![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
Vancomycin-intermediate Staphylococcus aureus (VISA) isolates are being increasingly identified across the United States. These isolates are usually negative for the luk-PV gene encoding Panton-Valentine leukocidin and the arcA gene of the arginine catabolic mobile element. These isolates are most often susceptible to which antimicrobial agent?
A) Linezolid B) Moxifloxacin C) Daptomycin D) Clindamycin E) Rifampin |
When 33 VISA isolates were tested for in vitro activity to antimicrobial agents 100% of the isolates were susceptible to linezolid and telavancin, 6% were susceptible to moxifloxacin, 30% to daptomycin, 30% to clindamycin, and 51% to rifampin.
|
|
|
Which test is the most sensitive method for diagnosing endocarditis caused by Coxiella burnetii?
A) Blood culture with Gram stain B) Coxiella urinary antigen detection C) Detection of antibodies against Coxiella D) Tissue Gram stain of the excised heart valve E) Coxiella skin test |
Coxiella is a small, gram-negative, intracellular organism. Coxiella burnetii is associated with cattle, sheep, and goats. Humans acquire the infection when they come in contact with the infected animal or animal tissues and fluids (e.g. fetus, placentas, and milk). The organism can remain viable in soil, hay, and the environment for several years. The detection of antibodies against Coxiella burnetii is the most commonly used diagnostic test. The primary serologic assays in use today are the indirect immunofluorescent antibody (IFA) assay, the compliment fixation (CF) test, and the enzyme-linked immunosorbent assay (ELISA). The IFA is considered as being the gold standard and most commonly used method. The CF methods lack sensitivity and are less commonly used, while ELISAs become increasingly more available. Many of the newer ELISAs are reported to be as sensitive and specific as the IFA. Despite the fact that C. burnetii can be grown in vitro, this is rarely performed, and the organisms do not grow on blood agar. Likewise, the bacteria stain very poorly by the Gram stain method, which is therefore considered an unreliable test. Although cellular immunity is important in clinical recovery in this disease, a skin test documenting human disease is not available. Likewise, antigen detection tests have not been developed.
|
|
|
Which of the following statements regarding extended-spectrum beta-lactamases (ESBL) and the amp-C beta-lactamase in Enterobacteriaceae is correct?
A) Infections due to ESBL-producing Enterobacteriaceae have no effect on a patient's morbidity and/or mortality. B) The detection of AmpC-production is only clinically relevant for Klebsiella sp., but not for Salmonella and Proteus sp. C) Monobactams and cephalosporins are useful in the treatment of infections due to ESBL-producing organisms. D) Cefoxitin appears to be superior in sensitivity compared to cefotetan as a primary marker for ESBL screening. E) The expression of chromosomally located AmpC beta-lactamase is of the constitutive type and not inducible. |
D. Since AmpC producing organisms may appear susceptible to expanded-spectrum cephalosporins when initially tested, the detection of AmpC-producing Klebsiella spp., Escherichia coli, P. mirabilis, & Salmonella spp. is of signif clinical relevance. Many gram-neg bacteria harbor chrom ampC beta-lactamase genes, which are constitutively expressed at low level. In general, the expression of chromosomally located ampC genes is inducible by beta-lactam antibiotics, such as cefoxitin, cefotetan, and imipenem. AmpC beta-lactamases degrade penicillins, expanded-spectrum cephalosporins (with the exception of cefepime and cefpirome), cephamycins, monobactams, and beta-lactam inhibitors.
Detection of AmpC production in pathogens is increasingly important to ensure effective antibiotic therapy since the presence of an AmpC beta-lactamase frequently seems to result in therapeutic failure when broad-spectrum cephalosporins are used. Cefoxitin and cefotetan (both are cephamycins) are useful primary screening markers, but cefoxitin has shown to be superior to cefotetan regarding sensitivity as a screening tool. |
|
|
56-year-old male patient, who is 2 years status post lung transplant, presents with progressive dyspnea, chest pain, and what appears to be an abscess formation in the right lung, seen on a chest X-ray. An aspirate from this area is submitted for culture to the microbiology laboratory; after 3 days of aerobic incubation, cultures show mucoid, light salmon-pink colonies. On Gram stain, organisms are gram-positive coccoid bacteria; a Kinyoun stain (modified acid-fast stain) is also positive. Which of the following organisms is most likely responsible for this patient’s infection?
A) Actinomyces B) Rothia C) Streptomyces D) Rhodococcus E) Tropheryma |
The genus Rhodococcus consists of gram-positive, weakly acid-fast bacteria, that may appear rodlike, but revert back to coccoid forms in older cultures. Sometime, rudimentary branching can also be observed. Aside from Mycobacteria, Gordonia, Nocardia, and Rhodococcus stain acid fast; the latter three organisms stain only when weak acid/alcohol solutions are used. Actinomyces and Streptomyces are filamentous, branching bacteria and are commonly confused with Nocardia. In contrast to Nocardia, these organisms do not retain acid-fast stains. Rothia and Tropheryma (the etiologic agent of Whipple's disease) are gram-positive rods or coccobacilli, do not contain mycolic acid and do not retain acid-fast stains.
Rhodococcus equi is the most important human pathogen, and has been recognized with increasing frequency as a pathogen in immunocompromised patients (HIV/AIDS, and transplant patients). Like Nocardia spp., Rhodococcus equi is a facultative, intracellular organism that is able to survive in macrophages. Infection with the organism leads to granulomatous inflammation and abscess formation. Rhodococci grow aerobically on nonselective media, forming mucoid colonies that ultimately form a characteristic salmon-pink pigment. Disseminated infections and infections in immunocompromised patients should be treated with intravenous antibiotics (e.g. vancomycin, imipenem, aminoglycosides, fluoroquinolones, and/or erythromycin). However, penicillins and cephalosporins should not be used because of commonly occurring resistance against these drugs in Rhodococci. |
|
|
Immuno-chromatographic membrane assays for influenza virus detect the presence of influenza in respiratory specimens by using specific antibodies to which of the following proteins?
A) Viral nucleoprotein B) Hemagglutinin C) Neuraminidase D) Matrix-1 (M1) protein E) Matrix-2 (M2) protein |
Commercially available rapid influenza diagnostic tests detect influenza A and B viral nucleoprotein from respiratory specimens. Hemagglutinin and neuraminidase are used to classify influenza A subtypes. The M1 and M2 proteins are found in influenza A. Changes in the nucleoprotein can negatively affect sensitivity of the assay when new strain emerge with altered nucleoproteins.
|
|
|
Which of the following statement regarding the publication of a cumulative antibiogram for a hospital is most accurate?A) The annual institutional antibiogram should always include percent susceptible and percent intermediate in the statistic for all bacteria.
B) It is best to report percent antimicrobial susceptibility for bacteria for which 5 or more isolates of a given species are available. C) Because of differences in susceptibility profiles for E. faecalis and E. faecium, a separate analysis for these organisms should be done. D) Test results for supplemental antimicrobial agents should be included on all bacterial isolates obtained from intensive care unit patients. E) Semiannually, the institutional antibiogram should include percent susceptible data for all isolates from surveillance cultures. |
The CLSI guideline M39-A2 describes in detail the approach to performing and presenting the analysis of cumulative antimicrobial susceptibility data. The guidelines include the following primary recommendations:
(i) prepare report at least annually; (ii) report % susceptible and do not include % intermediate (iii) include only results from the first isolate of a given species encountered from a patient. Ignore multiple isolates of the same species in a patient irrespective of their source or overall susceptibility profile (iv) it is best to report bacteria for which 30 or more isolates of a given species are available (v) exclude all surveillance isolates (vi)report results for all antimicrobial agents tested that are appropriate for the species and do not report supplemental agents or lump isolates of the same genus (e.g. all staphylococci or all enterococci) together, irrespective of their differences in susceptibility test results |
|
|
A 75-year-old woman living in Las Vegas, Nevada presents with fever, headache, fatigue, maculopapular skin rash, and altered mental status. Cerebrospinal fluid shows pleocytosis with predominance of lymphocytes, increased protein, and normal glucose. IgM enzyme linked immune assay is positive for West Nile (WN) virus. A positive IgM assay needs to be confirmed with a neutralization test because of cross reaction with which of the following viruses?
A) Venezuelan equine encephalitis B) Eastern equine encephalitis C) Sandfly fever virus D) Colorado tick fever virus E) St. Louis encephalitis (SLE) virus |
SLE and WN are Flaviviridae which have been shown to cross react and IgM positives should be confirmed. Nipah virus and parainfluenza virus are both part of the Paramyxoviridae a nonsegmented, negative sense, single-stranded RNA virus. Norovirus is a single stranded, positive sense RNA virus. Bocavirus is a single stranded DNA virus in the Parvoviridae family.
|
|
|
A 38-year-old woman has been treated for recurrent episodes of chronic gastritis and peptic ulcers with various courses of clarithromycin and amoxicillin, combined with a proton-pump inhibitor for suspected Helicobacter pylori infection. Because of more frequently recurring clinical symptoms and the concern for possible development of antimicrobial resistance, the patient underwent a gastroscopy and biopsies were obtained. The organism, H. pylori, was successfully grown in culture, and the treating clinician requests that the microbiology laboratory performs antimicrobial susceptibility testing. For which of the following antimicrobials does the CLSI guideline M45-A2 provide breakpoints to determine susceptibility?
A) Clarithromycin B) Amoxicillin C) Metronidazole D) Tetracycline E) Levofloxacin |
The prevalence of infection with Helicobacter pylori ranges from 30% to 50% in developed countries and from 70% to 80% in developing countries. In geographical areas where the rates of clarithromycin resistance are low (<15%) or where metronidazole resistance is below 40%, the standard approach to treatment of the infection consist of a 7 day triple therapy regimen with a combination of clarithromycin, amoxicillin or metronidazole, and a proton pump inhibitor. During recent years increasing antimicrobial resistance rates in Helicobacter pylori have been reported. Not only have different approaches to treatment been suggested, but the need to perform antimicrobial susceptibility testing prior to deciding on a definitive treatment has been recognized. CLSI has defined methods and breakpoints for susceptibility testing of H. pylori against Clarithromycin, only.
|
|
|
Which of the following antimicrobial agent combinations should be tested and reported for susceptibility testing of Campylobacter jejuni?
A) Erythromycin and Ciprofloxacin B) Ceftriaxone and Levofloxacin C) Ampicillin and Gentamicin D) Vancomycin and Ampicillin E) Meropenem and Cefotetan |
The CLSI has established breakpoints & interpretative criteria for antimicrobial susceptibility testing against Campylobacter jejuni/coli. According to this guideline, a lab should report the following antimicrobial agents for AST: erythromycin (in place for macrolides), ciprofloxacin (in place for fluoroquinolones), tetracycline, and doxycycline
|
|

A 54-year-old man is admitted to the hospital with progressive unintentional weight loss, fatigue and frequently recurring respiratory tract infections over a period of the last 12 months. For the episodes of upper respiratory tract infections (URI), the patient received treatment with various antimicrobials agents, incl. azithromycin, Augmentin, and levofloxacin, at times with variable success of eradicating the infections. Because of worsening respiratory symptoms, the patient is now seen at a local emergency room. The computed tomography (CT) scan of the chest demonstrates bullous changes of the basal lobe of the right lung, a 2.5-cm right hilar lymph node, and a 6-mm precarinal lymph node. Sputum cultures are obtained. The hilar lymph node is resected, and the surgical pathology report indicates presence of abundant acid fast bacilli (AFB)-positive organisms. After 3 weeks of incubation, the cultures demonstrate growth on Middlebrook agar, which was incubated at 37oC (see picture). The organism has scotochromogenic characteristics when grown at 37oC, but is photochromogenic at 25oC. The following biochemical characteristics of this organism are observed: niacin test is negative; nitrate reduction test is positive; urease positive; heat stable catalase positive; aryl sulfatase 3-day negative and 2-week +/-. Which of the following mycobacteria species is most likely responsible for this patient’s infection?
A) M. tuberculosis B) M. bovis C) M. szulgai D) M. avium E) M. abscessus |
C) M. sulgai
|
|
|
Methicillin resistant Staphylococcus aureus (MRSA) remains as a significant concern to infection control practitioners in hospitals. Decolonization of patients prior to elective surgery (e.g. arthroplasty surgeries) may be desirable. Therefore, clinicians/surgeons may submit nasal swab cultures for testing for MRSA at the 2-week preop patient visit and would instruct patients who are positive for MRSA to apply mupirocin to both nares for decolonization prior to surgery. Which statement regarding antimicrobial susceptibility testing of mupirocin against S. aureus is correct?
A) Microbiology laboratories should use the currently approved FDA breakpoints when reporting AST results for mupirocin. B) CLSI recommends a 200 mcg disk to detect high-level mupirocin resistance in S. aureus when using the disk diffusion method. C) CLSI recommends a 5 mcg disk to detect low-level mupirocin resistance in S. aureus, defined by a zone diameter less than 8mm. D) Using the recommended CLSI method, a zone diameter of >20 mm defines absence of high-level mupirocin resistance in S. aureus. E) Two categories of mupirocin susceptibility are defined based on the level of expression of the mupA gene: susceptible and resistant. |
B) CLSI recommends a 200 mcg disk to detect high-level mupirocin resistance in S. aureus when using the disk diffusion method
|
|
|
Which of the following is considered by the Department of Health and Human Services (DHHS) to be a select agent?
A) Mycobacterium tuberculosis B) Coxiella burnetii C) Neisseria meningitidis D) Histoplasma capsulatum E) Yersinia enterocolitica |
C. burnetii is listed as a select agent, the others are not considered select agents. Select agents are specifically identified by the DHHS because of potential to be used as a bioterrorism agent. Shipping classifications are based on the probability of causing harm to person or animals.
|
|
|
A 47-year-old, homeless male patient is admitted via the emergency department to your hospital for work-up of fever-of-unknown-origin (FUO) and possible endocarditis. Several sets of blood cultures remained negative despite extended length of incubation time. On day 12 of hospital admission, the infectious disease team consults with the medical director of the microbiology laboratory, who recommended to culture blood collected with the use of the lysis centrifugation method and being plated onto heart-infusion agar supplemented with 5% fresh rabbit blood. A Gram stain of the colonies that grow 8 days later shows small, slightly curved, gram-negative rods. The catalase and oxidase tests are negative. Although the organism is biochemically very inert, a presumptive identification could be achieved using a rapid anaerobe panel (e.g. RapID ANA II). Which arthropod is a vector for transmission of this organism to humans?
A) Fleas B) Lice C) Mosquitoes D) Sand flies E) Ticks |
This patient has an endocarditis due to Bartonella quintana. The organisms is a small, slightly curved gram-negative rod that is biochemically inert in its reactions. It is oxidase and catalase negative. As mentioned in the case description above, the organism can be recovered from blood, however, routine blood cultures are rarely positive. Special procedures such as the use of the lysis centrifugation method and culture on specially enriched media (chocolate or heart-infusion agar supplemented with fresh 5% rabbit blood) are necessary to recover the organisms. Even when using these methods, the colony growth is slow (>7 days). This slow growth, together with typical colony morphology and a negative catalase and oxidase test are usually sufficient to allow for presumptive identification. The majority of commercially available identification systems do not have Bartonella in their databases; however, the MicroScan Rapid Anaerobe panel, the RapID ANA II, and Rapid ID 32A panels have been successfully used for identification.
Bartonella quintana is transmitted via the human body louse; the infection typically occurs when body lice feces are scratched into the skin by the host. Bartonella quintana causes trench fever, endocarditis, bacillary angiomatosis, peliosis, and chronic bacteremia in infected human hosts. Since 1992, the organism has been recognized as a re-emerging infection in homeless populations in the United States and Europe, as well as an opportunistic pathogen in patients with AIDS. |
|
|
A 45-year-old male, HIV-positive patient is admitted to your hospital because of recurrent episodes of oropharyngeal thrush. The patient complains of creamy, white plaque-like lesions on his tongue and throat and now has difficulties swallowing. The patient has received HAART and fluconazole prophylaxis for the past 2 years and has been compliant with his therapy. Material from the oropharyngeal lesions is submitted for fungal culture. The organism grows within 48 hours; it is dark green on CHROMagar Candida and is germ tube positive. The organism grows readily at 37oC but not at 42oC. The organism has a fluconazole MIC of 32 mcg/mL. Which of the following yeast is most likely the cause for this patient’s condition?
A) Candida krusei B) Candida albicans C) Candida dubliniensis D) Candida parapsilosis E) Candida glabrata |
Oropharyngeal candidiasis (OPC) continues to be a common opportunistic infection in patients infected with human immunodeficiency virus (HIV) or who have AIDS. Candida albicans is the most common causative agent; however, other species, such as C. glabrata, C. tropicalis, and C. krusei have become increasingly prominent pathogens. A recently described species, C. dubliniensis, has been associated with the presence of OPC in HIV-infected patients and has also been recovered from healthy, non-HIV-infected patients. C. dubliniensis is closely related to C. albicans, and many C. dubliniensis isolates may have been improperly characterized as atypical C. albicans due to the phenotypic similarity of the two species. For example, both species produce germ tubes and chlamydoconidia, typically used to identify C. albicans. C. dubliniensis has been reported to produce a distinctive dark green color on CHROMagar Candida. However, this atypical color may not persist after serial passage of the organism and may be less useful for identifying isolates. In addition, differential temperature is useful in distinguishing C. albicans from C. dubliniensis. At 42°C and 45°C, C. dubliniensis demonstrates negligible or no growth. In the study by Kirkpatrick, all isolates identified as C. albicans grew well at 37°C or 42°C.
|
|
|
A 32-year-old woman with severe, bilateral joint pain in her elbows, wrists, and knees is seen in the emergency room at your hospital where you are the director of the clinical laboratories. The patient also reports of fatigue and complains of a headache. Upon further questioning, she indicated that she had returned from a 3 week vacation in Thailand just 2 weeks ago. She further reports that during her last week of vacation, she had a fever of 103oF (39.5oC) which she treated with acetaminophen. The fever lasted 8 days. She indicates that the joint pain, fatigue and fever have been worsening over the past 2 weeks and that these symptoms began shortly after she had the fever. During her vacation, the patient spent significant time in rural areas and had numerous mosquito bites despite the use of insect repellent. Which of the following laboratory tests is most likely to provide a confirmatory diagnosis for this patient?
A) RT-PCR and culture for Nipah virus B) RT-PCR and culture for Chikungunya virus C) ELISA to detect IgM and IgG against Chikungunya virus D) RT-PCR and culture for Dengue virus E) ELISA to detect IgM and IgG against Dengue virus |
Chikungunya virus (CHIKV) is an alphavirus that is transmitted to humans via the bite of infected Aedes mosquitoes. The virus was first recognized as a human pathogen during the 1950s in Africa; since then numerous cases and epidemics have been reported throughout Africa and Asia. In 2004, CHIKV re-emerged in Kenya, subsequently spread throughout countries in and around the Indian Ocean. There is usually a 3-7 day incubation period after being bitten by an infected Aedes mosquito. The illness is usually diagnosed as a "dengue-like" disease until laboratory confirmation of CHIKV infection is established. CHIKV infection begins with an abrupt onset of fever (>38.9oC) and lasts up to 2 weeks. Most patients develop shortly after the onset of fever debilitating polyarthralgia. Joint pain is usually bilateral and commonly affects elbows, wrists, fingers, knees, and ankles.
Because CHIKV infections cause high-level viremias, the diagnosis during the acute phase of the illness (first 7-10 days) can be easily achieved with reverse-transcriptase (RT) PCR or viral culture. In 2008, real-time RT-PCR assays became commercially available in limited markets and are preformed in reference laboratories. ELISA will detect both anti-CHIKV IgM and IgG from either acute- or convalescent-phase samples. IgM antibodies develop rapidly within 5-7 days after the onset of illness and persist for several months. Because the patient described in this case scenario presented to the hospital after returning from her vacation and approx. 2-3 weeks after the initial onset of symptoms, ELISA for IgM and IgG would be the most appropriate test to confirm the diagnosis at this point. Testing for Nipah virus is not indicated because the patient travelled not in an endemic area for this disease. |
|
|
Mycobacterium tuberculosis can be differentiated from Mycobacterium bovis and M. bovis BCG strain by the use of the following tests: niacin, nitrate reduction, colony morphology, susceptibility to thiophen-2-carboxylic acid hydrazide (TCH) and pyrazinamide. Which of the following test results is characteristic for Mycobacterium tuberculosis?
A) Niacin - positive; nitrate reduction - positive; rough colony morphology; TCH resistant; pyrazinamide susceptible B) Niacin - positive; nitrate reduction - positive; smooth colony morphology; TCH resistant; pyrazinamide resistant C) Niacin - negative; nitrate reduction - negative; smooth colony morphology; TCH susceptible; pyrazinamide resistant D) Niacin - negative; nitrate reduction - negative; smooth colony morphology; TCH susceptible; pyrazinamide susceptible E) Niacin - negative; nitrate reduction - negative; rough colony morphology; TCH susceptible; pyrazinamide resistant |
A: Niacin+, NO3 reduxn+, rough, TCH resistant, Pyr susceptible = M. tuberculosis
C: M. bovis D: M. caprae E: M. bovis BCG strain |
|
|
A 64-year-old man is diagnosed with meningitis and admitted to the intensive care unit. A cerebrospinal fluid (CSF) sample is obtained from the patient and submitted to the laboratory for bacterial cultures. On day 2, the culture is positive for E. coli. The laboratory is using a commercial system for combined organism identification and antimicrobial susceptibility testing (AST). Results for which of the following antimicrobial agents should NOT be reported to the treating physician(s)?
A) Ampicillin B) Ceftriaxone C) Gentamicin D) Levofloxacin E) Meropenem |
D. Levofloxacin
According to CLSI M-100-S22, the following antimicrobial agents should not routinely reported for bacteria isolated from CSF: agents administered by the oral route only, 1st- and 2nd-generation cephalosporins, cephamycins, clindamycin, macrolides, tetracyclines, and fluoroquinolones. However, Cefotaxime and Ceftriaxone should be tested and reported on isolates from CSF in place of cefazolin. |
|
|
A 22-year-old male college student presents to the student clinic with fever and a sore throat for 2-days duration. A rapid, group-A streptococcal antigen test from a throat swab is negative. A second swab is submitted for culture. The organism grows after 48 hours of incubation on sheep blood agar and is beta-hemolytic. The catalase and urease tests are negative. The organism is positive for a reverse CAMP test reaction. This short gram positive rod that causes exudative pharyngitis and that may be confused in the laboratory with Streptococcus pyogenes is
A) Rothia dentocariosa. B) Arcanobacterium haemolyticum. C) Corynebacterium pseudodiphthericum. D) Listeria monocytogenes. E) Erysipelothrix rhusiopathiae |
The genus Arcanobacterium comprises of six species, all of which are beta-hemolytic, except A. pluranimalium. A. haemolyticum is the most important species associated with human disease. All Arcanobacterium species grow and express hemolysis best in a CO2-enriched atmosphere.
|
|
|
Ventilator-associated pneumonia (VAP) is a challenging clinical diagnosis encompassing a variety of radiographic findings and wide-ranging signs and symptoms. How can a Gram stain result of a properly collected lower respiratory specimen help direct anti-infective therapy?
A) Initial therapy can be narrowed in spectrum if positive for gram-positive organisms. B) Initial therapy can be narrowed in spectrum if positive for gram-negative organisms. C) A positive Gram stain correlates well with culture and is evidence of infection. D) A positive Gram stain has a high positive predictive value and may guide therapy. E) A negative Gram stain has a high negative predictive value and may guide therapy. |
E.
A negative Gram stain from an adequately collected respiratory specimen has a high negative predictive value and suggests VAP is unlikely. A positive Gram stain, for either gram-positive or gram-negative organisms, is only moderately specific and doesn't correlate well with culture. Empiric therapy should be broad and directed against common pathogens that cause VAP. Narrowing of initial therapy should not occur on the basis of a Gram stain positive for only one type of organism. |
|
|
A 32-year-old man presents to the dermatology clinic with a single, solitary skin lesion on his posterior right thigh that has been for several months and has been slowly increasing in size. Minimal surrounding erythema & no assoc proximal or distal LAD. The pt indicates that he has recently returned from Peru where he spent much time in rural areas & the outdoors as a missionary worker. At present time, the pt denies fever, myalgia, malaise, or wt loss. Bx of the lesion were taken for histologic analysis & cx in microbiology. The skin bx exhibits mixed granulomatous inflmmxn w/ a focal area of central necrosis. The epithelioid type granulomata are surrounded by a chronic inflammatory infiltrate of lymphocytes & plasma cells. What is the most likely organism responsible for this condition?
A) Mycobacterium leprae B) Leishmania donovani C) Leishmania braziliensis D) Trypanosoma cruzi E) Staphylococcus aureus (MRSA) |
C. Leishmania braziliensis
More than 90% of all cases of cutaneous leishmaniasis occur in Afghanistan, Algeria, Brazil, Iran, Iraq, Peru, Saudi Arabia, & Syria. Most of mucocutaneous leishmaniasis is reported from Bolivia, Brazil, and Peru. There is a distinct geographic distribution of Leishmania species around the world: L. donovani is found in Africa & Asia, L. braziliensis in South & Central America, L. mexicana in Texas, Belize, Guatemala, and Mexico, L. tropica in Afghanistan, India, Turkey, and former USSR. In endemic areas, the dx can be made on clinical grounds. The development of one or more chronic papular skin lesions together w/ a hx of exposure in an area of endemicity is suggestive of cutaneous leishmaniasis. Definitive dx is achieved by demonstrating the amastigotes in the clinical specimen or the promastigotes in cx. |
|
|
Interferon gamma release assays have been developed and approved by the FDA as aids in diagnosing Mycobacterium tuberculosis infections. These assays use peptides ESAT6 and CFP-10 that are
A) absent from M. kansasii. B) absent from M. szulgai. C) absent from M. marinum. D) absent from BCG vaccine strains. E) present on M. chelonae. |
E)
Both the QuantiFERON-TB Gold In-Tube (QTB)test and the T-SPOT.TB test use synthetic ESAT6 and CFP-10 peptides. The QTB test also uses part of the TB7.7 protein. These proteins are present in all M. tuberculosis and they stimulate measureable release of IFN-gamma in most infected people. ESAT6 and CFP-10 are absent from BCG strains but are present and may cause a false positive in patients with an M. kansasii, M. szulgai, or M. marinum infection. |
|
|
Which of the following statements regarding antimicrobial susceptibility testing (AST) and guidelines for AST results reporting is true?
A) Because of the AST guidelines published in the CLSI M-100 document, all laboratories in The United States consistently perform and report results of antimicrobial susceptibility testing appropriately. B) The term cascade reporting applies to the practice of placing all antibiotics of a certain class in rank order based on the cost for the drug and report AST resulting only for the most expensive. C) A most recent consensus statement is that laboratories should only report category interpretations for AST and not the actual minimum inhibitory concentration (MIC) data, because of the obscure relationship between MICs and clinical outcome. D) Performance of routine AST and determining MIC data is not useful for immediate patient care but only provides the essential information for establishing a cumulative annual antibiogram and antimicrobial stewardship. E) In vitro susceptibility testing data are the single most important predictor for clinical outcome of infections, because in-vitro antimicrobial test data eliminate effects of patients' host-defense factors. |
C) A most recent consensus statement is that laboratories should only report category interpretations for AST and not the actual minimum inhibitory concentration (MIC) data, because of the obscure relationship between MICs and clinical outcome.
|
|
|
A female baby, born prematurely at 35 weeks gestation, is admitted to the neonatal intensive care unit (NICU) at your hospital with fever, listlessness and a bulging fontanel. A Gram stain of the cerebrospinal fluid (CSF) reveals gram-positive rods. Blood cultures are obtained and also show growth of gram-positive rods. The mother reports an episode of a flu-like illness approximately 5 weeks prior. The mother's illness occurred a few days after a visit to a dairy farm, where she ate freshly prepared soft cheese and goat cheese. The treating physician suspects an infection with Listeria monocytogenes. Which if the following laboratory testing characteristics are most likely to be expected for this organism?
A) Catalase - positive; gamma hemolytic; CAMP test positive; hippurate hydrolysis - negative B) Catalase - positive; beta-hemolytic; CAMP test - positive; hippurate hydrolysis - negative C) Catalase - positive; beta-hemolytic; CAMP test - positive; hippurate hydrolysis - positive D) Catalase - positive; beta hemolytic; CAMP test - negative; hippurate hydrolysis - negative E) Catalase - negative; beta hemolytic; CAMP test - negative; hippurate hydrolysis - positive |
C) Catalase - positive; beta-hemolytic; CAMP test - positive; hippurate hydrolysis - positive
|
|
|
A 20-year-old man presents with dysuria and copious, thick, purulent urethral discharge. A Gram stain of the discharge fluid demonstrates gram-negative intracellular diplococci. The patient reports that he had a similar episode of symptoms 2 weeks ago, for which he was treated with ciprofloxacin as a single drug-therapy regimen. Which of the following statement regarding the further clinical and laboratory management of this patient's condition is most accurate?
A) Without the need for further laboratory testing, the patient should receive another course of treatment with levofloxacin. B) Because of emerging fluoroquinolone resistance in N. gonorrhoeae, the patient should now receive treatment with cefixime. C) Because this patient’s illness is caused by Chlamydia trachomatis, he should have received azithromycin for his treatment. D) A positive result for test-of-cure by nucleic acid amplification testing (NAAT) should be confirmed by culture method and phenotypic susceptibility testing. E) Because of the postantibiotic effect of all fluoroquinolones, the patient's symptoms will subside shortly without further treatment. |
D) A positive result for test-of-cure by nucleic acid amplification testing (NAAT) should be confirmed by culture method and phenotypic susceptibility testing.
|
|
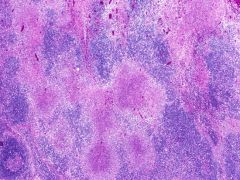
dx?
|
Cat-scratch disease
Bartonella henselae suppurative necrosis |

