![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
Explain foetal, maternal and placental factors affecting foetal growth
|
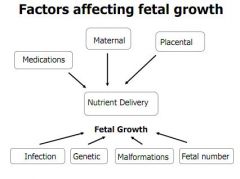
Maternal factors include blood flow, O2 capacity, nutrition, toxins like smoking and alcohol and age of mother.
Placental factors include surface area for exchange, blood flow and concentration of substrates Foetal factors include infections like CMV or Rubella, genetic factors, malformations and also the number of foetuses |
|
|
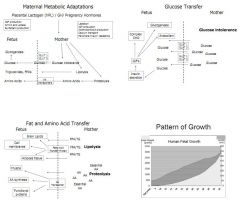
Describe the nutritional importance of maternal factors: Glucose, AAs and FFAs and TAGs
|
|
|
|
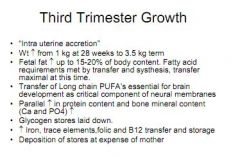
Describe the change in foetal weight seen in the third trimester
|
|
|
|
Describe the change in foetal weight seen in the third trimester
|
|
|
|
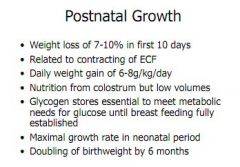
Describe changes in postnatal growth
|
|
|
|
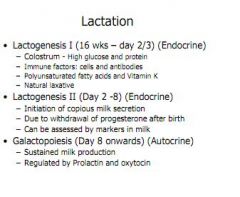
Outline the three stages of lactation
|
|
|
|
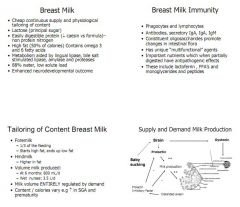
Explain why breast milk is so important, its role in immunity, how its contents are altered, and what stimulates production.
|
|
|
|
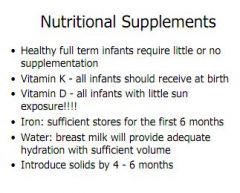
Explain the requirements for supplementation of diet in the neonate
|
|
|
|
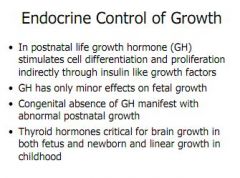
Explain the role of growth hormone and thyroid hormones in the foetus and neonate
|
|
|
|
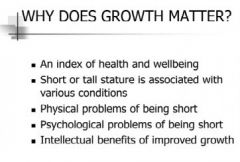
Give reasons why growth matters
|
|
|
|
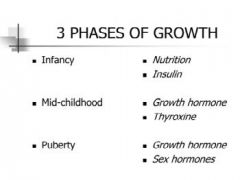
What are the 3 phases of growth and what hormones drive them
|
|
|
|
Explain growth hormone and its role in childhood development
|
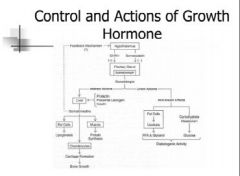
Growth hormone is the major determinant of childhood growth and also plays a big role in adolescent growth.
It acts through IGF-1 (liver) Secreted at night in pulses |
|
|
What are some tests for stimulating GH and why are they no good sometimes?
|
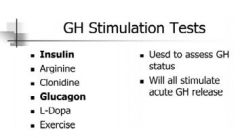
Non-physiological, and not very sensitive or specific
|
|
|
What is a growth chart? Give some relevant info about them
|
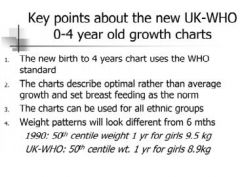
Compares a child's growth to a reference population
Shows centiles placed at 0.4, 2, 9, 25, 50, 75, 91, 98, and 99.6 Describe optimal weight for a breastfed child Can be used across ethnicity |
|
|
What is growth tempo, what factors determine it, and how is it best measured?
|
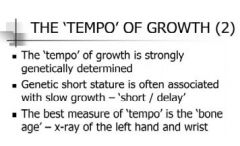
Growth tempo varies from child to child, will change over time, and is influenced by weight, with overweight children growing quicker and underweight children growing slower.
It is strongly influenced by genetics. Best measure is a 'bone age' done with an x-ray of the left wrist - this looks at the growth plates and appearance of bone, which can be plotted against 'norms' to place a childs bone age within a centile |
|
|
What is puberty staging?
|
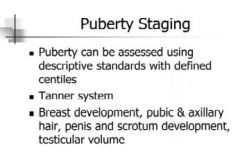
Tanner system, compares breast, testes and pubic hair development and classes them into 5 groups/stages.
|
|
|
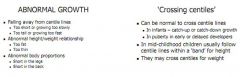
What is classed as abnormal growth, and when is crossing centiles ok?
|
|
|
|
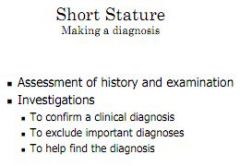
What investigations might you perform when looking at short stature?
|
|
|
|
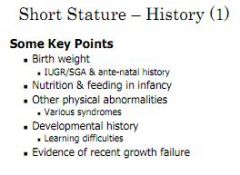
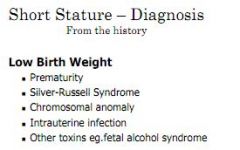
What factors might cause low birth weight and what is Silver Russel?
|
Silver Russell is a type of dwarfism, shown by a failure in pre-natal growth, with no catch up after birth.
Limb assymmetry, curved in 5th finger, and small triangular face. |
|
|
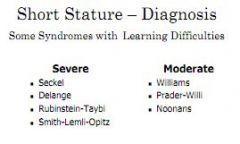
What factors might be relevant in a social history and what growth conditions affect IQ?
|
Abuse and neglect influence growth.
Some congenital growth defects have associated IQ pathology: Severe: Seckel, Delange, Rubinstein, Smith-Lemli-Opitz Mild: Williams, Prader-Willi, Noonans |
|
|
When diagnosing short stature, how can it be classified and what conditions might you be looking out for in each case?
|
Short and fat:
Endocrine?, GH?, Cushings? Short and thin: Disease (CVS, Renal, Metabolic, Coeliac), Neglect, Malnutrition Short and disproportioned: Short legs - Hypothyroid, Rickets, Turners Short spine - Spondyloepiphyseal Dysplasia, Scoliosis Long legs: Klinefelters |
|
|
Bone age can indicate what if advanced, normal, delayed or severely delayed?
|
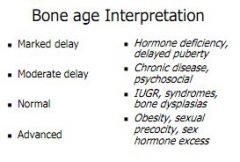
|
|
|
Define turners
|
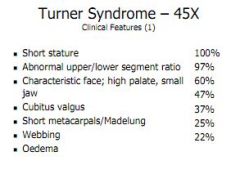
+ Gonadal failure
+ CVS abnormalities + Naevi |
|
|
Who is delayed puberty more commonly seen in? And how is it treated?
|
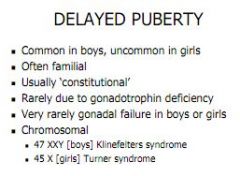
|
|
|
What are some causes of tall stature and what are some signs?
|

|
|
|
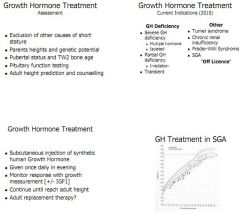
How would you treat a growth hormone deficiency?
|
|
|
|
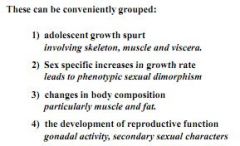
What four factors characterise changes at puberty?
|
|
|
|
What is the first stage of puberty and how does it affect hair growth?
|

Adrenarche occurs around 6-8 years, marks secretion of adrenal hormones.
Low levels = axilla and pubes Testes secrete higher levels = facial hair |
|
|
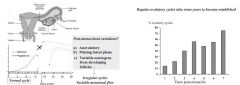
Post menarche what happens to menstrual cycles and for how long?
|
|
|
|
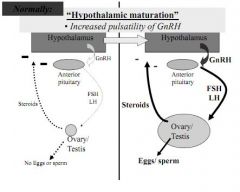
What happens at puberty to the hypothalamus?
|
|
|
|
The loss of oocytes which symbolises the menopause also causes a loss of oestrogen. What symptoms are associated with this?
|
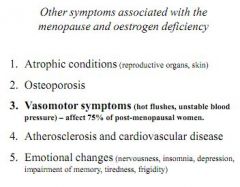
|
|
|
Describe the affects of ageing on female and male reproductive ability.
|
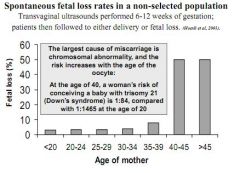
In men, the ability to produce sperm by mitosis continues almost throughout life.
In older age, deficiencies in testosterone will impair libido and sexual function. Sperm quality will be less. In women, reproductive ability is strongly age linked. Women aged <26 will conceive in 50% of cases after intercourse 2 days before ovulation. That rate drops to 40% in 27-34 year olds, and 25% in 35 to 39 year olds. Older pregnancy is associated with a greatly increased risk of miscarriage (10% <39, versus 50% >40), and Down's syndrome (1:1500 at age 20, versus 1:84 at age 40) |
|
|
Summarise learning ability in a newborn
|

|
|
|
What is PIAGET staging, what are the four concepts and 4 stages and when is it relevant?
|

Piaget was a developmental psychologist and his stages of thought development are useful for assessing a child's thought development.
It describes a mode of thinking based on the childs ability to produce schema (collections of thought concepts), and then assimilate new info into that schema. Later, if info presents itself which does not fit into the schema, the child must accomodate that info, either by modifying the schema, or developing a whole new one. Equilibrium is reached when assimilation and schema are in balance. |
|
|
How does motor ability develop?
|

|
|
|
How does perception develop?
|
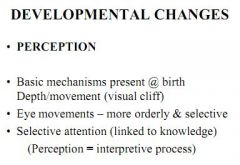
|
|
|
What is attachment theory?
|
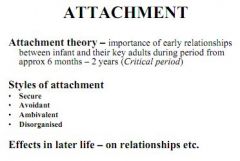
|
|
|
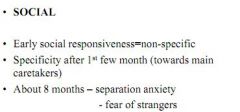
How does social behaviour develop?
|
|
|
|
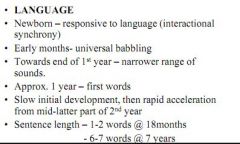
How does language develop?
|
|
|
|
What is sexual identity and what factors define it?
|
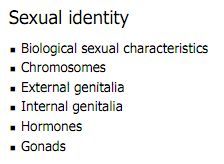
What makes boys boys and girls girls. So your biological sexual characteristics, your chromosomes, your genitals and the hormones you are influenced by.
|
|
|
What is gender identity?
|
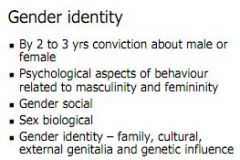
|
|
|
What is sexual behaviour?
|
|
|
|
Factors influencing psychosexual behaviours
|
|
|
|
Give some information on sexual behaviour based on studies
|
Average age of first intercourse is getting younger, now 17 (compared to 21 years ago).
Number of partners varies a lot. 65% of people have 0-1, 1% of men >22, and 1% women >8 The frequency of intercourse is median of 5 per month (1 per week) |
|
|
Why are sex and releationships important?
|
|
|
|
What are the commonest sexual problems in men and women and what underlies these problems?
|
Men: Libido, erectile dysfunction and premature ejaculation
Women: Libido, anorgasmia and dysparunia (pain on intercourse) Erectile dysfunction is the commonest sexual issue in men, and the problem gets worse with age (57% of over 70 year olds), can be physical or psychological. Treatment depends on cause. PD5 inhibitors. Premature ejaculation is another big one. Treat with stop/start, or a cock ring or SSRI In women, libido can be linked to anger at lack of respect, poor partner technique, depression or child birth. Can also be physical e.g. Hyperprolactinaemia |
|
|
What is the Pearl index, how is it calculated and what can it tell us about unprotected sex at age 20 and 40?
|
Total accidental pregnancies x 1200 / Total months of exposure = Failure Rate / Hundred Woman Years
At age 20, you would get 80-90 failures per 100 woman years At age 40, you would get 40-45 failures per 100 woman years |
|
|
Discuss the relative merits of barrier contraception with strengths and weaknesses.
|
Barrier: Condom, female condom, diaphragm, cap
Effective, cheap, safe, easy to use Effectiveness varies from 97% male condom with perfect use, to 85% cap with normal use. Technique is vital, and even with perfect technique, the best barrier method still has a 2-3% failure rate. No side effects. |
|
|
Discuss the relative merits of the hormone contraceptive pills with strengths and weaknesses.
|
Hormone: Oral contraceptive pill, Progesterone Only Pill (POP),
Highly effective - 99%+ in each case, cheap, safe, easy. Different methods of action: Mixed pill blocks FSH and LH, stopping mucus changes, blocking LH surge and stopping follicle maturation. But affected by antibiotics and liver enzyme tablets. Also causes nausea, bleeding, low libido and low mood Progesterone only works by cross-linking cervical mucus, stopping endometrial maturation. Doesn't necessarily prevent ovulation though. But good on anti-biotics. Can cause cysts and ectopic pregnancies. |
|
|
Discuss the relative merits of the implant and injection with strengths and weaknesses.
|
Also 99%+ effective.
The progesterone only injection works for 12 weeks. It inhibits ovulation (unlike the POP) and effects mucus and endometrium. It is not rapidly reversible, which is an issue, and can cause weight gain, but is good in breastfeeding and with antibiotics and enzyme inducing drugs The implant lasts 3 years, is >99% effective, brings about anovulation + mucus thickening + endometrial advantages, but can cause headaches - should not be used with enzyme inducing drugs |
|
|
Discuss the merits of the morning after pill and IUD
|
Morning after pill is a progesterone only tablet which is effective up to 5 days after sex, although success declines rapidly from 95% within 24 hours, to 58% after 2 days.
Delays egg release, inhibits implantation, and may also affect sperm. The Copper IUD can be used 5 days after ovulation or 5 days after UPSI (99.9% effective) Directly toxic to sperm and egg, lowers penetration of sperm and causes inflammation which prevents implantation. But can cause a heavier initial period, perforation and ectopic pregnancy |
|
|
Explain the hormone IUD (Mirena)
|
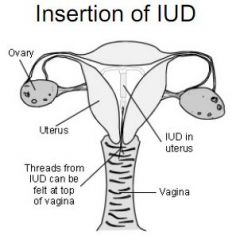
This is a progesterone coil, inserted as a normal IUD.
Changes cervical mucus and cervix endometrium. 75% continue to ovulate. Good with breastfeeding, can cause cysts. |
|
|
Describe male and female sterilisation.
|
Male - snip the Vas.
Female - snip the fallopian tubes. |
|
|
Describe contraceptive issues for the following:
Woman on antibiotics Woman on enzyme inducing drugs Breastfeeding mother Woman at risk of cysts/ectopic pregnancy Woman who wishes to keep ovulating Woman who doesn't want to take tablets Woman worried about her weight Woman who had unprotected sex 4 days ago Woman who had unprotected sex yesterday Woman at risk of osteoporosis |
Woman on antibiotics - Don't take normal pill, try POP, injection or implant
Woman on enzyme inducing drugs - Only try Depoprovera injection (not POP, normal pill or implant) Breastfeeding mother - Depoprovera injection Woman at risk of cysts/ectopic pregnancy - Avoid IUD Woman who wishes to keep ovulating - Mirena IUD Woman who doesn't want to take tablets - Injection/implant Woman worried about her weight - Barrier/POP (weight affects transient) Woman who had unprotected sex 4 days ago - Coil Woman who had unprotected sex yesterday - POEP Woman at risk of osteoporosis - Avoid injection |
|
|
What is the menopause, when does it happen and how is it diagnosed?
|
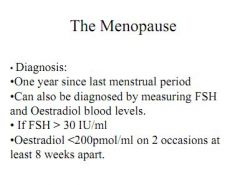
Defined as the last period, retrospectively after 1 year without a period
Happens around 50 (later in Japan), under 45 and it is early. Diagnosed anecdotally (last period, over 1 year ago), or by measuring FSH/Oestradiol FSH >30iu/ml and Oestradiol <200PMOL/ml on two separate occasions 8 weeks apart. |
|
|
What are the 6 principles for HRT therapy?
|

|
|
|
Is HRT contraception?
|
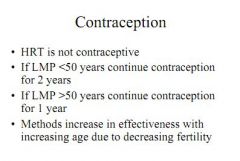
No!
|
|
|
What are the current prescribing guidelines for HRT?
|
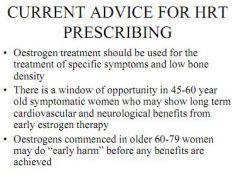
Oestrogen should be used for specific symptoms and low bone density
Good long term benefits on CVS and neurological benefits from early oestrogen therapy in patients 45-60. In older patients 60-79 you might do more early harm before benefits are achieved Give lowest dose possible to achieve effect. |
|
|
What are the risks of HRT?
|
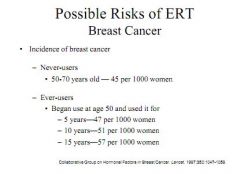
Increased risk of ovarian cancer with prolonged use
Increased risk of dementia with prolonged use Increased risk of breast cancer (+0.02% over 5 years, 0.06% over 10 years, and 0.12% over 15 years) |
|
|
What are the risks of HRT?
|
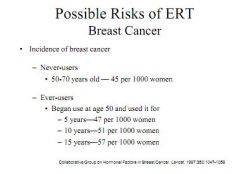
Increased risk of ovarian cancer with prolonged use
Increased risk of dementia with prolonged use Increased risk of breast cancer (+0.02% over 5 years, 0.06% over 10 years, and 0.12% over 15 years) Increased risk of venous thrombosis and endometrial hyperplasia (reduced by progestagen) |
|
|
Why might you need to replace androgens with HRT and what benefits is this said to give?
|

Testosterone binds to SHBG (sexual hormone binding globulin)
Ostrogen raises levels of SHBG, so HRT causes decrease in testosterone levels |
|
|
What are the benefits of HRT?
|
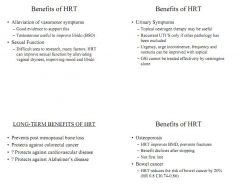
Increases lipoprotein levels (HDL), blood flow, and reduces inflammation, all improving CVS outcomes.
Menopause associated with raised risk - also add lifestyle measures Also good for osteoporosis as improves bone density (with lifestyle measures) Good for lowering colorectal cancer risk Alleviates vasomotor symptoms, urogenital symptoms, improves sexual function (moist vadge?) |
|
|
What are the major menopausal symptoms?
|
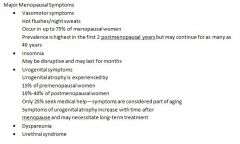
|

