![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
6 Cards in this Set
- Front
- Back
|
What is the role of the "crossing vessel" in regards to UPJ obstruction?
|
Significant controversy persists regarding the potential role of “aberrant” vessels in the etiology of UPJ obstruction. Significant crossing vessels have been noted in as many as 40% of cases of UPJ obstruction but as little as 20% of cases of normal kidneys ( Quillin et al, 1996 ; Zeltser et al, 2004 ). Although these lower pole vessels have often been referred to as aberrant, these segmental vessels, which may be branches from the main renal artery or arise directly from the aorta, are usually normal variants ( Stephens, 1982 ). In some patients, these lower pole vessels cross the ureter posteriorly and truly have an aberrant course. Regardless, it is unlikely that the associated vessel alone is causing the primary obstruction ( Hanna, 1978 ). In fact, the true etiology is an intrinsic lesion at the UPJ or proximal ureter that causes dilatation and ballooning of the renal pelvis over the polar or aberrant vessel. Recent studies using three-dimensional multidetector row computed tomography (CT) demonstrated that the precise location of crossing vessels did not correspond to the obstructive transition point in patients with UPJ obstruction ( Lawler et al, 2005 ). In contrast, one group found improvement in patients undergoing only ligation of crossing vessels ( Keeley et al, 1996 ). Regardless, the presence of crossing vessels most certainly has a detrimental effect on the success rates of minimally invasive treatments of UPJ obstruction, in particular endopyelotomy.
|
|
|
What are presenting signs/symptoms of a UPJ obstruction?
|
*UPJ obstruction, although most often a congenital problem, can present clinically at any time of life.
istorically, the most common presentation in neonates and infants was the finding of a palpable flank mass. However, the current widespread use of maternal, prenatal ultrasonography has led to a dramatic increase in the number of asymptomatic newborns being diagnosed with hydronephrosis, many of whom are subsequently found to have UPJ obstruction ( Bernstein et al, 1988 ; Wolpert et al, 1989 ). A fraction of cases may also be found during evaluation of azotemia, which may result from bilateral obstruction in a functionally or anatomically solitary kidney. UPJ obstruction may also be incidentally found during studies performed to evaluate unrelated anomalies such as congenital heart disease ( Roth and Gonzales, 1983 ). In older children or adults, intermittent abdominal or flank pain, at times associated with nausea or vomiting, is a frequent presenting symptom. Hematuria, either spontaneous or associated with otherwise relatively minor trauma, may also be an initial symptom. Laboratory findings of microhematuria, pyuria, or frank urinary tract infection might also bring an otherwise asymptomatic patient to the urologist. Rarely, hypertension may be a presenting finding. |
|
|
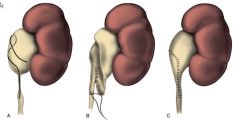
How does one perform a ureterocalycostomy?
|
*The ureter is identified and dissected as far cephalad as possible.
*A lower pole partial nephrectomy is performed so as to provide access to the lower pole calyx, a simple nephrotomy is not sufficient as it will likely stricture *Ureter is spatulated laterally, and the apex of the spatulation is sutured to the lateral portion of the calyx, then stitch 180 degrees away, then split the difference in an interrupted fashion till closed. *Close the renal capsule defect as much as possible without causing compression on new anastamosis, and for remainder place a peritoneal or omental or perinephric fat flap. |
|
|
Who is the dismembered pyeloplasty named after?
|
*It is also known as the Anderson-Hynes pyeloplasty which was originally described in 1949 to fix a retrocaval ureter.
|
|
|

|
|

|
|

