![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
What are the components of the following:
BP = ( a x b) CO = (a x b) |
BP = total peripheral resistance x cardiac output
CO = Stroke volume x Heart Rate |
|
|
What are 3 factors that determine Stroke Volume?
|
Cardiac Contractility
Venous Return Aortic Pressure (Afterload) |
|
|
"Catecholamines _______ (Increase/Decrease) HR and _________ (Increase/Decrease) Cardiac Contractility and ___________ (Increase/Decrease) Venous Tone.
Bonus: Name 2 catecholamines?" |
"Increase, Increase, Increase
Bonus: Norepinephrine, epinephrine, dopamine, " |
|
|
What happens to blood vessels as we age?
|
Become more rigid (less elastic) and accumlation of "insults" result in more arteriosclerotic deposits in blood vessels.
|
|
|
In SMOOTH muscle calmodulin when activated by calcium, activaes this enzyme which phosphorylates (using ATP) myosin to cause muscle contraction.
What is ""this enzyme"" called? |
MLCK = Myosin Light Chain Kinase
|
|
|
Artherosclerosis causes these 5 problems in the body
Narrowing of vessels by plaque Plaque Ulceration/Rupture Intraplaque Hemmorrhage Peripheral Emboli Weaking of vessel walls Match the relavant ones to these 5 diseases (can have more than 1 and can be used multiple times) Stroke Renal Artery Disease Aneurysms Coronary Artery Disease Peripheral Artery Disease |
1. Stroke = Plaque repture, Plaque hemmorahage, Peipheral emboli
2. Renal Artery Disease = narrowing of vessel, emboli 3. Aneurysms = Weaking of vessel wall 4. Coronary Heart Disease = Narrowing of vessel, plaque rupture/hemmorage 5. Peripheral Artery Disease = Narrowing of vessel, emboli |
|
Explain what this equation is for and each of the components in it in relation to vasculature.
|
R = vessel resistance
n = fluid viscosity L = length of vessel r = vessel radius ***NOTE*** - If vessel becomes narrower then since the radius is to the power of 4, the resistance goes up GREATLY |
|
|
What is laminar flow and what is turbulant flow?
|
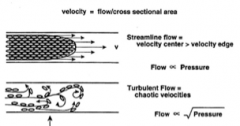
Laminar Flow (Streamline flow) = occurs when a fluid flows in parallel layers, with no disruption between the layers.
Turbulent Flow = the speed of the fluid at a point is continuously undergoing changes in both magnitude and direction. (Can hear on auscultation) |
|
|
In a healthy person is the state of the vasculature leans more towards _________ (Relaxed/Constricted) state. Where as in arthrosclerotic disease that balance shifts towards ________(Relaxed/Constricted)
|
Relaxed, Constricted
|
|
|
What contributes to:
Essential Hypertension Secondary Hypertension |
1. Essential hypertension: Fx of HTN, Obesity, Inactivity, EtOH, too much Na+, DM, low potassium
2. Secondary hypertension: Chronic Renal Failure, Primary Aldosteronism (too much), renovascular (narrowing of renal arteries), Pheochromocytoma, cushings |
|
|
Match the correct 3 together (1 from each Group)
Group #1(Class) Vasodilator Diuretic Sympatholytics Renin-Angiotensin-Aldosterone Group#2 (Drug Example) Thiazide Beta-Blocker Direct Renin Inhibitor Calcium Channel Blocker Group #3 (Physiological Action) Decrease Circulating Volume Decrease Sodium Retention Lower Vascular Resistance Lower Heart Rate/Contractility |
Diuretic-Thiazaide-Decrease ciculating volume
Sympatholytics-Beta Blocker-Decrease HR and Contractiltiy Vasodilator-Calcium Channel Blocker- Lower Peripheral Resistance (Renin-Angio-Aldo)- Directed renin inhibitor- decrease sodium retention |
|
|
Describe the different effects these receptors have:
Alpha 1 adrenergic - Alpha 2 adrengergic - Beta 1 adrenergic - Beta 2 adrenergic - |
Alpha 1 - stimulates smooth muscles contraction in vessels thus causes vasocontriction (both arteries and veins)
Alpha 2 - Generally Vasodilation effect, but also causes vasoconstriction (think vessels that need dilation or constriction in a ""fight or flight"" response) Beta 1 - Increase HR and heart contractility Beta 2 - Smooth muscle dilation of airways and vasculature |
|
|
In this pathway:
Renin (Kidney) -----(angiotensinogen)----> Anigotensin I ------(ACE in lungs)------> Angiotensin II Angiotenin II will ______(increase/decrease) thirst, will cause ________(vasodilation/vasocontriction), ______(increase/decrease) aldosterone release which will (increase/decrease) sodium absorption and also _________ (increase/decrease) contractility of the heart. |
1. Increase Thirst
2. Vasocontriction 3. Increase Aldosterone 4. Increase sodium reabsoprtion 5. Increase contractility |
|
|
What factors are normally released by endothelial cells?
And what enzymes increase the release of these factors |
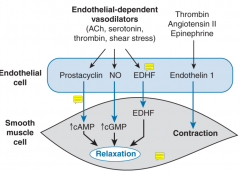
Prostacyclin
NO EDHF All lead to smooth muslces relaxation (ACh, serotonin, thrombin, shear stress) Endothelin 1 leads to smooth muscle contraction (thrombin, angiotensin II epineprine) |
|
|
What happens with dysfunctional endothelial cells?
|

Healthy endothelial secrete prostacyclin and NO which decrease platelet aggregation as well as decrease smooth muscle contraction.
So dysfunctional endothelial cells lead to a decrease in faction that would normally serve to relax smooth muscle cells and factor that prevent platelet aggregation, Also as a double whammy, aggregated plates release factors that lead to smooth muscle contraction |
|
|
Why do we go looking for secondary hypertension?
|
I get it, almost everyone has essential hypertension, but in the cases where the hypertension is secondary it's important to find it.
1. Therapy for SH may be different than EH, leading to excessive medication that will never work 2. if SH is left uncontrolled, adaptive CV changes may develop analogous to those of longstanding EH that could cause the elevated pressures to persist even after the underlying cause is corrected. |
|
|
Causes of hypertension
|
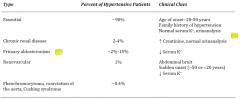
creatinine doesn't have to be super elevated. Creatinine at the high end of normal can indicate 50% renal damage
|
|
|
Where are AII receptors found?
What do they do at each site? What is the single most prominent effect of? |
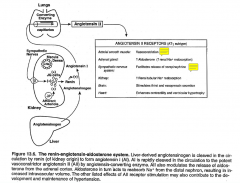
Single most prominent effect is smooth muscle contraction
I shouldn't say it this way the truth is that the substance with the strongest effect on smooth muscle contraction is AII |
|
|
Antihypertensives by class and by physiologic effect
|
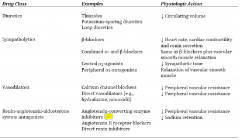
|

