![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
What are the two layers of the pericardium and what separates them?
|
Inner – Visceral pericardium
Outer – parietal pericardium Separated by 15 - 50cc of fluid |
|
|
What are the 3 primary functions of the pericardium?
|
1) Fixes heart within mediastinum
2) Prevents extreme dilatation of the heart 3) ?Barrier to spread infection from lungs |
|
|
Name some common causes of acute pericarditis.
|
Infectious -Viruses (most common), bacteria
Non-infectious - post OHS (open heart surgery), post MI, ureamia, cancer (breast and lung mets), rheumatologic disease, drug induced |
|
|
What are the four pathologies of acute pericarditis? Which is the most common? Which suggests malignancy?
|
1) Serous pericarditis = scant WBCs, thin fluid likely clear or straw coloured
2) Serofibrinous = most common. Exudate contains plasma proteins. Portions of pericardium can become thick and fused. 3) Suppurative = purulent (uncommon – bacterial infection) 4) Hemmorhagic = grossly bloody (malignancy or TB) |
|
|
What are the common clinical features of pericarditis?
|
Hx: Chest pain (sharp, retrostrenal, radiating to the back), fever, dyspnea
Px: Tachycardia, fever, triphasic pericardial friction rub |
|
|
In a case of pericarditis what diagnostic tests would you order and what would they show?
|
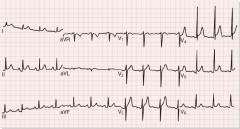
ECG - Diffuse ST elevation, PR depression
BW - increased WBCs, elevated ESR (> 80), mildly elevated troponins CXR - Normal unless effusion Echo - Normal, but may show fluid |
|
|
What is the treatment for acute pericarditis?
|
Rest and anti-inflammatory drugs.
Viral pericarditis (most common) usually runs it's course within 1-3 weeks. |
|
|
What is pericardial effusion? What determines whether it will remain silent?
|
An excess buildup of fluid (> 50cc) in the pericardium.
The 3 factors that determine whether or not it remains silent are: 1) The volume of fluid 2) The rate of accumulation 3) The compliance of the pericardium (balloon analogy) |
|
|
What are the clinical features of pericardial effusion?
|
Hx: Chest ache, dyspnea, dysphagia, hoarseness, hiccups
Px: Soft heart sounds (due to fluid insulation), Ewart sign (dullness over posterior left lung) |
|
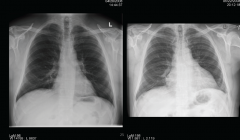
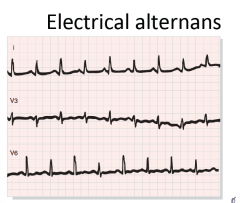
In a case of pericardial effusion what diagnostic tests would you order and what would they show?
|
CXR: Normal until ~250cc of fluid, enlrged cardiac silhouette
ECG: Reduced voltage, electrical alternans (complex variations in the wave size, due to movement of the heart within the fluid filled cavity) Echo: Fluid, effusion, hemodynamic compromise BW: WBCs, ESR, troponin, TSH, LFTs, albumin Pericardiocentesis: Diagnostic and therapeutic |
|
|
What is cardiac tamponade and what may lead to it?
|
Compression of the heart due to an accumulation of fluid due to percarditis a pericardial effusion, blunt chest trauma, ruptured LV following an MI and aortic dissection.
This can result in hypotensive shock and death |
|
|
What is the pathophysiology (consequences) of cardiac tamponade?
|
Ventricles are compressed due to fluid, especially during diastole, when the cardiac pressure is the lowest.
Systemic and pulmonary venous pressures rise. JVP becomes elevated and dyspnea and pulmonary congestion occur as a result. Reduced filling leads to a decreased CO which leads to hypotensive shock and death. |
|
|
What are the clinical features of cardiac tamponade?
|
Hx: Light-headedness, dyspnea, tachypnea
Px: Elevated JVP, systemic hypotension, quiet heart sounds, tachycardia, pulsus paradoxus |
|
|
What is pulsus paradoxus, what causes it and in what condition is it seen?
|
It is a decrease in systolic blood pressure by more than 10 mmHg during normal inspiration.
The external compression causes the two ventricles to have a fixed volume. When you breathe in, there is an increased RV volume so the septum shifts left, decreasing LV output. Seen most commonly in cardiac tamponade. |
|
|
In a case of cardiac tamponade what diagnostic tests would you order and what would they show?
|

Echo: effusion, diastolic chamber collapse
|
|
|
How is cardiac tamponade treated?
|
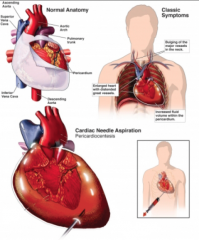
Pericardiocentesis - urgently
|
|
|
What is the pathophysiology of constrictive pericarditis?
|
The pericardium becomes thickened and calcified, often "sticking" to the heart.
As a result, diastolic filling is hindered (systole generally unaffected). On exertion, CO rises to compensate and the pericardium normally dilates to facilitate the increased volume. In constrictive pericarditis, the dilatation is hindered (balloon vs water bottle analogy). |
|
|
What are the clincal features of constrictive pericarditis?
|
Hx: Reduced CO (fatigue, hypotension), elevated systemic venous pressure (JVP, hepatomegaly, ascites, peripheral edema)
Px: Tachycardia, pulsus paradoxus, elevated JVP, pericardial knock on auscultation, Kussmal's sign |
|
|
What is Kussmal's sign, what causes it and in what condition is it seen most commonly?
|
Kussmal's sign is a phenomenon in which the JVP doesn't fall (it actually rises) during inspiration as would be normally expected.
The pericardium is very rigid in constrictive pericarditis, so during inspiration the blood is sucked into the chest, but is not able to get into the heart. This results in more blood flow into the veins, elevating JVP with inspiration. It is seen most commonly in constrictive pericarditis. |
|
|
In a case of constrictive pericarditis, what diagnostic tests would you order and what would they show?
|
CXR: May show calcifications
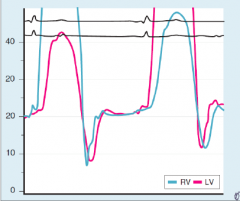
ECG: sinus tachycardia, ST T wave abnormalities, atrial arrhythmias Echo: Dilated IVC, septal bounce Cardiac catheterization: Dip and plateau |
|
|
What is the treatment for constrictive pericarditis?
|
1) Surgical removal of the pericardium (pericardiectomy)
2) Waffle procedure - hash marks to relieve some pressure, much like a mango at a buffet |

