![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
What is PEEP?
|
positive end-expiratory pressure (PEEP)
|
|
|
PEEP helps maintain patency of alveoli and small airways in the presence of destabilizing factors and therefore reverses hypoxemia and atelectasis by improving matching of ventilation and perfusion. PEEP levels between 0 and 10 cmH2O are generally safe and effective; higher levels are recommended only in the management of significant refractory hypoxemia unresponsive to increments in FIO2 up to 0.6.
(Just FYI) |
all intubated, mechanically ventilated patients should undergo a daily screening of respiratory function. If oxygenation is stable (i.e., PaO2/FIO2 > 200 and PEEP ≤ 5 cmH2O), cough and airway reflexes are intact, and no vasopressor agents or sedatives are being administered, the patient has passed the screening test and should undergo a spontaneous breathing trial.
(Just FYI) |
|
|
Muscles of inspiration
|
1. External intercostals
2. Sternocleidomastoid 3. Anterior serrati 4. Scaleni |
|
|
Muscles of expiration
|
1. Abdominal recti
2. Internal intercostals 3. Elastic rebound |
|
|
Pleural pressures:
a) resting b) inspiration |
a) -5 cm H2O
b) -8 cm H20 |
|
|
Alveoloar pressure:
a) resting b) inspiration c) expiration |
a) 0 cm H2O
b) -1 cm H2O c) 1 cm H20 |
|
|
Compliance ΔV/ΔP = ?
|
200 ml / cm H2O
(1 cm H2O ~ 0.7 mmHG) |
|
|
The relationship between the volume of gas contained in the lungs and the distending pressure (the transpulmonary pressure, or PTP, defined as alveolar pressure minus pleural pressure) is described by the pressure-volume curve of the lungs (Fig. 234-3A).
|

.
|
|
|
What is a primary component of transpulmonary pressure?
|
Elastic recoil
|
|
|
What are limiting features of transpulmonary pressure?
|
Lung and chest wall compliance are limiting features.
|
|
|
transpulmonary pressure is the pressure difference between that in the alveoli and that on the outer surfaces of the lungs, and it is a measure of the elastic forces in the lungs that tend to collapse the lungs at each instant of respiration, called the _______ _________
|
recoil pressure.
|
|
|
The extent to which the lungs will expand for each unit increase in transpulmonary pressure (if enough time is allowed to reach equilibrium) is called the ____ ______.
|
lung compliance
|
|
|
What is lung surfactant phospholipid?
|
dipalmitoylphosphatidylcholine
|
|
|
The total compliance of both lungs together in the normal adult human being averages about _?_ milliliters of air per centimeter of water transpulmonary pressure. That is, every time the transpulmonary pressure increases 1 centimeter of water, the lung volume, after 10 to 20 seconds, will expand _?_ milliliters.
|
200
|
|
|
the tissue elastic forces tending to cause collapse of the air-filled lung represent only about (?fraction-a?) of the total lung elasticity, whereas the fluid-air surface tension forces in the alveoli represent about (?fraction-b?).
|
a) 1/3
b) 2/3 |
|
|
It is secreted by special surfactant-secreting epithelial cells called _____ _______ _____ cells, which constitute about 10 per cent of the surface area of the alveoli.
|
type II alveolar epithelial
(These cells are granular, containing lipid inclusions that are secreted in the surfactant into the alveoli) |
|
|
If the air passages leading from the alveoli of the lungs are blocked, the surface tension in the alveoli tends to collapse the alveoli. This creates positive pressure in the alveoli, attempting to push the air out. The amount of pressure generated in this way in an alveolus can be calculated from the following formula:
|
P = 2 x surface tension / radius of alveolus
|
|
|
For the average-sized alveolus with a radius of about 100 micrometers and lined with normal surfactant, this calculates to be about 4 centimeters of water pressure (3 mm Hg). If the alveoli were lined with pure water without any surfactant, the pressure would calculate to be about _?_ centimeters of water pressure, _?_ times as great
|
18
4.5x |
|
|
What's the first thing that happens to air when it is inhaled
|
air is humidified
|
|
|
the smaller the alveolus, the _______ the alveolar pressure caused by the surface tension
|
greater
|
|
|
when might you start to dissolve your lungs?
|
when you lack alpha-1 anti-trypsin
|
|
|
The work of inspiration can be divided into three fractions: (1) that required to expand the lungs against the lung and chest elastic forces, called ______ (2) that required to overcome the viscosity of the lung and chest wall structures, called _______; and (3) that required to overcome airway resistance to movement of air into the lungs, called _______.
|
1) compliance work or elastic work;
2) tissue resistance work 3) airway resistance work |
|
|
During normal quiet respiration, the total energy expended by the body required for pulmonary ventilation.
|
only 3 to 5 per cent
|
|
|
during heavy exercise, the amount of energy required can increase as much as _?_-fold,
|
50
|
|
|
dead space air.
|
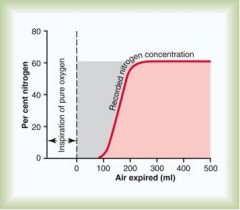
With a little thought, the student can see that the gray area represents the air that has no nitrogen in it; this area is a measure of the volume of _____
|
|
|
VD = gray area * VE / (pink area + gray area)
|
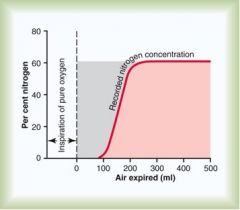
where VD is dead space air and VE is the total volume of expired air, make eqn for dead space air based on this graph
|
|
|
The normal dead space air in a young adult man is about __?_ milliliters. This increases slightly with age.
|
150
|
|
|
Do obstructions create dead space?
|
no
|
|
|
When the alveolar dead space is included in the total measurement of dead space, this is called the ____ ____ ____, in contradistinction to the anatomic dead space.
|
physiologic dead space
|
|
|
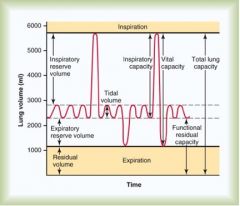
the volume of air inspired or expired with each normal breath; it amounts to about 500 milliliters in the adult male.
|
tidal volume
|
|
|
response to hypoxia in the lungs as compared to the periphery
|
it is reversed
|
|
|
What is the extra volume of air that can be inspired over and above the normal tidal volume when the person inspires with full force? it is usually equal to about ___?___ milliliters.
|
The inspiratory reserve volume
3000 |
|
|
What is the maximum extra volume of air that can be expired by forceful expiration after the end of a normal tidal expiration? this normally amounts to about __?__ milliliters.
|
The expiratory reserve volume
1100 |
|
|
What is the volume of air remaining in the lungs after the most forceful expiration? this volume averages about __?__ milliliters.
|
The residual volume
1200 |
|
|
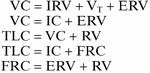
the tidal volume plus the inspiratory reserve volume = ?
|
The inspiratory capacity
|
|
|
the expiratory reserve volume plus the residual volume = ?
|
The functional residual capacity
|
|
|
the inspiratory reserve volume plus the tidal volume plus the expiratory reserve volume = ?
|
The vital capacity
|
|
|
the vital capacity plus the residual volume = ?
|
The total lung capacity
the maximum volume to which the lungs can be expanded with the greatest possible effort (about 5800 milliliters) |
|
|
All pulmonary volumes and capacities are about _____per cent less in women than in men, and they are greater in large and athletic people than in small and asthenic people.
|
20 to 25
|
|
|
Afferent nerve impulses pass from the respiratory passages mainly through the vagus nerves to the medulla of the brain. There, an automatic sequence of events is triggered by the neuronal circuits of the medulla, causing the following effect:
|
Cough reflex
|
|
|
The initiating stimulus of the sneeze reflex is irritation in the nasal passageways; the afferent impulses pass in the ______ nerve to the medulla, where the reflex is triggered.
|
fifth cranial - trigeminal
|
|
|
What are the 3 functions of "the air conditioning function" of the upper respiratory passageways
|
(1) the air is warmed by the extensive surfaces of the conchae and septum, a total area of about 160 square centimeters (see Figure 37–8); (2) the air is almost completely humidified even before it passes beyond the nose; and (3) the air is partially filtered.
|
|
Think about relations
|
.
|
|
|
alveoli & tissue capillaries
|
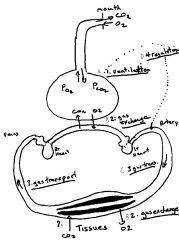
Where does gas exchange occur?
|

