![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
86 Cards in this Set
- Front
- Back
|
This is an atrial impulse that is conducted with delay or fails to conduct to the ventricle at a time when the AV node should not be refractory.
|
AV heart block
|
|
|
What are the four types of AV heart blocks?
|
1st degree heart blocks
2nd degree heart block, Mobitz Type I (Wenckebach) 2nd degree heart block, Mobitz Type II 3rd degree heart block |
|
|
The etiology of this includes increased vagal tone, drug effect, electrolyte abnormalities, ischemia or conduction system disease.
|
1st degree heart block
|
|
|
The symptoms of this are usually asymptomatic, but may exacerbate heart failure.
|
1st degree heart block
|
|
|
What do you see when you are diagnosing a 1st degree heart block
|
Constantly long PR interval (> 0.2 seconds)
|
|
|
What is the treatment for 1st degree heart block?
|
No Tx, or if patient is symptomatic and in absence of underlying treatable causes - place dual chamber pacemaker.
|
|

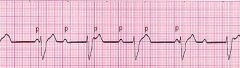
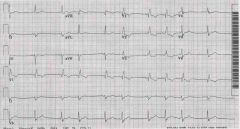
What is this displaying?
|

First degree heart block
|
|
|
What are two other names for 2nd degree heart block?
|
Mobitz Type I / Wenckebach
|
|
|
What is the etiology of 2nd degree heart block - Mobitz I / Wenckebach?
|
Increased vagal tone, antiarrhythmic drugs, electrolyte abnormalities, ischemia or conduction system disease.
|
|
|
What are the symptoms of 2nd degree heart block - Mobitz Type I / Wenckebach?
|
Usually asymptomatic, but can see lightheadedness, dizziness, syncope
|
|
|
If you see progressive PR interval prolongation (or variable PR intervals) before atrial impulse is blocked and QRS is dropped what would you diagnose?
|
2nd degree heart block - Mobitz Type I / Wenckebach
|
|
|
How do you treat 2nd degree heart block - Mobitz Type I / Wenckebach?
|
1. Usually benign, does not develop into complete heart block.
2. If symptomatic: Initially Atropine 0.5 IV q2min to max of 0.04 mg/kg 3. For persistent Sx, permanent pacemaker |
|

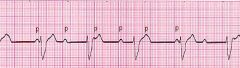
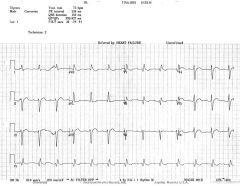
What is this representing?
|

2nd Degree Heart Block - Mobitz Type I / Wenckebach
|
|
|
What is the etiology of 2nd degree heart block - Mobitz Type II?
|
Includes conduction system dz, antiarrhythmic drug effect, MI (usually ant distribution), and increased vagal tone.
|
|
|
What are the symptoms of 2nd Degree Heart Block - Mobitz Type II?
|
Since this block often antecedes development of complete heart block, Sx include fatigue palpitations, lightheadedness and syncope.
|
|
|
How do you diagnose a 2nd degree heart block - Mobitz type II?
|
1. Abrupt AV conduction block without e/o conduction delay in preceding conducted impulses.
2. This type of AV block often progresses to complete (third degree) heart block! |
|
|
What is more common, Mobitz Type I or Type II?
|
Benign Mobitz Type I is more common.
|
|

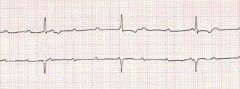
What does this represent?
|

2nd degree heart block - Mobitz Type II
|
|
|
How do you treat 2nd degree heart block - Mobitz Type II?
|
Pacemaker implantation (even in asymptomatic Pts because of risk of developing complete heart block).
|
|
|
This is when all atrial impulses fail to conduct to the ventricle and the prevailing ventricular escape rhythm is slower than the atrial rate.
|
3rd degree heart block
|
|
|
The etiology of this is ischemia or infarction, drug toxicity, idiopathic degeneration of the conduction system, infiltrative dz (amyloidosis, sarcoidosis, mets), rheum d/o (polymyositis, scleroderma, rheumatoid nodules), infectious d/o (lyme dz), calcific AS or endocarditis.
|
3rd degree heart block
|
|
|
What is something that is always the case in third degree heart block?
|
The QRS, or ventricular rate, is always slower than the P wave.
|
|
|
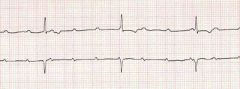
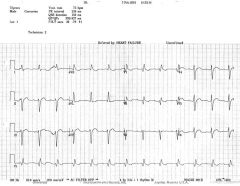
What is this?
|
3rd Degree Heart Block
|
|
|
What is this?
|
3rd Degree Heart Block
|
|
|
What is this?
|
3rd Degree Heart Block
|
|
What is this?
|
3rd Degree Heart Block
|
|
What is this?
|
3rd degree heart block
|
|
|
What are the symptoms of third degree heart block?
|
1. Depend on degree of bradycardia
2. May include lightheadedness, dyspnea, CHF, angina, syncope |
|
|
What is the TX of 3rd degree heart block?
|
Permanent pacemaker
|
|
|
This is when there is a rhythm in which atrial and ventricular activation occurs from different pacemakers. Atrial rhythm can be of sinus origin or from any atrial arrhythmia. Ventricular activation may be from either junctional or lower pacemakers.
|
Atrioventricular dissociation
|
|
|
In this, the atrial and ventricular rate are usually the same.
|
In AV Dissociation
|
|
|
3rd degree heart block is a special form of what?
|
AV dissociation
|
|
|
When you see PR Interval > 0.20 sec and constant.
|
1st degree heart block
|
|
|
If the PR is getting longer and longer (or varies) until the QRS is completely dropped.
|
2nd degree heart block, Mobitz Type I, Wenckebach.
|
|
|
If there is no PR prolongation, QRS just suddenly dropped.
|
2nd degree heart block, Mobitz Type II
|
|
|
P and QRS are completely asynchronous, ventricular rate is much slower.
|
3rd degree heart block.
|
|
|
This is when there are blocks within ventricular bundles, normally consist of a L or R bundle branch block. Can effect entire ventricular bundle or a fascicle of the L bundle.
|
Bundle branch blocks
|
|
|
What is not serious in itself, but it may indicate significant heart damage due to something such as a previous MI?
|
Right BBB
|
|
|
this is more serious, in older people, it often indicates heart dz due to HTN or atherosclerosis.
|
Left BBB
|
|
|
What is more common, RBBB or LBBB?
|
Left BBB
|
|
|
What are the Sx of bundle branch blocks?
|
Usually asymptomatic, possibly syncope or presyncope (if both bundles effected)
|
|
|
Bundle branch blocks have what kind of feature?
|
"Bunny Ears"
|
|
|
How do you diagnose RBBB and LBBB?
|
R-R' wave
QRS wider than 0.12 seconds |
|
|
This represents 2 superimposed QRS complexes from each ventricle, spiking separately but very close in time to each other. In LBBB, the LV firing is delayed. In RBBB, the RV firing is delayed.
|
R-R' wave
|
|
|
In RBBB, the R wave represents the LV depolarization, while the R' wave represents the delayed RV response. In LBBB, the R wave represents the RV and the R' represents the LV depolarization.
|
QRS wider than 0.12 seconds (3 small boxes)
|
|
|
What leads does RBBB usually show up in?
|
V1 and V2
|
|
What is this?
|
Right bundle branch block
|
|

What is this?
|

Right Bundle Branch Block
|
|
|
How do you diagnose a RBBB?
|
1. Secondary R wave in lead V1
2. Wide QRS >0.12 sec (3 small boxes) |
|

What is this?
|

LBBB
|
|
What is this?
|
LBBB
|
|
|
How do you diagnose a LBBB?
|
Secondary R wave in a LBBB is best appreciated in leads V5-V6
Wide QRS, more than 0.12 sec (3 small boxes) |
|
|
How do you treat BBB?
|
1. Often no tx needed in RBBB, reevaluate periodically
2. Treat underlying disorder (ie. HTN) 3. Packemaker (if brady after MI) 4. Cardiac resynchronization treatment (CRT) - paces both ventricles at the same time (in dilated cardiomyopathy) |
|
|
BBB increases mortality with Pt with?
|
MI
|
|
|
This makes diagnoses of other cardiac disease more complicated?
|
BBB
|
|
|
With this, there is a greater risk of CHF and sudden death?
|
LBBB
|
|
|
This occurs when you have a normal QRS width (or just slightly prolonged)
QRS morphology is significant |
Hemiblocks
|
|
|
With this you see an EKG with a Tall R in 1 plus a deep S in aVf (left axis deviation)
additional criteria for this is a Q wave in lead 1, an S wave in lead 3 or aVf |
Left Anterior Hemiblock
|
|
|
With this you see a Deep S in lead 1 plus a tall R in aVf (R axis deviation), Additional criteria includes an S wave in lead 1, a Q wave in lead 3 or aVf.
|
L Posterior Hemiblock
|
|
What is this showing?
|
Left Anterior Hemiblock
|
|
|
What is this showing?
|
Left anterior hemiblock
|
|

What is this showing?
|
Left posterior hemiblock
|
|
|
A bifasicular block is present if?
|
RBBB +
L ant BBB or L post BBB |
|
|
What does it mean when there is only 1 fasicle conducting properly, and if that fasicle is intermittently blocked it leads to what?
|
Mobitz type II which leads to AV dissociation.
|
|
What is this?
|
Bifascicular block
|
|
|
This is present if you have prolonged PR (1st degree AV block) + RBBB + Either L ant or L post BBB
|
Trifascicular block
|
|
|
If you see alternating LBBB and RBBB it can mean what?
|
Trifascicular block
|
|
What is this?
|
Trifascicular block
|
|
|
This originates from the right side of the aorta, divides into the marginal artery and the posterior interventricular artery, supplies RA and RV, inf and posterior wall of LV and post 1/3 of interventricular septum, as well as SA and AV nodes.
|
Right main coronary artery
|
|
|
This originates from the left side of the aorta, divided into the anterior descending and circumflex, the anterior descending artery supplies the anterior surface and lateral surface of LV and anterior 2/3 of interventricular septum as well as RBB and LBB, the circumflex A supplies LA, anterolateral, posterolateral, and post. wall of left ventrical, as well as SA and AV nodes.
|
Left main coronary artery
|
|
|
This is caused by atherosclerosis in 90% of cases.
|
Coronary artery disease
|
|
|
This is a progressive process of obstruction and hardening of the artery wall.
|
atherosclerosis
|
|
|
This is a deprivation of 02 and nutrients to the myocardium.
|
Myocardial ischemia
|
|
|
What are the causes of myocardial ischemia?
|
Atherosclerosis, vasospasm, thrombosis, embolism, decreased ventricular filling time (in tachycardia), and decreased filling pressure in coronary arteries (in severe hypotension or aortic valve disease).
|
|
|
What is a symptom of ischemia?
|
Pain - Angina
|
|
|
Tissue damage is ________ in ischemia?
|
Reversible
|
|
|
This is the degree of cellular damage beyond ischemia.
|
Myocardial injury
|
|
|
This occurs if blood flow is not restored within a few minutes, and/or if blood flow is not restored tissue death ultimately occurs.
|
Myocardial injury
|
|
|
This is when there is a death of injured myocardial cells?
|
Myocardial infarction.
|
|
|
When you have myocardial infarction tissue damage is _________ ?
|
Not reversible
|
|
|
What EKG changes do you see with an MI?
|
T wave peaking or inversion
ST elevation or depression Significant Q waves (> .04 sec and 1/2 of QRS), new Q waves |
|
|
How can you tell if an MI is an anterior MI?
|
changes will be seen in leads V1-V4 (LAD occluded)
|
|
|
How can you tell if an MI is a septal MI?
|
changes will be seen in leads V1-V3
|
|
|
How can you tell if an MI is a lateral MI?
|
Changes in I, aVL (and V5, V6) (LAD occluded)
|
|
|
How can you tell if an MI is a inferior MI?
|
Changes in II, III, and aVf (right coronary artery occluded)
|
|
|
What is seen with a posterior MI?
|
Large R wave and upright T wave, ST depression will be seen in V1 or V2 - (right coronary artery occluded)
|

