![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
144 Cards in this Set
- Front
- Back
|
integumentary system physiological changes during pregnancy
|
estrogen induced vascular and pigment changes
increased pigmentation = chloasma and linea nigra striae gravidarum (stretch marks) increased sebaceous and sweat gland activity palmar erythema angomas--vascular spiders |
|
|
alterations affecting comfort rest mobility musculoskeletal system
|
progesterone, estrogen, and relaxin induced relaxation of joints, cartilage, and ligaments
function in childbearing--increases anteroposterior diameter of rib vcage and enlarges birth canal |
|
|
lab test during pregnancy
|
1. urinalysis - for protein, sugar, signs of asymptomatic infection; drug screen for high risk groups
2. venous blood-Hgb, Hct, blood type and Rh; RPR, rubella titer, antibody titer, sickle cell. HIV and hepatitis antigen recommenced for all preg. clients 3. cultures (vaginal discharge; cervical scrapings, for chlamydia trachomatis, neisseria gonorrhoeae 4. TB screening in high risk areas 5. maternal alpha fetoprotein screen 16-18 wk optimum time 6. serum glucose screen 24-48 wk; 1 hour glucose tolerence test |
|
|
if TB is positive during pregnancy how is it treated
|
isoniazid (INH) and regampin given daily. INH is associated w/ increase in fetal malformations, particularly neurotoxicity.
Pyridoxine administered simultaneously to prevent thier developemnt |
|
|
signs of preeclamsia are
|
visual disturbances--blurring, double vision, spots before eyes
swelling of fingers, ankles, hands, feet, or face severe freqiemt pr continual headache rapid weight gain not associated w/ eating |
|
|
If there is persistant vomiting beyond first trimester or sever vomiting at any time what is possible cause
|
hyperemesis gravidarum
|
|
|
Fluid discharge from vagina---bleeding or amniotic fluid (anything other than leukorrhea--what are possible causes of this
|
placental problem, rupture of membranes
|
|
|
possible cause fo severe or unusual pain: abdominal
|
abruptio placentae
|
|
|
possible cause of abscence of fetal movmement after quickening, lasting more than 24 hours
|
intrauterine fetal death
|
|
|
who would you give RhoGAM to
|
1. mother who is Rh neg who gives birth to neonate who is Rh positive
2. nother who is Rh neg after spontaneous or induced abortion (>8week) 3. mother who is Rh neg after amniocentesis or chorionic villus sampling 4. mother who is Rh neg between 28 and 32 weeks gestation |
|
|
Older mother over age 35 primigravida ...what are some issues in pregnancy
|
1. higher incidence of congenital anomolies (down syndrome) increased possibility of complications
|
|
|
older mother over age 40 miltipara....what are some issues of pregnancey
|
increased incidence of preexisting and coexisting medical disorders (hypertension, diabetes, arthritiis)
increased incidence of complications such as preeclampsia/eclampsia, hemorrhage smoking major factor |
|
|
what is lightening
|
process in which fetus drops into pelvic inlet
1. nullipara - usually occurs 2-3 week before onset of labor 2. multipara - commonly occurs w/ onset of labor |
|
|
how much should protein be increased during pregnancy
|
30 g/day
|
|
|
folic acid during pregancy
|
800-1000 mcg through diet and supplements---prevents neural tube defects some places say 400 micrograms (0.4 milligrams) daily which is what I learned in school..the other number is coming from a hesi book
|
|
|
what maternal position provides optimum fetal and placental perfusion during pregnancy
|
the knee chest position---but ideal comfort for mother which supports fetal, maternal, and placental perfusion is the side lying position (removes pressure from abdominal vessels (vena cava, aorta)
|
|
|
what is ultrasonography used for in first trimester
|
number of fetuses
presence of fetal cardiacc movement and rhythm uterine abnormalities gestational age |
|
|
what is ultrasonography used for in 2nd and third trimester
|
fetal viability
size-date descrepancies amniotic fluid volume placental location and maturity uterine anomalies and abnormalities results of amnocentesis |
|
|
findings on ultrasonography 2nd and third trimester
|
1.fetal heart activity is apparent as early as 6-7 weeks gestation
2.serial evaluation of biparietal diameter and limb length can differentiate between wrong dates and true intrauterine growth restriction (IUGR) 3. A biophysical profile (BPP) is made to ascertain fetal well being -----a. five variables are assessed; fetal breathing movements, gross body movements, fetal tone, reactivity of fetal heart rate, and amniotic fluid volume ----b. a score of 2 or O can be obtained for each variable. An overal score of 10 designates that the fetus is well on the day of the exam |
|
|
how is gestational age best determined
|
by early sonogram rather than later one
|
|
|
what is chorionic villi sampling
|
removal of a small piece of villi during the period between 8 and 12 weeks gestation under ultrasound guidance (cannot replace amniocentesis completely b/c no sample of amnoitic fluid can be obtained for AFB or Rh disease testing
|
|
|
findings in chorionic villi sampling
|
1. the test determines genetic diagnosis early in first trimester
2. results obtained in 1 week |
|
|
nursing care for ultrasound
|
instruct woman to drink 3-4 glasses of water prior to coming for exam and not to urinate
when fetus is small in first and second trimester the clients bladder must be full during exam in order for the uterus to be supported for imaging Remember a full bladder is not needed if ultrasound is done transvaginally instead of abdominally postition woman w/ pillows under neck and knees to keep pressure off of bladder---late in third trimester, place wedge under right hip to displace uterus to the left |
|
|
nursing care for chorionic villi smapling
|
have informed consent signed before any procedure
place woman in lithotomy position using stirrups warn of slight shapr pain upon catherter insertion complications are spontaneous abortion (5%) contraversy regarding fetal anomalies (limb) |
|
|
what is amniocentesis
|
removal of amniotic fluid sample from uterus as early as 14-16 weeks
|
|
|
what is amniocentesis used to determine
|
1. fetal genetic diagnosis (usually in first trimester)
2. fetal maturity (last trimester) 3. fetal well being it is performed when uterus rises out of symphysis at 13 weeks and amniotic fluid has formed it usually takes 10 days to 2 weeks to develop cultured cell karotype--therefore woman could be well into second trimester before diagnosis is made...making choice for abortion more dangerous |
|
|
what are finding in amniocentesis
|
1. genetic disorders
a. karyotype: determines down syndrome (trisomy 21), other trisomies, and sex chromatine (sex linked disorders) b. biochemical analysis: determines more that 60 types of metabolic disorders (tay-sachs) c. AFP: elevations may be associated w/ neutral tube defects.....low levels may indicate trisomny 21 2. fetal maturity a. lecithin: sphingomyelin (L:S) ratio: 2:1 ratio indicates fetal lung maturity unless mother is diabetic or has Rh disease or fetus is septic b. L:S ration and presence fo phosphatidylglycerol (PG) : most accurate determinatio of fetal maturity. PG is present after 35 weeks gestation c. lung maturity is the best predictor of extra uterine survivial d. creatinine: renal maturity indicator >1.8 e. organge staining cells: lipid containing exfoliating sebaceous gland maturity >20% stained orage means 35 weeks or more 3. Fetal well being a. bilirubin delta optical denisity assessment s/b performed in mother previously sensitized to the fetal RH+ RBC and having antibodies to the RH+ circulating cells. The delta OD test measures the change in optical density of the amniotic fluid caused by staining w/ bilirubin-----done at 24 weeks gestation b. meconium in amniotic fluid may indicate fetal stress |
|
|
nursing care for baseline for amniocentesis
|
obtain base line vital signs and FHR
place client in supine position w/ hands across chest if prescribed shave area and scrub w/ bedadine (povidone/iodine) draw maternal blood sample for comparison w/ postprocedure blood sample to determine maternal bleeding provide emotional support, explain procedure, stay w/ the client (DO NOT LEAVE HER ALONE) label samples; if bilirubin test is prescribed darken room and immediately cover the tubes w/ aluminum foil or use opaque tubes after speciman is drawn, was abdomen, assist woman to empty bladder (a full bladder can irritate the uterus and cause contractions) monitor FHR for 1 hour after procedure and assess for uterine contractions and irritability instruct woman to report any contractions, change in fetal movement, or fluid leaking from vagina |
|
|
complications of amniocentesis are
|
spontaneous abortion (1%)
fetal injury infection |
|
|
when amniocentesis is done in early pregancy the bladder
|
must be full to help support the uterus and to help push the uterus up in the abdomen for easy access
|
|
|
when amniocentesis is done in late pregnancey the bladder
|
must be empty so it will not be punctured
|
|
|
Variables measured by fetal monitoring
|
1. begining, peak, and end of each contraction
2. duration: length of each contraction from beginning to end 3. frequency: beginning of one contraction to beginning of the next (3-5 contractions must be measured 4. intensity: measured not by external monitoring but in mmHg by internal (intrauterine) montoring after amniotic membranes have ruptured: ranges from 30mmHg (mild) to 70 mmHg (strong) at peak |
|
|
what is baseline fetal heart rate
|
the range of FHR (avg. 110-160bpm) between contractions, monotored over a 10 min period
2. the balance betwen parasympathetic and sympathetic impulses usually preduces not observable changes in the FHR during uterine contractions (w/ healthy fetus, a healthy placenta, and good uteroplacental perfusion) |
|
|
baseline FHR
|
1. normal rhythmicity
2. average FHR 110-160. 3. description --a the FHR results from the balance between the parasympathetic and the sympathetic branches of the autonomic NS b. it is the MOST IMPORTANT indicator of the health of the fetal central NS |
|
|
baseline variability
|
1. normal irregularity of cardiac rhythm
2. description a. short term variability (STV): change in fetal HR from one beat to the next --1. fetal scalp electrode (internal monitoring) is necessary to evaluate STV --2. if STV is present, the fetus is not experiencing cerebral asphyxia; therefore ITS PRESCENCE IS A REASSURING SIGN b. Long ter variability (LTV): avg 6-10 changes per minute; ie heart rate may avg 140 bpm but change from 137-149 during that minute when LTV can be evaluated by external or internal monitoring |
|
|
fetal accelerations
|
1. caused by sympathetic fetal response
2. occur in response to fetal movement 3. indicative of a reactive, healthy fetus |
|
|
early decelerations
|
1. benighn pattern caused by parasympathetic response (head compression)
2. heart rate slowly and smoothly decelrates at beginning of contraction and returns to baseline at end of contraction No nursing actions except to monitor the progress of labor document the processes of labor |
|
|
what are nonreassuring warning signs
|
1. variability
2. bradycardia 3. tachycardia |
|
|
non reassuring variability
|
1. FHR is abscent or minimal
2. short term variability is abscent 3. long term variability is minimal (3 changes per min) 4. Causes --hypoxia (asphyxia) --acidosis --maternal drug ingestion (narcotics, CNS depressants such as MgSO4) --fetal sleep |
|
|
non reassuring bradycardia
|
1. baseline FHR is below 110 bpm (assessed between contractions) for 10 minutes (as differentiated rom a periodic change
Causes --late manifestation of fetal hypoxia --medication induced (narcotics, MgSO4) --maternal hypotension --fetal heart block --prolonged umbilical cord compression |
|
|
non reassuring tachycardia
|
1. baseline FHR is above 160 bpm (assessed between contractions) for 10 minutes
Causes --early sign of fetal hypoxia --fetal anemia --dehydration --maternal infection, maternal fever --maternal hyperthyroid disease --mediation induced (atropine, retodrine, terbutaline, hydroxyzine) |
|
|
nursing actions for decreased variability, bradycardia, and tachycardia
|
treatment is based on cause
variable decel pattern --most common periodic pattern --occurs in 40% of all labors and is caused mainly by cord compression, but can also indicate rapid fetal descent characterized by --an abrupt transitory decrease in teh FHR that is variable in duration, depth of fall, and timeing relative to the contractions cycle ***an occasional variable is usually benign change maternal postition stimulate fetus if indicated d/c oxytocin if infusing administer oxygen at 10L by tight face mask perform a vaginal exam to check for cord prolapse report finding to DR and document |
|
|
nonreassuring (omnious) Signs
Severe variable decelertion |
1. FHR below 70bpm lasting longer than 30-60 seconds
2. slow return to baseline 3. decreasing or absent variability late decelerations 1. an ominous and potentially disatrous nonreassuring sign 2. indicative of uteroplacental insufficiency 3. the shape of the decelration is uniform and the FHR returns to baseline after the contraction is over 4. the depth of the decelration does not indicate severity; rarely falls below 100 bpm |
|
|
nursing actions for nonreassuring (omnious) signs severe variable deceleration
|
1, immediately turn client on side
2. D/C oxytocin if infusing 3. check scalp stimulation for accelerations (a non compromised fetus will demonstrate accelerations w/ scalp compression) 4. administer oxygen 10L by tight face mask 5. assest w/ fetal blood sampling if indicated 6. maintain intravenous line and if possible elevate legs to increase venous return 7. correct any underlying hypotension by increasing IV rate or w/ prescribed meds 8. determine presence of FHR variability 9. notify dr |
|
|
early decelerations caused by head compression and fetal descent usually occur when?
|
between 4-7 cm and in the second stage-----check for labor progress if early decelerations are noted
|
|
|
what should be done if cord prolapse is detected
|
examiner should position the mother to relieve pressure on the cord (knee chest position) or push presenting part off of cord until immediate cesarean delivery can be accomplished
|
|
|
late decelerations indicate uteroplacental insufficiency and are associated w/ what?
|
postmaturity
preeclampsia diabetes mellitus cardiac disease abruptio placentae |
|
|
when deceleration patterns (late and variable) are associated w/ decreased or absent variability and tachycardias---what does this mean
|
the situation is ominous (potentially disatrous) and requries immediate intervention and fetal assessment
|
|
|
a decrease in uteroplacental perfusion result in ?
|
late decelerations
|
|
|
cord compression results in
|
a pattern of variable decelerations
|
|
|
what is a non stress test used to determine
|
fetal well being in high risk pregnancy and especiall useful in postmaturity (notes response of the fetus to its own movement)
a healthy fetus will usually respond to its own movement by means of an FHR accelration of 15 beats, lasting for at least 15 seconds after the movement, twice in 20 min period the fetus that responds w/ 15/15 acceleration is considered reactive and healthy |
|
|
nursing care for non stress test
|
1. apply fetal monitor, ultrasound, and tokodynamometer to maternal abdomen
2. give mother handheld event marker and instruct her to push the button whenever fetal movement is felt or recorded as FM on the fetal heart rate strip 3. monitor for 20-30 minutes----observing reactivity 4.. suspect fetus is sleeping if there is no fetal movement---stimulate fetus acoustically or physically, or have mother move fetus around and begin test again |
|
|
contraction stress test or oxytocin challenge test is
|
1. the fetus is challenged w/ the stress of labor by the induction of uterine contraction, and the fetal response to physiologically decreased oxygen supply during uterine contractions is noted
--an unhealthy fetus will develop nonreassuring fetal heart rate patterns in response to uterine contractions; late decelerations are indicative of UPI Contractions can be induced by nipple stimulation or by infusing a dilute soln of oxytocin |
|
|
nursing care for contraction stress test or oxytocin challenge test is
|
--assess for contraindications: prematurity, placenta previa, hydramnios, multiple getstation, and previous uterine classical scar, rupture of membranes
--place external monitors on abdiomen (FHR ultrasound monitor and tokodynamometer) record a 20 minute baseline strip to determine fetal well being (reactivity) and presence or absence of contractions --to assess fetal well being a recording of at least 3 contraction in 10 minutes must be obtained if nipple simulation is attempted, have woman apply warm, wet washcoths to nipples and roll the nipple of one breast for 10 min. Begin rolling both nipples if contractions do not begin in 10 minutes. Preceed w/ oxytocin infusion if unsuccessful w/ nipple stimulation Piggy back w/ oxytocin (10 units of pitocin) to main IV line. Begin at 0,5 mcg/min and increase by 0.5 mcg/min every 20 minutes to achieve three firm contraction, each lasting 40 seconds over a period of 10 min a negative test suggest fetal well being (ie., no occurrence of late decelerations |
|
|
danger in nipple stimulation
|
the danger in nipple stimulation lies in controlling the "dose" of oxytocin delivered by the posterior pitutary. the chance of hyperstimulation or tetany (contraction over 90 seconds or contractions w/ less than 30 seconds in between) is increased
|
|
|
Biophysical profile is used for what
|
ultrasonograpy is used to evaluate fetal health by assessing 5 variables
1. fetal breathing movements 2. gross body movements 3. fetal tone 4. reactive fetal heart rate (non stress test) 5. qualitative amniotic fluid volume Each variable receives 2 points for a normal response or 0 points for abnormal or no response |
|
|
fetal pH blood sampling tecnique
|
performed only in the intrapartum period when the fetal blood from the presenting part (breech or scalp) ca be taken, (when membranes have ruptured and the cervix is dilated 2-3 cm
this test is used to determine true acidosis when nonreassuring fetal heart rate is noted (late decel, severe variable decel unresponsive to tx, decreased variability unrelated to nonasphyxial causes, tachycardia unrelated to maternal variables) because fetal blood gas values vary rapidly w/ transient circulatory changes, this test is usually done ONLY in tertiary centers that have the capability of repetitive sampling and rapid results |
|
|
nursing care for Fetal pH blood sampling
|
place client in lithotomy position at end of labor bed and prepare w/ perineal cleansing and sterile draping
assist health care provider by gathering steril supplies and prviding ice in cup or emesis basin to carry pipette filled w/ blood to units pH machine or lab |
|
|
accelerations are cause by
|
a burst of sympathetic activity; they are reassuring and require not tx
|
|
|
early decelerations are caused by
|
head compression; they are benign and alert the nurse to monitor for labor progress and fetal descent
|
|
|
variable decelerations are caused by
|
cord compression; change of position should be tried first
|
|
|
late decelerations are caused by
|
UPI and chould be treated by placeing client on her side and adminstering oxygen
|
|
|
what is the most important indicator of fetal autonomic nervous system integrity and health
|
fetal heart rate variability
|
|
|
stages of labor are
|
latent
active transition |
|
|
latent phase is
|
from beginning of true labor until 3-4 cm cervical dilation
contractions mild initially 10-20 min apart 15-20 seconds durations later 5-7 min apart 30-40 seconds duration |
|
|
active phase of labor
|
from 4-7 cm cervical dialation
increased anxiety increased discomfort unwillingness to be left alone contractions moderate to severe 2-3 min apart 30-60 seconds in duration |
|
|
transition phase of labor
|
from 8-10 cm cervical dilation
changed behavior sudden nausea, hiccups extreme irritability and unwillingness to be touched although desire of companionship contractions severe 1 1/2 min apart 60-90 seconds duration |
|
|
Intrapartum nusing care begins w/ true labor and consist of what 4 stages
|
1. from the beginning of regular contractions or rupture of membranes to 10 centimeters of dilation and 100% effacement
2. 10 cm to delivery 3. delivery of the placenta 4. first 1-4 hours following delivery |
|
|
difference between true labor and false labor
|
true labor
--pain in lower back that radiates to abdomen --pain accompanied by regular rhythmic contractions --contractions that intensify w/ ambulation --progressive cervical dilatation and effacement false labor --discomfort localized in abdomen --no lower back pain --contractions decrease in internsity or frequency w/ ambulations |
|
|
prodromal labor signs include
|
1. lightening (fetus drops into true pelvis)
2. braxton hicks contractions (practice contractions) 3. cervical softening and slight effacement 4. bloody show or expulsion of mucousl plug 5. burst of energy ---nesting instinct |
|
|
in prodromal labor determine the following
|
1. gravidity and parity >5 (grand multiparity)
2. gestational age 37-42 weeks (term gestation) 3. FHR best head over fetal back 4. maternal vital signs 5. contraction frequency, intensity and duration |
|
|
perform vaginal exam to determine?
|
fetal presentation and position
cervical dilatation, effacement, position, and consitency fetal station |
|
|
assess the client for
|
status of membranes (ruptured or intact)
urine glucose and albumin data comfort level labor and delivery preparation presence of support person presence of true or false labor |
|
|
vaginal exam is preceded by antiseptic cleansing, w/ client in modified lithotomy position then
|
sterile gloves are worn
exams are not done routinely..they are sharply curtailed after membranes rupture to prevent infection |
|
|
vaginal exams are performed
|
prior to analgesia and anesthesia
to determine the progress of labor to determine whether second stage pushing can begin |
|
|
the purpose of a vaginal examination is to determine
|
1. cervical dilation: cervix opens from 0 to 10 cm
2. cervical effacement: cervix is taken up into th eupper uterine segment; expressed in percentage from 0% to 100%---cervix is shortened from 3 cm to <0.5 cm in length; often called thinning of the cervix an misnomer 3. cervical position: cervix can be directly anterior and plapated easily or posterior and difficult to palpate cervical consistency: it is firm to soft |
|
|
what is fetal station
|
location of presenting pare in relation to midpelvis or ischial spines; expressed as cm above or below the spinds
|
|
|
fetal station 0 is
|
engaged
|
|
|
station -2 is
|
2 cm above the ischial spines
|
|
|
fetal presentation is
|
the part of the fetus that presents to the inlet
|
|
|
vertex is
|
head, cephaic
|
|
|
shoulder is
|
acromion
|
|
|
breech is
|
buttocks
|
|
|
other variations include
|
brow (sinciput) and chin (mentum)
|
|
|
fetal position
|
the relationship of the point of reference (occiput, sacrum, acromion) on the fetal presenting part (vertex, breech, shoulder) to the mothers pelvis. Most common is LOA (left occiput anterior) the point of freference on the vertex (occiput) is pointe up toward the symphysis and direct toward the left side of the maternal pelvis
|
|
|
fetal lie
|
the relationship of the long axix (spine) of the fetus to the long axis (spine) of themother. It can be either longitudinal (up and down) transverse (perpendicular), or oblique (slanted)
|
|
|
fetal attitude is
|
relations hipe of fetal parts to one another
flexion or externsion flexion is desirable so that the smallest diameter of the presenting part move through the pelvis |
|
|
normal findings for client in labor
|
--normal FHR in labor = 110-160 bpm
--normal maternal BP: <140/90 --normal maternal pulse: <100 bpm --normal maternal temp: <100.4 F --slight elevation in temperature may occur b/c of dehydration and the work of labor. Anything higher indicates infection and must be reported immediatly |
|
|
determine FHR auscultation schedule
|
FHR every 30 min in latent phase
FHR every 15-30 minutes in midactive stage FHR ever 15 minutes in trasition stage |
|
|
assess maternal vital signs
|
1. take BP betwen contractions, in side lying position at least every hour unless abnormal (BP increases during contractions
2. take temp every 4 hours until membranes rupture, then every hour |
|
|
determine birth plan desires for
|
analgesia and anesthesia
delivery situation |
|
|
Urine s/b assessed
|
every 8 hours unless abnormal
normal findings Protein=glucose = 1+ or less |
|
|
assess contractions when assessing FHR
|
1. frequency: time contractions from beginning of one contraction to the beginning of next contraction (measured in minutes apart)
duration: time the length of the entire contraction (from beginning to end) strength--assess intensity of strongest part (peak) of contraction. It is measured by clinical estimation of the indentability of the fundus (use gentle pressure of fingertips to determine it) |
|
|
if membranes of bag of water has ruptured...signs are
|
1. nitrazine paper turns black or dark blue
2. vaginal fluid ferns under microscope 3. color and amoutn of amniotic fluid s/b noted 4. woman s/b allowed to ambulate during labor only if the FHR is w/in a normal range and if the fetus is engaged (0 station). if the fetus is not engage, there is an increased risk that a prolapsed cord will occur |
|
|
begin a graph of labor progress....
|
1. prolonged latent phase lasts > 20 hours in primgravida
>14 hours in multipara 2. a primigravida dilates an avg of 1.2 cm/hr in the midactive phase; a multipara 1.5 cm/hr |
|
|
client should be taken to the bathroom or offered a bedpan when during labor
|
at least every 2 hourse ( a full bladder can impede labor progress)
|
|
|
meconium stained fluid is what color and may indicate what
|
fluid is yellow green or gold yellow and may indicate fetal stress
|
|
|
should assist woman w/ the use of psychoprophylactic coping techniques such as
|
breathing exercises and effleurage (abdominal massage)
|
|
|
breathing techniques such as deep chest, accelerated, and cued are not prescribed by the stage and phase of labor but by
|
the discomfort level of the laboring woman----if coping is decreasing switch to another method
|
|
|
Hyperventilation results in
|
respiratory alkalosis that is caused by blowing off too much CO2
Symptoms --dizziness --tingling in fingers --stiff mouth --------have woman breathe into her cupped hands or in a paper bag in order to rebreathe CO2 |
|
|
anesthesia and analgesis is offered when
|
in midactive phase of labor----if given too early they will retard the progress of labor
if given too late, narcotics increase the risk of neonatal respiratory depression |
|
|
notify dr if
|
1. labor progress is retarded
2. maternal vital signs are abnormal 3. fetal distress is noted |
|
|
facts about 2nd stage of labor
|
1. Heralded by the involuntary need to push, 10 centimeter of cervical dilatation, rapid fetal descent
---second stage of labor avg. 1 hour for a primigravida and 15 min for a multipara --the addition of abdominal force to the utrine contraction force enhances the cardinal movements of the fetus: engagement, descent, flexion, internal rotation, extension, restitution, and external rotation |
|
|
nursing assessment 2nd stage of labor
|
assess BP and pulse every 5-15 min
detrmine FHR w/ every contraction observe perineal area for --increase in bloody show --bulging perineum and anus --visibility of the presenting part palpate bladder for distention assess amniotic fluid for color and consitency |
|
|
nursing plans and interventions for 2nd stage of labor
|
1. document meaternal BP and pulse every 15 min between contraction
2. check fetal heart rate w/ each contraction or by continuous fetal monitoring 3. continue comfort measure: mouth care, linen change, positioning 4. decrease outside distractions 5. teach mother positions such as aquatting, side lying, or high fowler/lithotomy for pushing 6. teach mother to hold breath for no longer than 5 seconds during pushing 7. teach mother to exhale when pushing or use gentle pushing technique (pushing down on vagina, while constantly exhaing through open mouth, followed by deep breath) |
|
|
determine cervical dilatation before allwoing client to push. Cervix should be completely dilated (10cm) before the client begins pushing or what can happen
|
if pushing starts too early, the cervix can become edematous and never fully dilate
|
|
|
procedures for delivering in another room
|
1. transfer multipara at 8-9 cm, +2 station
2. transfer primigravida at 10 cm, w/ presenting part visible between contractions and during contractions 3. set up delivery table, including bulb syringe, cord clamp, and sterile supplies 4. perform perineal cleansing 5. at crowning put gentle counterpressure against the perineum. Do not allow rapid delivery over womans perineum 6. make sure cleint and support person can visualize delivery if they so desire. I fsiblings are present, make sure they are clesly attended to by support person explaining their mom is all right Record exact delivery time (complete delivery of baby) |
|
|
third stage of labor
|
from complete expulsion of the baby to complete expulsion of the placenta
avg length of 3rd stage is 5-15 minutes the longer the third stage of labor, the greter the chance for uterine atony or hemorrhage to occur |
|
|
what are signs of placental separation
|
1. Lengthening of umbilical cord outside of vagina
2. gush of blood 3. uterus changes from oval (discoid) to globular Mother describes a full feeling in vagina firm uterine contractions continue |
|
|
when do you give oxytocin
|
give oxytocin after the placenta is delivered b/c the drug will cause the uterus to contract. If the oxytocic drug is administered before the placenta is delivered, it may result in a retained placenta, which predisposes the client to hemorrhage and infection
|
|
|
Placental separation procedure
|
place hand under drap and palpate fundus of uterus for firmness and placement at or below the umbilicus----at signs of placental separation, instruct mother to push gently
take maternal BP before and after placental separation check patency and site integrity of infusing IV administer oxytocic medication immediately after delibery of the placenta observe for blood loss and ask physicia for estmate of blood loss dry and suction infant, perform apgar assessment, place blanket on mothers abdomen or allow skin to skin contact w/ mother after delivery place stockinett cap on newborns head or cover head to prevent heat loss allow faterh or other support person to hold infant during repair of episiotomy allow siblings present to hold new family member gently cleanse vulva and apply steril perineal pad remove both legs simultaneously if legs are in stirrups provide clean gown and warm blanket lock bed before moving mother, and raise side rails during transfer |
|
|
application of perineal pads after delivery
|
place 2 on perineum
do not touch inside of pad apply from front to back, being careful not to drag pad across the anus |
|
|
oxytocin
|
give immediately after delivery of placenta to avoid trapped placenta
10-20 units added to remaining IV fluid at least 50 ml may stimulate let down milk reflexs and flow of milk when engorged |
|
|
indications of oxytocin
|
uterine atony
|
|
|
adverse reactions of oxytocin
|
severe afterpains in multipara
hypertension |
|
|
methylergonovine maleate (methergine) nursing implications
|
usual dose: 0.2 mg IM followed by tabs of 0.2 mg every 4-6 hours
use w/ caution in clients w/ elevated BP or reeclampsia take BP prior to administration and if 140/90 or above, w/ hold and notify dr |
|
|
methylergonovine indications
|
uterine atony
|
|
|
methylergonovine adverse reactions
|
hypertension
***not given to clients w/ hypertension b/c of its vasoconstrictive action NEVER give methergine to a client while she is in labor or before delivery of placenta |
|
|
prostaglandin F2 (Hemabate) nursing implications
|
contraindicated for clients w/ asthma
dose is 0.25 IM every 15-90 minutes; up to 8 doses may be given intramyometrially by provider check temperature every 1-2 hours auscultate breath sounds frequently |
|
|
prostaglandin F2 adverse reactions
|
headache
nausea and vomiting fever bronchospasm, wheezing |
|
|
prostaglandin F2 indications
|
uterine atony
NEVER Give prostaglandin to a client while she is in labor or before delivery of placenta |
|
|
fourth stage of labor
|
the fourth stage of labor is the first 1-4 hours after delivery of placenta
|
|
|
Nursing assessment for 4th stage of labor
|
A. Review antepartum and labor and delivery records for possible complications
1. postpartum hemorrhage 2. uterine hyperstimulation 3. uterine overdistension 4. dystocia 5. anterpartum hemorrhage 6. magnesium sulfate therapy 7. bladder distension b. routine postpartum physical assessment c. mother infant bonding |
|
|
Nursing planas and interventions for 4th stage of labor
|
a. maintain bed rest for at least 2 hours to prevent orthostatic hypotension
b. assess bp, pulse, and respirations every 15 minutes for 1 hour, then every 30 minutes until stable (BP<140/90, pulse <100, and respiration <24 D. assess fundal firmness and height, bladder, lochia, and perineum every 15 minutes for 1 hour, then every 30 minutes for 2 hours |
|
|
fundus should be
|
firm, midline, at or below the umbilicus. Massage if soft or boggy--------------suspect full bladder if above umbilicus and to the right side of abdomen
|
|
|
Lochia is
|
rubra (red), moderate, and clots <2 to 3 cm. Suspect undetected laceration if fundus is firm and bright red blood dontinues to trickle. Always check perineal pad and under buttocks
|
|
|
Perineum should be
|
intact, clean, and slightly edematous. Suspect hematomas if very tender or discolored or if pain is disproportionate to vaginal delivery
|
|
|
one of the most common reasons for uterine atony or hemorrhage in the first 24 hours after delivery
|
a full bladder--------------if the nurse finds the fundus soft, boggy and displaced above and to the right of the umbilicus, what action should be taken first--------------------perform fundal massage; then have the client empty her bladder-----recheck fundus every 15 minutes for 1 hour, the every 30 minutes for 2 hours
|
|
|
things that should be reported to the doctor are
|
1. abnormal vital signs
2. uterus not becoming firm w/ massage 3. second perineal pad soaked in 15 minutes 4. signs of hypovolemic shock---pale, clammy, tachycardic, light headed, hypotensive |
|
|
what should nurse do if analgesics (codeine, meperidine) are given
|
raise side rails and place call light w/in reach
instruct client not to get out of bed or ambulate w/out assistance caution client about drowsiness as a side effect |
|
|
more nursing interventions in 4th stage of labor
|
Prevent discomfort of afterpains
--keep bladder empty---catherterize only if absolutely necessary --place warm blanket on abdomen --administer analgesics as prescribed (usually codeine, acetaminophen, or ibuprofen) offer fluids PO when woman is alert and able to swallow apply ice pack to perineium to minimize edema, especially if a thir or fourth degree episiotmy has been performed or if lacerations are present apply witch hazel compresses for comfort |
|
|
first degree tear involves
|
only the epidermis
|
|
|
2nd degree tear involves
|
dermis, muscle and fascia
|
|
|
a third degree tear
|
extends into anal sphincter
|
|
|
a fourth degree tear
|
extends up the rectal mucosa
|
|
|
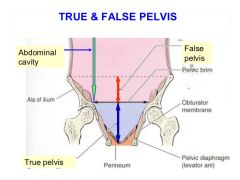
True Pelvis lies below pelvic brim: pelvic inlet mid pelvis & pelvic outlet False Pelvis is the shallow portion above pelvic brim supports abdominal viscera |
|
|
Pelvis: Oval shape adequate outlet w/ narrow pubic arch |
Anthropoid |
|
|
Pelvis: heart shaped or angulated; resembles male. Not favorable for labor & birth. Causes: |
Android Slow descent |
|
|
Pelvis: Flat with oval inlet wide transverse diameter but short anteroposterior diameter. Labor & birth difficult |
Platypelloid |
|
|
Pelvis: Normal transversely rounded or blunt. Most favorable for labor & birth |
Gynecoid |
|
|
Menstrual phase that begins with Ovulation when body temp increases 0.5-1 |
Luteal |
|
|
Pre-embryonic Embryonic Fetal Neonate/newborn |
First 2 weeks after conception Day 15-week8 Week 9 to birth Birth-1yr |
|
|
Umbilical Cord |
2 arteries 1 vein Arteries-cary deO2 blood (way from fetal heart) Veins bring O2 blood (to fetal heart) |
|
|
Fetal HR |
160-170 1st 120-160 thru birth usually double maternal Physician must be notified if outside parameters |

