![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
Renal failure
-define |
-state of decreased renal function that allows persistent abnormalities (renal azotemia and inability to concentrate urine) to exist
-loss of 75% of nephrons |
|
|
Renal failure
-aka |
-Renal azotemia
|
|
|
Renal failure
-types |
-acute
-chronic |
|
|
Acute Kidney Disease
-characteristics |
-history of ischemic or toxic insult
-normal or increased Hct -swollen kidneys -hyperkalemia/acidosis especially with oliguria -active urine sediment/normoglycemic glucosuria -good body condition -relative severe signs for level of dysfunction -US usually normal |
|
|
Chronic Kidney Disease
-characteristics |
-long history of renal disease or PU/PD
-nonregenerative anemia -small, irregular kidneys -normal or hypokalemia -less severe acidosis -inactive urine sediment -poor BCS/history of weight loss -relatively mild signs for level of dysfunction -US = dense renal cortices, loss of C/M junction |
|
|
Acute kidney injury
-causes |
usually ischemic or toxic insult
Toxicants: -ethylene glycol -amphotericin -aminoglycosides -cisplatin -NSAIDs Ischemia: -hypotension -hypovolemia -prolonged/deep anesthesia -heat stroke -DIC Miscellaneous: -Immune mediated -hypercalcemia -leptospirosis -lyme disease |
|
|
Acute kidney injury
-risk factors that we have less control over |
-fever
-sepsis -advanced age -Stage 1/Early stage 2 CKD -liver disease -cardiac disease -neoplasia |
|
|
Acute kidney injury
-risk factors that we have more control over |
-dehydration
-hypokalemia -excessive dose/duration -adverse drug combinations -prior use of aminoglycosides -anesthesia |
|
|
Acute kidney injury
-most adverse risk factor |
-dehydration
|
|
|
Acute kidney injury
-affect of multiple risk factors |
-typically additive
|
|
|
Acute kidney injury
-when is increased monitoring needed for patients at risk? |
-anesthesia
-drug administration |
|
|
Acute kidney injury
-what is monitored in patients under anestheia who are at risk |
-hydration status
-blood pressure -cardiac output -urine production |
|
|
Acute kidney injury
-what is monitored in patients administered drugs who are at risk |
-casts/renal epithelial cells
-normoglycemic glucosuria -enzymuria -plasma drug concentrations |
|
|
Acute kidney injury
-early recognition urinalysis |
-granular cysts
-renal epithelial cells -cellular debris -normoglycemic glucosuria -tubular proteinemia -enzymuria |
|
|
Acute kidney injury
-appearance of renal epithelial cells on a stained slide |
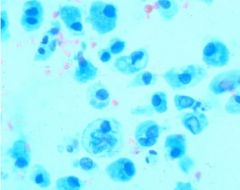
-fusiform
-spindle shaped -bi/tri nucleated -eccentric nuclei |
|
|
Acute Kidney Injury
-how is it potentially reversible |
-nephron repair and compensatory hypertrophy
|
|
|
Acute kidney injury
-goal of treatment |
-buy time for repair and compensation
|
|
|
Acute kidney injury
-treatment |
-discontinue all potentially nephrotoxic drugs (mjeasures to decrease absorption of drugs as well i.e. vomiting, charcoal)
-Start specific antidotal therapy if applicable (ex. alcohol dehydrogenase inhibitors for ethylene glycol) -Identify and treat and prerenal or postrenal abnormalities -Start IV fluid therapy (helps buy time for nephron compensation) -assess volume of urine production -correct acid-base and electrolyte abnormalities (rule out hypercalcemia nephropathy) -diuretics to increase urine volume if necessary (furosemide, mannitol) -consider potential dialysis (if no response) biopsy kidney at time of dialysis catheter placement |
|
|
Acute Kidney injury
-how much IV fluid do you want to provide |
-maintenance and continuing fluid loss
|
|
|
Acute kidney injury
-when can overhydration be a problem -what can happen |
-oliguria/anuria
-can lead to pulmonary edema |
|
|
Ethylene glycol ingestion
-3 stages |
1) central nervous
2) cardiopulmonary 3) renal` |
|
|
Ethylene glycol ingestion
-prognosis |
-treatment in Stage 1 = successful
-treatment in stage 3 = grave |
|
|
Ethylene glycol ingestion
-early clinical signs |
-ataxia and other CNS deficits
-vomiting -PU/PD metabolic acidosis with an increased anion gap -hyperosmolarity with an increased osmolal gap -increased EG in serum and urine |
|
|
Ethylene glycol ingestion
-late signs |
-calcium oxalate crystalluria
-azotemia |
|
|
Chronic kidney disease
-secondary to what in dogs |
-glomerular disease
|
|
|
Chronic kidney disease
-caused by what in cats |
-tubulointerstitial disease
|
|
|
Effect of irreversible damage to a nephron
|
-entire nephron is rendered nonfunctional
-subsequent healing with replacement fibrosis |
|
|
Chronic kidney disease
-goals of treatment |
1) identify and treat the primary disease process
2) slow down progressive nature of the disease 3) alleviate patient symptoms |
|
|
Chronic kidney disease
-stages |
1) non-azotemic
2) mild renal azotemia 3) moderate renal azotemia 4) severe renal azotemia |
|
|
Chronic kidney disease
-causes |
Immunologic
-glomerulonephritis -SLE -amyloidosis Tubulointerstitial inflammatory disease -pyelonephritis -renoliths -leptospirosis Neoplasia Systemic hypertension Congenital/hereditary disorders: -hypoplasia/dysplasia -polycystic disease -familial nephropathy Idiopathic |
|
|
Chronic kidney disease
-diagnosis of stage 1 based on |
-persistent proteinuria
-urine concentrating deficits -increase in serum creatinine (remains in normal range) -abnormal renal pallpation/ultrasound |
|
|
Chronic kidney disease
-diagnosis of stages 2-4 based on |
-persistent azotemia superimposed on the inability to concentrate urine
|
|
|
Chronic Kidney Disease
-Renal Proteinuria considered abnormal |
> 0.4/0.5
|
|
|
Chronic Kidney Disease
-Blood pressure vs. Risk of future target organ damage |
-Minimal: S=<150; D=<95
-Mild: S=150-159; D=95-99 -Moderate: S=160-179; D=100-119 -Severe: S=>180; D=>120 |
|
|
Chronic Kidney Disease
-Treatment |
-Discontinue all potentially nephrotoxic drugs
-Identify and treat any prerenal or postrenal abnormalities -Rule out and treat any treatable primary causes of renal disease (pyelonephritis, renoliths, renal LSA) -Measure Blood Pressure (systemic hypertension common) -Initiate dietary therapy (CKD diet) -Treat vomiting/gastroenteritis if possible -Treat anemia if present -Provide caloric requirements (70-100 kcal/kg/day) |
|
|
Chronic Kidney Disease
-how to treat systemic hypertension |
-Dog: ACE-inhibitor
-Cat: Ca channel blocker |
|
|
Chronic Kidney Disease
-dietary therapy components |
-reduced quantity but increased quality protein
-restricted phosphorus -N-3 polyunsaturated fat supplement -reduced sodium -alkalinizing agent |
|
|
Chronic Kidney Disease
-treating vomiting/gastroenteritis |
-Metoclopramide
-Trimethobenzamide -Chlorpromazine -H2 receptor blockers |
|
|
Prioritization of diagnostic and therapeutic efforts in CKD
|
Stage 1 & 2:
-ID and treat primary disease process Stage 2 & 3: -slow disease progression with renoprotective treatment (diet, phosphate binders, ACE-inhibitors) Stage 3 & 4: -alleviate patient symptoms (anorexia, vomiting, anemia) |
|
|
Prognosis for Acute Kidney Injury and Chronic Kidney Disease
-depends on |
-severity of dysfunction
-response to treatment -ability to control GI signs -Renal histology |
|
|
Most important component of AKI/CKD prognosis
|
-response to treatment
|
|
|
Which of the following is most likely to be a risk factor for acute renal failure due to ischemia?
-pre-existing renal disease -hypernatremia -hypothermia -acidosis -hyperkalemia |
-pre-existing renal disease
|
|
|
Which of the following is not compatible with a diagnosis of chronic kidney disease?
-a long history of PU/PD and weight loss -an inactive urine sediment -decreased renal cortical echogenicity on ultrasound -nonregenerative anemia -relatively mild clinical signs for the degree of azotemia |
-decreased renal cortical echogenicity on ultrasound
|
|
|
Why is anemia not normally seen with Acute Kidney Injury?
|
-long life of RBCs (120 days)
|

