pigs, Dogs, Cats & Humans 8. South East Asia (V'NAM) 9. HELICPOTER 10 .Pulmonary Infection |
|
|
Both Burkholderia
1. Four basic from of the disease |
1. Acute Local→ Ulcer can spread to Lymphatics
2. Pulmonary 3. In immunocompromised, Acute Septicemia → Highest fatality rate 4. Chronic → Visceral damage w/ multiple abcesses |
|
|
Burkoholderia that causes & more like to take what form
1. Glanders 2. Meliodosis |
1. mallei (local)
2. pseudomallei (pulmonary |
|
|
Glanders & Meliodosis
1. Pulmonary difficult to distinguish vs. 2. Local 3. Isolate bacteria from (3) 4. Chronic infections may remain dormant for (2) 5. Complication (2) 6. Septecemia Fatality w/ treatment 7. w/o |
1. TB
2. Many other infections 3. Blood Sputum, Urine, Skin lesions sources 4. 10 to 20 yrs 5. HIV & Diabetes 6. 35-60& 7. 95% |
|
|
Yersinia pestis
0. Caused 1. Bacteria 2. Member of 3. 4 characteristics of this group 4. Grows readily on 5. Present in virulent strains |
0. Black Plague
1. Gram negative 2. Enterobacteriacae 3. Gram -ve non spore forming rod, Oxidase negative, Facultative & Glucose Fermented 4. MaConkey agar 5. Rich polysacchardie capsue |
|
|
Y. pestis
1. Reservoir 2. Type of infection in reservoir 3. Meta-Stable balance = 4. Main vector 5. Flea contracts Yersina when 6. Multiples in (2) 7. Starving flea, when taking next meal 8. Infection in Flea → |
1. Small Rodents: RATS, voles, Ground hogs & Squirrels
2. Lymphohematogenous (endemic in rodent population) 3. Requries host to grow, but kills host too 4. Xenopsillia cheopsis (Rat flea) 5. Takes blood meal 6. Proventriculs→Block fleas GIT 7. Regurgitates infectious material 8. DEATH |
|
|
Y. pestis
1. Primary Exposure 2. Organisms Spreads to 3. What happens here (3) 4. Spread continue via → (4) 5. Pulmonary infection can be spread via |
1. Flea bite
2. Lymph Noedes 3. High Temp → Virulence Factor Formation, Rapdi Multiplication, & LN → BUBO (pianful) 4. Bacteriam → Liver, Spleen, Lungs & (sometimes) Meninges 5. Respiratory dropletns (Pneumonic Plague) |
|
|
Yersini pestis
1. Favored LNs (2) 2. Bubonic Incubation 3. Bubonic Acute starge (6) 4. Pneumoninc Incubation 5. Pneumoninc Acute Stage Symptoms (3) |
1. Inguinal & Axillary
2. 4-7 dayts 3. Swollen, Painful LNs, ↑ Feverm Pooling of Blood & MACROhemmorhages in Face & Extremeties 4. 18-36hrs 5. Violent & Fulminating Pneunmonia. FATAL |
|
|
Y. pestis & HIV ADIS
1. People who survived the plague 2. Heterozygous for mutation 3. Homozygous for mutation 3. He |
1. Mutation in CCR5
2. ↑ Resistance to HIV 3. Immune to HIV → |
|
|
Y. pestis
Bubonic diagnosis 1. Sample 2. Diagnosis Pneumonic 3. Sample 4. Diagnosis |
1. Lymph node aspirate or Blood sample
2. Fluroscent AB diagnosis 3. Sputum 4. Fluorescent AB |
|
|
Transmission via
1. B. recurentis 2. B. burgdorferi 3. Leptospira interrogans |
1. Louse or Tick borne
2. Ixodes ticks 3. Direct contact or water borne tranmission |
|
|
Borellia recurentis/ Tick borne relapsing fever
1. Louse maintained in 2. Tick maintained in |
1. Human population
2. Rodent reservoir |
|
|
Borrelia
1. Bacteria 2. Outer Membrane Proteins encoded by? Giving? → 3. Grown on 4. Seen on (2) 5. Diagnosis during |
1. Gram -ve Spirocherrs, thick & long
2. 4-9 Plasmids, ↑ Anitgenic Variability 3. Barbour-Stoenner-Kelly Medium 4. Microscopy * Fluorescent Microscopy 5. ACute phaase (3-4) days |
|
|
Boreullia recurentis
1. Disease 2. Onset 3. Incubation 4. Invasion of (4) 5. Initial Attack lasts 6. Further symptoms 7. Diagnosis |
1. Relapsing fever
2. Abrupt Prodrome 3. 3-4 days 4. Spleen, Liver, Kidney, Eyes &/or Brain 5. 3-7 dayts 6. Series of up to 4 cycles, each shorter & less severe 7. Blood smear during Acute phase 3-7 days |
|
|
Lyme disease
1. Most common 2. Reservoir (2) 3. Geo 4. East coast vector 5. West coast Vector 6. Seasonal incidence 7. By |
1. Zoonotic disease
2. Eastern White-Tail Deer & White-Footed Deer Mouse 3. New England & northeast europe 4. Ixodes dammini 5. Ixodes pacificus 6. Summer 7. NYMPH |
|
|
Borellia sp
1. In tick vector (3 steps) 2. When tick feeds (6 steps) |
1. Borellia sp→ adheres to epthelial cells of Tick GUT → Quasidormant state
2. Feeding → Mircoorgnaimsims exposed to higher temperatures → Activates them→ Multiply→ Penetrate Slvary Glands →Injected into skin of host |
|
|
Ixodes sp.
1. Season: Egg to Adult 2. When most infectious |
Winter: Eggs dormant →Spring/Summer Larvae hatch→ Early Fall: Become NYmphs after vertebrate meal → Winter: Nymphs dormant →Spring/Summer : Require another blood meal to become Adult→Summer/Fall: Adult lays eggs
2. The second SRPING/SUMMER |
|
|
1. Ticks are removed via (3)
2. Why |
1. Tick tool, Burning or Iodine
2. Don't want to squirt disease into host |
|
|
Borrelia burgdoferi. Decribe the time & what is happening
0. Incubation period 1. Stage 1 2. Stage 2 Latent Infection 3. Stage 3 |
27-33 day: Organism multiplies in Skin
1. 4 weeks: Localized infection → Erythema migrans 2. 1 week - 6monints: Disseminated infection → Secondaty ANNULAR skin lesions L: Organims in protected niches 3. 6 months - 30 years: Acrodermatitis chronicna atrophicans |
|
|
If Boreilla burgdoferi, stragiht into blood
1. Dissemination of Organisms |
1. Meningitis, Caridits, Musculoskeleton pain & Eye Abnormalities
|
|
|
Chronic symptoms of B. burgodorferi
1. Intermittent 2. Chronic (3) 3. Chronic severe |
Intermittent chronic arthritis
2. Chroninc encephalopathy, ploy neuropathy & Leukoencephalitis 3. Chronic cardiomyopathy |
|
|
B. burgorferi
1. First stage? Time? 2. Oter symptoms (4) 3. Second Stage Symptoms (3) 4. thrid Stage |
1. Erythema chronicum Migrans "target lesion" @ 3- 14 days
2. Red/Brown purple lesions at Earlobes, Nipples, Scrotum & Exteremties 3. Arthritis (Knee), pain in bursa, tendons & muscle. 4. ACA (Acrodermititis Chronicum Atrophicans) & Discoloration of Skn |
|
|
B. burgodorferi
1. Analgous to |
1. Syphillus
|
|
|
B. burgodorferi
1. During Early stage can be seen in 2. Later stage |
1. Blood smear
2. Serology unreliable |
|
|
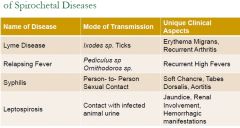
Mode of Transmission & Clinical aspects for the following
1. Lyme Disease (1 & 2) 2. Relapsing fever (2 & 1) 3. Syphillus (2 & 3) 4. Leptospirosis (1 & 3) |
|
|
|
Leptospirosis
1. Animal 2. Shed 3. Transmission between animals via 4. Exposure (2) 5. Organisms enter via (2) 6. Multiply in 7. Seed in (4) |
1. Kidney in Rodents
2. Urine 3. Drinking water with urine in it 4. Occupational (fly fisher) or Recreational (drinking water from river) 5. Abrasions in skin or Mucous membrane 6. Blood 7. Seed liver, Kidney, Lungs &/or meninges |
|
|
Leptispora interrogans
1. Bacteria 2. Differentiate vs. other 3. Motile, Spore, Capsule 4. Sensitive to (3) 5. Survives how long? in? 6. Enters susceptible host via |
1. Tight gram-ve SPIROCHETE, think & long
2. Curved into HOOK 3. Motile, no, no 4. Heat, Drying & Most chemicals 5. 1-2 weeks in Slightly Alkaline Ground water/Soil 6. Penetrating Skin/Mucus Membrane |
|
|
Leptospira interrogans
1. Incubation 2. Early symptoms 3. Later symptoms 4. Course 5. Diagnosis |
1. 8-12 days
2. Flu0like plus PAIN in THIGHS, CALVES & ABDOMEN 3. Weill's Diseae: Jaundice, Renal Dysfuntion & SEVERE HEMORRHAGC Manifestations 4. HIGH mortality rate 5. Serology: Macro & Micro agglutinnation |
|
|
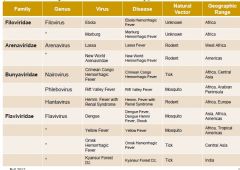
For the following Hemorrhagic Viruses, name the Family, Genus, Disease, Natural Vector & Geo
1. Ebola 2. Marburg 3. Lassa. 4. New world Arenaviridaie 5. Crimean Conog Hemorrhage Fever 6. Rift Valley Fever 7. Hemm. Fever w/ Renal Syndrome 8. Dengue 9. Yellow Fever 10. Omsk Hemm. Fever 11 Kyansur Forest |
|
|
|
Flavivurs
1. Family 2. Genus 3. Genome 4. Class 5. All are? Except 6. All serologically related to |
1. Flaviviridae
2. Flavivirus 3. ss+ RNA 4. Class IV 5. ARBOviruses 6. Cross Reacting Bodies |
|
|
Name 4 flaviviruses that produce hemmorhagic fever
|
1. Dengue, Yellow Fever, Omsk Hemm. Fever & Kyansur Forest Dz
|
|
|
Falvivirus
1. Pathogenesis 2. Infect 3. Damge cells 4. Tissure destruction via 5. Shock syndrome due |
1.Macrophages
2. Cell damage by cytokine storm 3. Tissue destruciton by T cells 4. Virus-AB complex enters monocytes via FC 5. AB ehnahces infection 6. Increased production of cytokines 7. Severe, illness, shock & hemmorrhagese |
|
|
Dengue Fever
1. Symtpms (3) 2. Hemorrhagic Shock syndrome 3. Vector 4. reservoir 5. Region (5) 6. Key for dengue |
1. Fever, Rash & Hemorrhagic Shock Syndrome
2. Severe illness, shock, hemmorhage & 10% mortality 3. Mosqutioes 4. Unknown 5. India, SE Asia, Pacific, South America & Caribbean 6. Normal a 1st & a 2nd infection |
|
|
Yellow Fever
1. Reservoir 2. Vector 3.Symptoms (2) |
1. Monkey
2. Aedes Ageytpi 3. Hemorrhagic fever w/ Jaundice |
|
|
Arena Virus
1. Family 2. Genus 3. Genome 4. Baltimore 5. Unique 6. Cause H.F. ? |
1. Arenaviridae
2. Areanavirus 3. ss - RNA, 2 segments 4. Class V 5. Host ribosome in virus particle 6. Lass Virus, Macuvirus, Juninvirus, Guantovirus |
|
|
Which arenavirus is located in
1. Argentina 2. Bolivia 3. Sierre leone 4. Venezuale 5. Highest mortalily 6. Reservoid of Bush RAT (Mastomys natelnsis) 7. Bush MICE (Callomys) (2) 8. Cane (zygodontomys bervicauda) & Cotton Rats (Sigmoid alstoni) |
1. Juninvirus
2. Machupovirus 3. Lass fever 4. Guantovirus (highest nortality) 6. Lass Fever 7. Machu & Junin 8. Guanarito |
|
|
Bunyaviruses
1. Family 2. Genra 3. Genome 4. Baltimore 5. Name THREE. H.F. viruses |
1. Bunyaviridae
2. Bunyavirus, Hantavirus, & Niarovirus 3. ss - RAN, 3 segments (S, M & L) 4. Group V 5. Nairo: Crimean Congo H.F, Phleb:Rift Valley Fever Hanta: Korean H.F. (w. Renal Syndrome) |
|
|
Bunyaviruses
1. Reservoir in (3) 2. Pathogenesis |
1. Mice, Rats & Ticks
2. Plasma & RBC leak through Vascular Epithelium |
|
|
Korean H. F.
1. Genus 2. Symptoms (2) 3.Reservoir 4. Geo (3) 5. In South West USA had |
1. Hantavirus
2. H.F. w/ Renal Syndrome 3. Mice & Rats 4. Far East, Scandinavia & E. Europe 5. severe pulmonary syndrome (Sin Nombre) |
|
|
Congo-Crimean H.F.
1. Genus 2. Symptoms 3. Reservoir 4. Vector 5. Region |
1. Niavirus
2. Fever & Hemorrhage 3. Rodent 4. Tick 5. Asia & Africa |
|
|
Filoviridae
1. Family 2. Filovirus 3. Genome 4. Baltimore 5. Viruses that cause H.F. (2) 6. mortality 7. reservoir |
1. Filoviridae
2. Filovirus 3. ss - RNA long filamentous virus 4. Class V 5. Marburgvorus & Ebolavirus 6. 20-90% 7. UNKNOWN |
|
|
Marburg virus
1. Family 2. Symptoms (3) 3. May lead to 4. Reservori 5. Vecto 6. Mortality 7. Pathogenesis (site + 3 steps) |
1. Filovirus
2. Fever, Rash & Hemorrhage 3. DIC 4. n/a 5. N/A 6. 20% 7. Liver, Spleen, Liver & Lungs → Destruction of Parenchyma → Edema → Hypovolemic Shock |
|
|
Ebolavirus
1. Symoroms (3) 2. Region (2) 3. Pathogenesis (3 steps 4. Highest to lowest pathogenic strains (3) |
1. Sudan Ferbile illness → VAscular collapse → Internal Bleeding→ Death
2. Sudan & Zaire 43. Glycoprotein peplomers → Destrcution of Endothelium → Massive Hemmorhage 4. Zaire>Sudan>Cote d'Ivoire |

