![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
Plasmodium species - agents of malaria
|
P. vivax, P. ovale, P. malariae, P. falciparum
Spread by mosquitos |
|
|
Babesia species - agents of babesiosis
|
B. microti (in US) - spread by ticks
|
|
|
Toxoplasma gondii - agent of toxoplasmosis
|
Single species - spread by oocyst consumption
|
|
|
Leishmania species - agents of leishmaniasis
|
L. donovani, L. tropica, L. braziliensis
Spread by sand flies |
|
|
Trypanosomes - agents of sleeping sickness & Chagas’ disease
|
T. brucei, T. cruzi
Spread by Tsetse flies (T. brucei) & kissing bugs (T. cruzi) |
|
|
Plasmodium species Require 2 hosts for life cycle:
|
Mosquito: sexual stage
Human: asexual stage |
|
|
Plasmodium species life cycle
|
1) female mosquito transmits sporozoite to humans
2)In the liver, sporozoite turns into merozoites 3) merozoites become Trophozoites in RBC 4)Trophozites makes schizonts in RBC via asexual reproduction 5)RBC Lyses releasing merozoites 6)Gametocytes ingested by female mosquito 7) Gametocytes undergo sexual repro in mosquito and turn into sporozoites. |
|
|
In blood smear what is diagnostic of plasmodium species?
|
Schizont, Gametocytes and ring shape (immature trophozoite)
|
|
|
Most prevalent malaria Invades young RBCs
RBCs enlarged w/pink granules called Schüffner dots |
Invades young RBCs
RBCs enlarged w/pink granules called Schüffner dots Latent liver form |
|
|
Most prevalent in tropical Africa. Also in Asia, S. America
Invades young RBCs RBCs enlarged w/pink granules called Schüffner dots Latent liver form |
P. ovale:
|
|
|
Invades only mature RBCs
No RBC enlargement - band & bar forms No latent liver form Less prevalent, subtropical & temperate regions |
P. malariae:
|
|
|
Invades ANY RBCs
three or four rings may be seen in RBC rings appear at edge of cell - look stuck on surface Crescent shaped gametocytes occasionally seen No latent liver form |
P. falciparum
|
|
|
No latent liver form
Tropical/subtropical regions, often w/HIV |
P. falciparum
|
|
|
influenza-like symptoms with headache, muscle pains, photophobia, anorexia, nausea, vomiting
|
P. vivax & P. ovale. Rupturing erythrocytes liberate merozoites as well as toxic cellular debris. Produces patterns of chills, fever, malarial rigors (paroxysms) every ~48 hours. Benign tertian malaria
|
|
|
what can happen if P. vivax & P. ovale not treated?
|
to brain, kidney, and liver damage
|
|
|
18-40 day incubation period, can be months to years
influenza-like symptoms with headache, muscle pains, photophobia, anorexia, nausea, vomiting |
P. malariae: Produces patterns of chills, fever, malarial rigors (paroxysms) every ~72 hours.
|
|
|
how long does an untreated P. malariae infection last
|
as long as 20 years.
|
|
|
incubation period (shortest)
rapidly produces daily chills & fever as well as severe nausea, vomiting, & diarrhea. |
P. falciparum:
Produces patterns of chills, fever, malarial rigors (paroxysms) every 36-48 hours (more irregular). Malignant tertian malaria. |
|
|
Course of P. Falciparum infection
|
Attacks more severe - may result in death if untreated. Larger numbers of RBCs infected.
Capillary plugging can occur from debris, can involve brain and result in coma and death. Blackwater fever - sign of kidney damage |
|
|
The best time to take a blood sample for diagnosis of malaria is
|
midway between paroxysms of chills and fever when the greatest number of intracellular organisms are present.
|
|
|
P. malariae, P. vivax, and P. ovale tx
|
chloroquine
|
|
|
P. vivax & P. ovale have latent forms in the liver (protected from chloroquine.) Drug of choice for this stage is
|
primaquine.
|
|
|
Chloroquine resistant P. falciparum are present in all endemic regions, except
|
Central America & Carribean.
Should assume drug resistant if drug resistance not know |
|
|
P. falciparum treatment options include
|
quinidine, artemether
|
|
|
Malaria and babesia are very similar symptomatically, but the organisms that causee differ in that
|
babesia parasite does not infect the liver.
|
|
|
The diagnostic stage of babesia parasite is
|
trophozoite. Female mosquito transmits pyriform bodies.
|
|
|
Found in Africa, Asia, Europe, & North America. In US, found along northeastern seaboard.
|
Babesia
|
|
|
general malaise, fever, chills, sweating, weakness
As RBCs are destroyed, can lead to hemolytic anemia and renal failure Hepatomegaly and splenomegaly can develop in severe disease |
Babesia
|
|
|
Babesia infections are mild, but can cause fatal infections in
|
patients lacking a spleen.
|
|
|
Babesia tx
|
clindamycin and quinine
Those with mild disease will recover without treatment. Ticks must feed for several hours before transmission occurs, so prompt removal helps to reduce disease. |
|
|
Organisms develop in the intestinal cells of house cats. Get passed in feces where they mature into infective cysts.
|
Toxoplasma gondii
Infections come from: (1) ingestion of improperly cooked meat from animal hosts (2) ingestion of oocysts from contaminated cat poop |
|
|
Transplacental infections can occur with devastating effects on the developing fetus.
|
Toxoplasma gondii
|
|
|
Toxoplasma gondii becomes disseminated and severe in
|
Patients with HIV, organ transplants, or immunosuppression most likely to have disseminated disease
|
|
|
Toxoplasma gondii Symptoms occur when
|
T. gondii moves from blood into tissues, with cell destruction, organism replication, and cyst formation occurring.
Target organs: lungs, heart, lymphoid organs, CNS Symptoms: chills, fever, headaches, myalgias, fatigue |
|
|
Toxoplasma gondii First trimester infections can result in
|
abortion, stillbirth, or severe disease that includes epilepsy, encephalitis, microcephaly, psychomotor or mental retardation, blindness.
Symptoms may develop months to years after birth. |
|
|
Neurological symptoms, including diffuse encephalopathy, meningoencephalitis, cerebral mass lesions.
|
T. gondii - disease in older immunocompromised patients. Reactivation of cerebral toxoplasmosis is a major cause of encephalitis in patients with AIDS, but can occur in transplant patients as well.
|
|
|
Toxoplasma gondii - diagnosis
|
Serological testing is required for acute infections to look for evidence of increasing antibody titers in serial blood samples.
For reactivation, diagnosis is more difficult. Histological diagnosis or PCR of tissue samples can be used. |
|
|
Toxoplasma gondii - treatment
|
pyrimethamine plus sulfadiazine-Disseminated
clindamycin and spiramycin -pregnancy None for healthy people |
|
|
Obligate intracellular pathogen. Transmitted by bite of female sand flies. Animal to human or human to human spread can occur via flies.
Can also be transmitted through direct contact with a lesion. |
Leishmania species
|
|
|
There 3 types of diseases cause by Leishmania
|
1. L. donovani - visceral leishmaniasis
2. L. tropica - cutaneous leishmaniasis 3. L. braziliensis - cutaneous leishmaniasis |
|
|
Wide spread in Middle East & focal areas of So. America
.1. Red papule occurs at fly bite, 2 weeks to 2 months 2. Lesion becomes irritated, begins to enlarge and ulcerate. 3. Lesion becomes hard and crusty & exudes material. 4. May heal without treatment but will leave a scar |
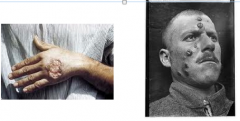
Cutaneous:
|
|
|
Bolivia, Brazil, Peru
1. Similar beginning to cutaneous, but involved destruction of mucous membranes and surrounding tissue 2. Spread may occur right away or years later 3. Lesions do not heal - disfiguring disease that can lead to death |
Mucocutaneous:
|
|
|
(also known as kala-azar or dum dum fever)
90% of cases in Bangladesh, Brazil, India, Nepal, Sudan |
Visceral
|
|
|
Gradual onset of fever, diarrhea, anemia. May resemble malaria.
3. As organisms proliferate, marked enlargement of liver and spleen, weight loss, emaciation. Kidney damage may occur. |
visceral. May occur as fulminating, rapidly fatal disease, chronic, or asymptomatic
|
|
|
Leishmania species - diagnosis
|
In endemic areas, diagnosis may be made on clinical grounds, but definitive diagnosis depends on detecting amastigotes or promastigotes in culture
|
|
|
Specimens for diagnosis of visceral leishmaniasis include
|
splenic puncture, lymph node aspirates, liver biopsy, sternal aspirates, and buffy coat preparations of venous blood. These specimens may be subjected to microscopic examination, culture, or DNA based assays.
Molecular based tests (DNA, RNA) are most sensitive, but may not be readily available in endemic areas. |
|
|
Leishmania species - treatment
|
Pentavalent antimonial compound sodium stibogluconate (Pentostam) is drug of choice.
|
|
|
For cutaneous leishmaniasis tx
|
compounds may be directly injected into lesion or parentarally – cryotherapy, heat, or surgical excision are also used.
|
|
|
African trypanosomiasis or sleeping sickness spread by tsetse flies.
|
T. brucei gambiense and T.b.rhodesiense
|
|
|
American trypanosomiasis or Chagas’ disease, spread by true bugs or kissing bugs.
|
T. cruzi
|
|
|
The diagnostic feat of Trypanosome brucei is
|
Trypomastigote in cell
|
|
|
Limited to tropical West and Central Africa (range of testse fly vector). Flies prefer shaded stream beds for reproduction and close proximity to human dwellings
|
T. brucei gambiense
|
|
|
Found primarily in East Africa, especially cattle raising countries
|
T. brucei rhodisiense
|
|
|
Early sign of infection include occasional ulcers at site of fly bite. As organisms replicate, lymph nodes are invaded and fever, myalgia, arthralgia, and lymph node enlargement results.
|
T. brucei - disease Produce chronic disease with CNS involvement that often ends in death after several years of infection.
|
|
|
Winterbottom sign
|
T. brucei infected pt Swelling of the posterior cervical lymph nodes occurs and is called Winterbottom sign. Patients in this acute phase often exhibit hyperactivity.
|
|
|
T. brucei chronic final stage
|
CNS involvement with lethargy, tremors, meningoencephalitis, mental retardation, and general deterioration.
Final stages of chronic disease include convulsions, hemiplegia, and incontinence, and the patient becomes difficult to arouse or respond, eventually progressing to a comatose state. Death is the result of CNS damage and other infections such as malaria or pneumonia. |
|
|
T. brucei tx for
acute form CNS involvement |
-Suramin
-Melarsoprol |
|
|
North, Central, and South America. Found most often in children in Central and South American, where 16-18 million people are infected.
Bugs prefer nesting in animal burrows. Cases are rare in US. |
T. cruzi , kissing bug
|
|
|
Early signs develop around bug bite as an erythematous and indurated area known as a chagoma. Often followed by a rash and edema around the eyes and face (Romaña's sign).
|
T. cruziMost severe in children <5. Fever, chills, myalgias, malaise, and fatigue.
Death may occur a few weeks after an acute attack, the patient may recover, or the patient may enter the chronic phase with organism proliferation and entry into the heart, liver, spleen, brain, and lymph nodes. |
|
|
: hepatosplenomegaly, myocarditis, and enlargement of the esophagus and colon as a result of the destruction of nerve cells.
|
Chronic Chagas' disease. Megacardia and electrocardiographic changes are commonly seen in chronic disease.
Death from chronic Chagas' disease results from tissue destruction in the many areas invaded by the organisms, and sudden death results from complete heart block and brain damage. |
|
|
T. cruzi - diagnosis
|
Can see organism in thick and thin blood films during the acute stage.
As infection progresses, organisms leave the blood and replicate within tissues requiring biopsies to visualize amastigotes. Serological tests are available, as are PCR tests, however the latter is not commonly used in the field |
|
|
T. cruzi diagnosis
|
Treatment is limited by lack of reliable agents – drug of choice is nifurtomox
|

