![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
Case 1 Questions (history only, exam next) - |
Amount of menstrual flow, length of menstrual cycle and menstrual period, length of intermenstrual bleeding, pregnant?
Flow is normal, not pregnant, pain a day or two prior to menses, constant pain, turns off quickly, takes tylenol and helps a little bit, mother complains of similar symptoms or has in the past.
Make sure each question connects to a disease mechanism or process. |
|
|
All additional “significant history” is negative Exam:
Labs requested (if any)? |
Normal height and weight throws out chromosomal defects
Tanner 3 = have not gone through adolescence yet (but still normal)
Labs = hematocrit, CBC, TSH Ultrasound, historosalpinogram |
|
|
Lab values reveal normal FSH, serum progesterone and TSH.
Differential?
Any other testing? |
Differential = 1. Pelvic inflammatory disease (probably not with no sexual activity and being cyclical) = chlamydia, gonorrhea
2. Endometriosis = lining of uterus moves to other areas (uterine wall, on the colon, ovaries,
3. Dysmenorrhea |
|

What type of imaging is this? |
Hystrosalpinogram (injection of dye into uterus via cervix)
Abnormal = should not look like a banana shaped = essentially shows |
|
|
Diagnosis? |
Bicornate uterus |
|
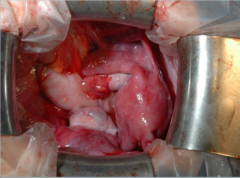
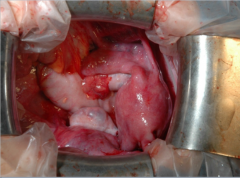
Identify uterus, colon, and left ovary, pouch of Douglas, oviduct |
|
|
Notice the abnormalities. |
Flat then bulging up, has had this condition since she was born. |
|

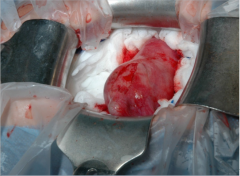
Squeezing incision, push out mass with blood.
What is it? |
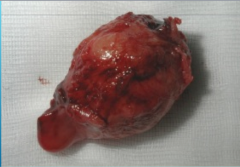
Non-communicating uterine horn. |
|
|
Case 2
Additional history? |
Height and weight No contraceptives No significant stress Some changes in weight Mother went through menopause at 50
|
|
|
No breast leakage Differential Dx? |
Breast = PROLACTING Headaches = PITUITARY LESIONS, CRANIOPHARYNGIOMA Weight = OBESITY OR THYROID Medication = ANTI-DEPRESSANTS Exercise = intense exercise can have effects No hormonal contraception |
|
|
Exam General exam negative Differential? |
Thyroid, polycystic ovarian syndrome, etc. NORMAL EXAM
Order FSH, LH, TSH, |
|
|
Hypothyroidism
Weight gain, reflexes, hair loss, skin changes, etc. |
|
|
Case 3 55 yo woman presents on referral from primary care for vaginal bleeding. Other than CBC, which was normal, no other eval has been undertaken. Healthy, no medications except daily aspirin for heart health.
Additional history? |
When was your last normal menstrual period? When were they last normal and regular? How much aspirin is she taking? Any risk factors? Any HRT? Smoke? Family history of cancer? Abnormal PAP smear? |
|
|
3 children, all C/S, last with tubal ligation at age 34. No other gyn surgeries. No pain. Regular menses q 28 d, lasting 4 d, until uneventful menopause age 48 (smoker). She is quite sure this is vaginal bleeding, not GI. Starting age 17 and between C/S she used OCPs. Never obese, breastfed each child 6 months. VS normal; General exam is negative, pelvic exam is negative. Differential? Lab tests? |
Birth control pills have elevated protection for OVARIAN cancer. Lack of children, lack of breast feeding = ENDOMETRIAL CANCER?
Post-menopausal bleeding = always do endometrial biopsy (it was negative) |
|

What does patient have?
What are the chances this is cancer? |
Uterine polyp = bleeding
1/50 chance of being cancer |
|
|
Case 4. Additional history? |
Continue |
|
|
Pathology on ovaries – bilateral dermoid cysts (benign teratomas are 15% bilateral). Spotting is not cyclic or predictable, occasionally heavy. No pain
CBC – not anemic, normal
Exam – very thin, NAD. NEFG, thin, pale vaginal mucosa. Scant blood per cervical os. Uterus small. No adnexal masses.
Lab tests? |
Thin woman reduces risk of ovarian cancer
|
|
|
Ultrasound – very thin to absent endometrial stripe.
EMB – scant tissue, no hyperplasia or cancer
Diagnosis? Recommended treatment? |
Scant tissue = uterine atrophy => bleeding in post menopausal patient
Mechanism = no estrogen (lack of estrogen for 20 years) |
|
|
Case 5 Husband eval has been done – normal sperm motility, normal count. |
Diagnosis of infertility because they have been trying.
Husband is normal (not the cause). |
|
|
Exam Differential? Labs? |
Hair distribution, acanthosis nigricans = PCOS Other unlikely options = primary adrenal tumor, diabetes, craniopharyngioma, etc.
Labs = FSH, LH (probably not important because it is too expensive) = neither of these will help in diagnosis
Need to look for androgens (testosterone and DHEA, prolactin sometimes but rarely) |
|
|
TSH 2.2 Other test needed? |
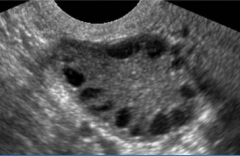
Ultrasound! Look for the "string of pearls." |
|
|
What are the hormonal issues here? |
We don't really know
Possibility: Overactive CYP 450 (17-alpha --OH) |

