![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Why does an aortic atresia cause significant underdevelopment of the left ventricle and aorta?
|
This is an obstruction, which leads to significantly less blood flow through the area. Blood flow is needed to stimulate growth.
|
|
|
Will a septal defect favor L to R or R to L shunting?
|
L to R shunting - high to low pressure.
|
|
|
What is the cause of dilation in a developing heart?
|
excessive blood flow
|
|
|
Define shunt
|
Shunting refers to an abnormal mixing of blood between L and R heart structures.
|
|
|
Why does a patient not become cyanotic with a L to R shunt?
|
In this type of shunt, a portion of the oxygenated blood is shunted back through the pulmonary system. *All blood leaving the aorta is oxygenated*
|
|
|
Explain why R to L shunting causes cyanosis.
|
Deoxygenated blood from the R side of the heart enters the L side of the heart, bypassing pulmonary circulation.
|
|
|
Name an example of a congenital R to L shunt.
|
Tricuspid atresia with RA to LA shunting.
|
|
|
True or false: it is easy to spot a patient with cyanosis.
|
False - a low O2 sat can cause very subtle signs of cyanosis and testing is necessary to rule out cyanosis.
|
|
|
How can you differentiate respiratory from central causes of cyanosis?
|
Give oxygen: if the pt improves, the cause of cyanosis is respiratory. If the patient does not improve, the cause is central.
|
|
|
Name the three main types of VSDs.
|
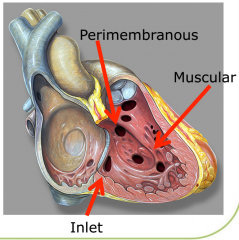
1. Perimembranous - involves membranous septum, roofed by aortic valve
2. Muscular - surrounded by muscle 3. Inlet - bordered by the tricuspid valve. Typically part of an atrioventricular septal defect |
|
|
What causes L to R shunts to become worse over the first few weeks of life?
|
Decreasing pulmonary vascular resistance.
|
|
|
Name at least three signs of CHF in infants.
|
-tachypnea
-increased work of breathing -tachycardia -failure to thrive or poor weight gain -hepatomegaly (cyanosis and edema are not usually present in infants with CHF, unless they are in mulisystem organ failure) |
|
|
Describe the pathophysiology of pulmonary congestion due to a large L to R shunt.
|
-A large volume of blood enters the pulmonary circulation (from system circulation and from the L side of the heart).
-This causes pulmonary arterial congestion. -Pulmonary interstitium becomes congested. -This causes decreased lung compliance and therefore more work is required to inflate the lungs. -Additionally, over time more vessels develop in the lungs to compensate. These can be counterproductive as they can actually cause a compressive force, reducing compliance further. *Keep in mind that a different mechanism is responsible for pulmonary venous congestion. |
|
|
Do infants have stiffer or more pliable cardiac tissue, with comparison to adults?
|
Stiffer - this makes it more difficult to increase stroke volume. Instead, infants are more likely to have tachycardia when an increase in CO is needed.
|
|
|
Why do infants with CHF often have diaphoresis?
|
A decrease in cardiac output causes increased sympathetic activity.
|
|
|
What is the most common cause of CHF in infants?
|
Excessive pulmonary blood flow.
|
|
|
Describe the management of CHF in infants.
|
Provide nutritional support - high calorie feed, tube feed, if necessary.
Heart failure meds - diuretics, other targeted treatments including beta blockers, ACE inhibitors, antiarrhythmics If medical therapy does not work sufficiently, surgery should be the next step, to close the defect. |
|
|
Do all VSDs require intervention?
|
No, many small VSDs will eventually close spontaneously or will not cause significant Sx.
A hemodynamically significant VSD will present by 3-4 months |
|
|
When can CHD be present?
|
at birth
during the first week (ductus related) in early infancy (PVR related L-R shunts) when there is maladaption or decompensation |
|
|
In an infant with a complex heart defect, what treatment is given to maintain the ductus arteriosis?
|
Prostaglandin (treatment was developed in Canada).
|
|
|
How can you recognize coarctation of the aorta during physical examination of an infant?
|
The infant will have normal brachial pulses and weak femoral pulses.
|
|
|
What is the key element of an atrioventricular septal defect (AVSD)?
|
A common, abnormal atrioventricular valve.
one valve with 5 leaflets There will be an ASD and a VSD but the hallmark is a single mitral/tricuspid valve |
|
|
How long does it take for the patent ductus arteriosis (PDA) to close (and subsequently cause decompensation of PDA-dependent defects)?
|
48-72 hours
|

