![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
|
Immune system specificity:
|
The ability to recognize a pathogen and fight it individually.
|
|
|
What are the two different branches of the specific immune system?
|
-The Humoral Immune System (Antibody-Mediated)
-The Cell-Mediated Immune System |
|
|
The Humoral Immune System responses deal with:
|
B-Cells and their eventual production of antibodies.
|
|
|
The Cell-Mediated Immune System responses deal with:
|
T-Cells
|
|
|
Is there some crossover between the branches?
|
Yes, they are not completely distinct from one another.
|
|
|
Define Immunity:
|
The bodies defense against a particular pathogen.
|
|
|
Define Cell-Mediated Immunity:
|
Deals with T-Cells
|
|
|
Define Humoral Immunity:
|
Deals with B-Cells and their production of antibodies.
|
|
|
Define Antigens (Ag):
|
Something that triggers an immune response; whatever is causing the immune system to respond.
|
|
|
Define Antibodies (Ab):
|
Proteins made by B-Cells to attack the Antigens.
|
|
|
Define Antigenic Determinant (Epitope):
|
The precise part of the Antigen that the Antibody binds to.
|
|
|
If the Immune System is responding to a bacterial cell, the entire bacterial cell is the _____________, and the parts on its surface where the antibodies will bind are called _____________.
|
ANTIGEN; ANTIGENIC DETERMINANTS / EPITOPES
|
|
|
Where the Antibody attaches to the Antigen is called:
|
The Antigenic Determinant/Epitope.
|
|
|
What kind of things can serve as Antigens?
|
Anything; anything that triggers immune response.
-Bacteria -Viruses -Foreign human or animal cells -Pollen or Dust |
|
|
What sorts of structures make good Antigens, ie. stimulate a large immune response?
|
Generally, the LARGER, more COMPLEX the molecule, the stronger the immune response.
|
|
|
What sorts of structures make bad Antigens, ie. don't stimulate a large immune response?
|
Smaller molecules or molecules with a repetitive structure.
|
|
|
Why do smaller molecules or molecules with a repetitive structure stimulate a smaller immune response?
|
Because there is only one Antigenic Determinant over and over.
|
|
|
The importance of having a good Antigen is seen in:
|
Vaccine technology, where it is important to choose a large, complex molecule with lots of Antigenic Determinants on it to stimulate a large immune response and get lots of memory cells from it.
|
|
|
Describe the Antibody Structure:
|
The Antibody is made of 4 protein chains:
-2 are identical HEAVY chains (having the same amino acid sequence) -2 are identical LIGHT chains The heavy chains are attached together, and the Light chains are attached to the heavy chains. |
|
|
Describe the regions of the Antibody:
|
There are two regions on both the heavy and light chains:
-the Constant region -the Variable region |
|
|
Describe the Constant region of Antibodies:
|
The constant regions have the exact same amino acid sequence. All Antibodies of the same class have an IDENTICAL constant region.
|
|
|
The area at the tip of both the heavy and light chains of the antibody:
|
the Variable region.
|
|
|
What does the Variable region determine?
|
The Variable regions controls what the antibody binds to; ie. it's specificity.
-one antibody binds to E. coli and nothing else, another antibody has a different variable region and binds to Salmonella and nothing else. |
|
|
What controls the specificity of antibodies? ie, what the antibody can bind to?
|
The variable regions
|
|
|
On the Antibody:
-The top of the Y structure is called: -The bottom of the Y structure is called: |
-The top of the Y structure is called: the Antigen Binding Fragment (Fab).
-The bottom of the Y structure is called: the Crystallizable Fragment (Fc). |
|
|
On Antibodies, the binding site for cells is on the:
|
Crystalizable Fragment
|
|
|
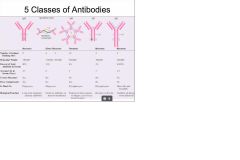
What are the 5 classes of Antibodies?
|
-IgG
-IgA -IgM -IgE -IgD |
|
|
Antibodies are also called:
|
Immunoglobulins
|
|
|
Describe IgG:
|
Exist as Monomers; known for being the Memory Antibody
|
|
|
Describe IgA:
|
Exist as Dimers; "the secreted antibody." Found in all body secretions:
-Saliva -Mucus -Cervical secretions |
|
|
IgA Dimers are composed of:
|
2 monomers attached together through a protein called the J-chain.
|
|
|
What is unique about IgA?
|
It has the Secretory Component; a molecule added in that allows IgA to be secreted in body fluids.
|
|
|
Describe IgM:
|
Exist as a Pentamer; five monomers held together via J-chain. The first antibody made during immune response; can serve as B-Cell receptor.
|
|
|
Describe IgD:
|
Exists as a monomer; Is the receptor on B-Cells.
|
|
|
Which Antibodies are monomers?
|
IgG, IgE, & IgD
|
|
|
Which Antibody is the first one made during immune response?
|
IgM
|
|
|
Describe the B-Cell receptor:
|
The B-Cell receptor is simply an IgD antibody stuck on its surface.
|
|
|
Describe IgE:
|
Exists as monomer; specifically involved in allergy responses.
|
|
|
Which antibodies bind to phagocytes?
|
IgA & IgG
|
|
|
Which antibodies bind to B-cells?
|
IgM & IgD
|
|
|
Which antibodies bind to Mast cells & Basophils?
|
IgE
|
|
|
What makes the classes of Antibodies?
|
The Identical amino acid sequences of their Constant regions.
|
|
|
Do antibodies of the same class have the same Variable regions?
|
No. ie, one will have Variable regions that will bind to e. coli, while another has Variable regions to bind to Strep pneumoneae. This is what gives them their specificity.
|
|
|
What are the antibodies functions?
|
-Compliment Fixation(Classical pathway of triggering complement)
-Agglutination -Neutralization -Opsonization |
|
|
Describe Opsonization:
|
The enhancement of phagocytosis by coating the microbe with Compliment proteins or antibodies.
|
|
|
Describe Agglutination:
|
The binding of antigens together to deactivate them.
|
|
|
Describe compliment fixation:
|
The classical mechanism of triggering Compliment:
-The antibody binds to its antigen triggering the first Compliment protein the the cascade, C1 → Opsonization, Activation of Mast cells (triggering of Inflammation), & Cytolysis by MAC. |
|
|
Describe Neutralization:
|
When Antibodies surround the pathogen so that it can't attach to host tissues. (usually used against viruses)
|
|
|
There is a repertoire of __________ in the _________.
|
B CELLS in the LYMPH NODES.
|
|
|
The B cell receptor on each B cell is:
|
specific for a particular antigen; each one is different.
|
|
|
Define Clonal Selection:
|
When the B cell is activated by the antigen binding to its receptor, endocytosis, & T Helper Cell interaction.
|
|
|
What happens after Clonal Selection:
|
Clonal Expansion, the activated B Cell will go through cell division and give rise to two different types of cells: Memory B cells and Plasma cells.
|
|
|
What then happens to the Memory B cells and Plasma cells?
|
The Memory B cells hang out in the Lymph Nodes in case of future infection; the Plasma cells secrete antibodies (IgM)
|
|
|
Define Clonal Expansion:
|
The process after Clonal Selection where B cell division creates Memory B cells and Plasma cells.
|
|
|
After an initial infection, what happens to the Plasma cells that were produced in Clonal Expansion?
|
They die, but the Memory B cells live on in the Lymph Nodes waiting for possible future infection.
|
|
|
What is the benefit of the Memory B cell response?
|
It is much faster than the Clonal Selection/ Clonal Expansion process & can flood the body with IgG very quickly in response to infection.
|
|
|
The memory response is only seen in the:
|
Specific Immune system.
|
|
|
Describe how the B Cell repertoire is made:
|

|
|
|
The B cell receptor formed will determine:
|
the antibody made; ie, if the receptor identifies Vibrio cholera, then it will make antibodies against Vibrio cholera.
|
|
|
Are all B cells unique in their specificity?
|
yes.
|
|
|
How many different possibilities are there in making B cells based on receptors?
|
1.92 Million
|
|
|
B Cells mature in the:
|
Bone marrow
|
|
|
B Cell maturation is called:
|
Clonal Deletion
|
|
|
Describe Clonal Deletion:
|
B Cells are tested to see if they interact with self tissue. Those that do are destroyed, those that pass are sent to the lymph nodes.
|
|
|
What are the steps in the life of the B cell:
|
1) Random production of B cell receptors
2) Clonal Deletion 3) Deployment to the Lymph Nodes to await Clonal Selection |
|
|
How are T cells different from B cells?
|
T cells cannot see antigen floating around them like B cells can. They have to have antigen presented to them on Self-MHC.
|
|
|
Sometimes in medicine, MHC is called:
-Tissue-typing is called: |
Human Leukocyte Antigen (HLA)
-HLA typing |
|
|
In tissue typing they are looking at:
|
MHC (HLA), trying to identify how close the donor's MHC is to the recipient.
|
|
|
What are the classes of MHC?
|
MHC Class l & MHC Class ll
|
|
|
Describe MHC Class l:
|
MHC Class l is made and presented by all cells of the body (except RBCs).
|
|
|
Describe MHC Class ll:
|
MHC Class ll is made and presented by professional Antigen Presenting Cells (APCs).
|
|
|
What exactly does MHC Class l present?
|
MHC Class l presents intracellular antigens and cellular molecules; takes things from inside the cell and presents it on the surface of the cell.
|
|
|
What exactly does MHC Class ll present?
|
MHC Class ll presents bits and pieces of digested FOREIGN antigens.
|
|
|
The real self-tag is:
|
MHC Class l
|
|
|
What binds to MHC Class l ?
|
Cytotoxic T cells
|
|
|
What binds to Class ll MHC?
|
T helper cells
|
|
|
Cytotoxic T cells bind to MHC Class __ via:
|
Cytotoxic T cells bind to MHC Class l via their T CELL RECEPTOR & CD8
|
|
|
T helper cells bind to MHC Class __ via:
|
T helper cells bind to MHC Class ll via their T CELL RECEPTOR & CD4
|
|
|
B cells are:
made in the _____________. mature in the ____________ . |
made in the: Bone marrow
mature in the: Bone marrow |
|
|
T cells are:
made in the _____________. mature in the _____________. |
made in the: Bone marrow
mature in the: Thymus |
|
|
T cell receptors bind specifically to both:
|
the particular Antigen and self-MHC
|
|
|
T cells also have additional receptors called:
These help: |
Clusters of Differentiation (CD)
These help with the interaction. |
|
|
Cytotoxic T cells = MHC__ & CD__
|
Cytotoxic T cells = MHC l & CD8
|
|
|
T helper cells = MHC__ & CD__
|
T helper cells = MHC ll, CD4
|
|
|
What are the two main types of T lymphocytes?
|
The T Helper Cells & Cytotoxic T Cells
|
|
|
T Helper Cells get activated and differentiate into:
|
Either:
-T helper 1 Cells -T helper 2 Cells -CD4+ T Memory Cells |
|
|
Do you get memory cells from all of the specific immune cells?
If so, what are they? |
Yes, they are:
B Cells= Memory B Cells T Helper Cells = CD4+ T Memory Cells Cytotoxic T Cells = CD8+ T Memory Cells |
|
|
What do the T Helper 1 & 2 Cells stimulate?
|
-T helper 1 Cells: Stimulate Macrophages, Cytotoxic Ts, & other T Helper Cells.
-T helper 2 Cells: Stimulate B Cells & Suppress T Helper 1 Cells. |
|
|
What do CD4+ T Memory Cells do?
|
They wait for re-activation upon future infection.
|
|
|
What do Cytotoxic T Cells do?
|
They destroy foreign or abnormal cells and give rise to: CD8+ T Memory Cells
|
|
|
What do CD8+ T Memory Cells do?
|
They wait for re-activation upon future infection.
|
|
|
Describe the T Cell Receptor (TCR):
|
The T Cell Receptor has a Constant Region and a Variable Region.
|
|
|
On the T Cell Receptor, what does the Constant Region and Variable Region bind to?
|
The Constant Region binds to: Self-MHC
The Variable Region binds to: the Antigen. |
|
|
How are T Cell Receptors made?
|
The same way that B Cell Receptors & MHC is made, random selection of exons from genes.
|
|
|
The maturation process of T Cells occurs in the ________ and is called:
|
Thymus; and is called Positive Selection or Negative Selection.
|
|
|
Describe:
-Negative Selection: -Positive Selection: |
-Negative Selection: T Cells with useless or dangerous TCRs are destroyed.
-Positive Selection: T Cells with good TCRs are propagated and sent to the lymph nodes and lymphoid tissues. |
|
|
What are the APCs?
|
Macrophages, B Cells, & Dendritic Cells
|
|
|
Which APC's main job is to be an APC?
|
the Dendritic Cell.
|
|
|
APCs present antigen on:
|
MHC Class ll
|
|
|
What is the first step of T Helper Cell Activation?
|
T Cell Receptor with the help of CD4+, binds to the Antigen on MHC Class ll being presented by the APC
|
|
|
What is the second step of T Helper Cell Activation?
|
After binding, the APC releases Interleukin-1 or Interleukin-4. The T Helper Cell is now activated and ready to differentiate.
|
|
|
If the APC releases IL-1, then the T Helper will differentiate into a:
|
T Helper 1 Cell
|
|
|
If the APC releases IL-4, then the T Helper will differentiate into a:
|
T Helper 2 Cell
|
|
|
T Helper 1 Cells release ______ which activates:
|
T Helper 1 Cells release IL-2 which activates: Macrophages, Cytotoxic T Cells, & other T Helper Cells.
|
|
|
T Helper 2 Cells release ______ which activates:
|
T Helper 2 Cells release IL-4 & B Cell growth factor which activates: B Cells. They also have an inhibitory affect on T Helper 1 Cells.
|
|
|
Regardless of IL-1 or IL-4 differentiation, either way, these will be created:
|
CD4+ T Memory Cells
|
|
|
If the APC releases IL-1 then:
|
The T Helper Cell differentiates into a T Helper 1 Cell, which releases IL-2 and activates Macrophages, Cytotoxic T Cells, and other T Helper Cells.
|
|
|
If the APC releases IL-4 then:
|
The T Helper Cell differentiates into a T Helper 2 Cell, which releases more IL-4 & B Cell Growth Factor which activates B Cells. They also inhibit T Helper 1 Cells.
|
|
|
If the APC is a Macrophage or Dendritic cell, then when it interacts with the T Helper Cell it is most likely to release:
|
IL-1
|
|
|
If the APC is a B Cell, then when it interacts with the T Helper Cell it is most likely to release:
|
IL-4
|
|
|
What exactly do B Cells need to go through clonal expansion?
|
They have to present the Antigen on MHC Class 2 to a T Helper Cell. The B Cell releases IL-4 turning the T Helper Cell into a T Helper 2 Cell. The T Helper 2 Cell then releases more IL-4 and B Cell Growth Factor. The IL-4 & B Cell Growth Factor cause the B Cell to go through Clonal Expansion.
|
|
|
Define Cytokines:
|
Chemical messenger molecules that communicate between immune cells.
|
|
|
Define Interleukin-1:
|
Activates T Helper Cells to become T Helper 1 Cells when produced by the bound APC.
|
|
|
Define Interleukin-2:
|
Produced by active T Helper 1 Cells and stimulates Macrophages, Cytotoxic T Cells, and other T Helper Cells.
|
|
|
Define Interleukin-4:
|
Activates T Helper Cells to become T Helper 2 Cells when produced by the bound APC. Also produced by T Helper 2 Cells to help activate B Cells.
|
|
|
Define B Cell Growth Factor:
|
Made by T Helper 2 Cells to activate B Cells.
|
|
|
Define Interferons:
|
Stimulate production of anti-viral proteins when released by other virally-infected cells.
|
|
|
Define Chemokines:
|
Attract leukocytes to an infection when released by Mast Cells.
|
|
|
Cytotoxic T Cells bind to antigens presented on:
|
MHC Class l
|
|
|
Cytotoxic T Cells are activated by:
|
IL-2 released from T Helper 1 Cells.
|
|
|
The active Cytotoxic T Cell releases:
|
Perforins & Granzymes
|
|
|
What do Perforins & Granzymes do?
|
Perforins lyze the bound cell & Granzymes degrade cellular proteins.
|
|
|
Describe the steps in Cytotoxic T Cell activation:
|
1) Cytotoxic T Cell is activated by IL-2 released from T Helper 1 Cells.
2) Self-Cell presents a piece of Intracellular Antigen on MHC Class 1. 3) Cytotoxic T Cell receptor binds to Antigen & MHC Class 1 with the help of CD8+. 4) Cytotoxic T Cell releases Perforins & Granzymes that destroy the cell. |
|
|
Since T Helper Cells interact with MHC Class ll, they are only activated by:
|
APCs
|
|
|
T Helper Cells act as the _____ for the entire immune system.
|
the CONDUCTOR
|
|
|
Since Cytotoxic T Cells interact with MHC Class l, they can be activated by:
|
any cell of the body (except RBCs).
|
|
|
Which cells target and destroy cells with viral infections and cancerous cells.
|
Cytotoxic T Cells.
|

