![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
|
Meningioma- hx
|
-Peak incidence 6-7th decades
-Female predominance -Most common location is at falx or base of skull -May present with seizures, headaches, and focal neurologic deficits -Early morning headache (d/t increased ICP) -Possible loss of taste/smell (olfactory meningioma) |
|
|
Meningioma- phys
|
-Focal neurologic deficits
-Cranial neuropathies may arise if tumor is from base of skull -Paraparesis if tumor is in falx cerebri – causes bilateral compression of leg areas of motor cortex |
|
|
Meningioma- dx tests
|
-CT: smooth, lobulated, isodense tumor that is adjacent to dura and enhances uniformly w/ contrast; possible multiple small calcifications
-MRI: less characteristic; T1- isointense or hypointense; T2- isointense or hyperintense; possible edema in adjacent brain |
|
|
Meningioma- tx
|
-Many are slow growing, small and asymptomatic and thus can be followed w/ periodic imaging
-When tumor becomes symptomatic, partial or total removal is indicated -Gammaknife tx -Radiotherapy and chemo show no benefit |
|
|
Meningioma- prognosis
|
-Total tumor removal has a 10 year recurrence rate of10%
-Partial removal has a 10 yr recurrence rate of major sx in 40% -90% are benign, 10% are aggressive |
|
|
Meningioma- pathophys
|
-60% of sporadic meningiomas have NF2 mutation
-Pathology: whirls of cells w/ pseudonuclear inclusions; psammoma bodies -WHO Grade I-III -Slow-growing benign tumors attached to dura composed of neoplastic arachnoid cells -20% recurrence in 20 yrs -Atypical meningioma: increase in cellularity & growth, increased mitoses, prominent nucleoli |
|
|
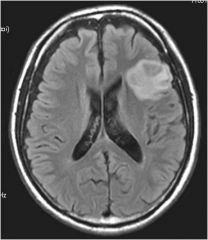
What tumor is shown here
|
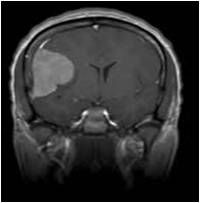
|
|
What tumor is shown here
|
Meningioma
|
|
|
Ependymoma- dif
|
-CNS mass
-Meningitis -Encephalitis -ADEM -Abscess |
|
|
Ependymoma- hx
|
-Typically occurs in first 2 decades of life, 30% in children <3 yo
-Headache (60%), usually worse in am -N/V secondary to increased ICP (80%) -Behavioral changes: lethargy, irritability, decreased social interaction, loss of appetite (50%) -Ataxia, dizziness (30%) |
|
|
Ependymoma- phys
|
-Papilledema (60%)
-Ataxia (45%) -Nystagmus with or without gaze palsy (40%) -Apraxia or hemiparesis (20%) -Increase in head circumf in children <2 yo (10%) |
|
|
Ependymoma- dx tests
|
-MRI: Evidence of calcification, necrosis, cystic change; 2/3 are located in posterior fossa, 90% in 4th ventricle
-LP: contraindicated! |
|
|
Ependymoma- tx
|
-Preoperative steroids to limit edema and alleviate sx
-Surgical resction: most effective therapy -Postoperative radiation therapy improves survival |
|
|
Ependymoma- prog
|
-Gross total resection: progression-free survival rates of 70-80% after 5 years, compared to 35% for incomplete resection
-The younger the pt, the worse the prognosis -May lead to hydrocephalus increased ICP -Usually do not proliferate rapidly, are not invasive, and do not metastasize |
|
|
Ependymoma- pathophys
|
-Summary: neoplasms of ependymal cells that occur throughout the entire neuraxis in association with the lining of the cerebral ventricles and central canal of the spinal cord
-Pathology: well circumscribed lesion; perivascular pseudorosette formation, cellular atypia -WHO Grade II -Slow-growing tumor originating from the wall of cerebral ventricles (ependyma) |
|

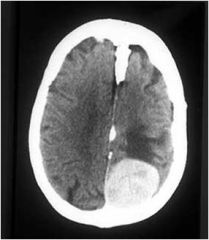
What type of tumor is this
|
Ependymoma
|
|
|
Astrocytoma - pilocytic- dif
|
-Ependymoma
-Headache -Hydrocephalus -Head injury -MS -Oligodendro glioma -Epidural abscess -Subdural empyema -Cerebral abscess -Hamartoma -AVM |
|
|
Astrocytoma - pilocytic- hx/phys
|
-Presents in 1st 2 decades
-Early morning headache (d/t increased ICP) -Can cause sxs by perturbing cerebral function (seizures), elevating ICP by mass effect or obstructing CSF pathways ( hydrocephalus), or causing neurologic abnormalities (paralysis, sensory deficits, aberrant behavior, HA) |
|
|
Astrocytoma - pilocytic- dx tests
|
-MRI: Contrast enhancing because there are abnormal leaky, proliferating blood vessels that allow for enhancem.
|
|
|
Astrocytoma - pilocytic- tx
|
-Surgery is 1st line
-Phenytoin for sz |
|
|
Astrocytoma - pilocytic prognosis
|
-Cured if undergo gross total resection
-Unresected - neurologic deficit may occur over a period of years -Median survival duration is 7.5 yrs -Age at onset, type of astrocytoma and type of therapy influence outcomes -May dedifferentiate into a higher grade lesion |
|
|
Astrocytoma - pilocytic- pathophys
|
-Low grade, slow-growing
-Occurs throughout CNS, cerebellum, optic nerve, hypothalamus -Pathology: biphasic growth pattern, bipolar cells w/ long processes; Rosenthal fibers (degenerative processes); rare mitoses -WHO Grade I: well circumscribed, often cystic -Most common glioma (and solid tumor) in children |
|

What type of tumor
|
Astrocytoma - pilocytic
|
|
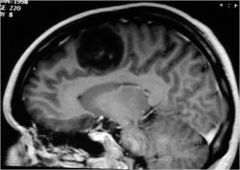
What tumor was this person treated for?
|
astrocytoma
|
|
|
Astrocytoma – diffusely infiltrating- hx
|
-60% occur btwn 20-45 yo
-Can occur anywhere, most commonly cerebrum |
|
|
Astrocytoma – diffusely infiltrating- tx
|
-Can’t be surgically resected
|
|
|
Astrocytoma – diffusely infiltrating- pathophys
|
-60% occur btwn 20-45 yo
-Can occur anywhere, most commonly cerebrum -WHO Grade II-IV: progression to malignancy from astrocyte w/ genetic mutation astrocytoma anaplastic astrocytoma glioblastoma |
|
|
Glioblastoma- hx
|
-Tends to occur in older adults (mean age 55 yrs)
-Most common primary brain tumor in adults -Headaches (50%) -Altered mental status (50%) -Seizures (20%) – focal or secondarily generalized tonic-clonic -Sx progress rapidly in the absence of tx |
|
|
Glioblastoma- phys
|
-Hemiparesis (40%)
-Aphasia (15%) -Visual field loss (5%) -Papilledema |
|
|
Glioblastoma- dx tests
|
-MRI w/ gad: central low signal intensity on T1 outlined by high intensity ring-enhancement; surrounding high intensity areas are hypointense signals that represent cerebral edema and tumor infiltration
-CT: variably hypodense or isodense lesions surrounded by hypodense cerebral edema -EEG: focal or extensive slowing (delta waves) in tumor region |
|
|
Glioblastoma- tx
|
-Management aims at slightly prolonging survival and controlling sx
-Corticosteroids to reduce vasogenic edema & prolong survival 1-3 mos -Neurologic side effects of high dose steroids: psychosis, hyperactivity, irritability, insomnia, myopathy -Surgical removal (debulking) improves length of survival and improves neurologic sx by reducing ICP -Radiotherapy after surg slightly improves survival -Anticonvulsants to control sz -Palliative care |
|
|
Glioblastoma- prog
|
-Survival less than 18 mos., always fatal
-Survival <6 mos if untreated -Better prognosis in young pts |
|
|
Glioblastoma- pathophys
|
-WHO Grade IV: highest grade astrocytic neoplasm
-Can cause uncal herniation -Primary glioblastoma: de novo; older ages; genetic mutations (EGFR – epidermal growth factor) -Secondary glioblastoma: progression over time from diffuse astrocytoma; younger ages; mutation of p55 -Pathology: microvascular proliferation, pseudopallisading necrosis, multinucleated giant cells |
|
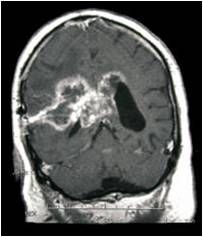
Type of tumor?
|
Glioblastoma
|
|
|
Oligodendroglioma- hx
|
-Incidence peaks in 5th-6th decades; M:F is 1:1
-Slow-growing neoplasm -Frontal lobe 50-65% of cases -Early morning headache (d/t increased ICP) |
|
|
Oligodendroglioma- tx
|
-Loss of heterozygosity of 1p & 19q responds to chemo treatment and increases life expectancy
- not generally surgically resectable - slow growing so watchful waiting. |
|
|
Oligodendroglioma- pathology
|
-Pathology: -Well circumscribed w/ calcifications; diffusely infiltrates white matter & cortex; proliferating, leaky blood vessels, atypical, enlarged nuclei; Fried egg, halo artifact; Chicken wire vasculature
|
|
Type of tumor?
|
Oligodendroglioma
|
|
|
Medulloblastoma- epi
|
-Peak at 7 yrs of age
|
|
|
Medulloblastoma- phys
|
-Can grow along 4th ventricle cause hydrocephalus
|
|
|
Medulloblastoma- prog
|
-5 yr survival 50-70% w/ poor developmental outcomes
|
|
|
Medulloblastoma- patho
|
-WHO Grade IV
-Malignant, invasive embryonal tumor in cerebellum; in posterior cranial fossa |
|
|
Brain metastasis- hx
|
-25% of cancer pts develop brain mets
-Impaired cognition (60%) -Headache (60%) -Aphasia (205) -Seizures (20%) – focal, motor -Stupor or coma (5%) -Clinical sx occur via displacement of brain tissue from rapidly growing tumor and surrounding vasogenic edema vessel compression ischemia |
|
|
Brain metastasis- phy
|
-Hemiparesis (60%)
-Hemisensory loss (20%) -Papilledema (20%) -Visual field cut (10%) |
|
|
Brain metastasis- dx test
|
-MRI w/ gad: best diagnostic test; T1 w/ gad – heterogeneous or ring-enhancing lesion usually w/ surrounding edema; shifting of brain structures d/t mass effect
-Majority of mets are supratentorial – 80% loc in cerebral hemispheres |
|
|
Brain metastasis- tx
|
-Surgical removal of met only occasionally is helpful in markedly prolongling life
-Dexamethasone reduces edema and dramatically improves sx for 1-2 mos -Radiation therapy adds a few more mos of survival |
|
|
Brain metastasis- prognosis
|
-Median survival w/o tx is 1-2 mos from discovery of brain tumor
-W/ corticosteroids, survival extends 2-4 mos -Median survival w/ steroids + radiotherapy is 3-6 mos -Increased ICP may trigger herniation |
|
|
Brain metastasis- pathophys
|
-Summary: Neoplasms that originate in tissues outside the brain and spread secondarily to involve the brain
-80% are supratentorial, 15% cerebellar, 5% in brainstem or spinal cord -25% discovered before or at the time of dx of primary tumor -Most common sources: lung (44%), breast, GI, GU, renal cell, melanoma, leukemia |
|
|
Neurofibroma-tosis 1- dif
|
-CNS neoplasm
-Spinal cord hemorrhage, infarction, abscess -NF2 |
|
|
Neurofibroma-tosis 1- hx
|
-First degree relative has NF1
|
|
|
Neurofibroma-tosis 1- phy
|
-Café-au-lait spots
-Axillary or inguinal freckles -Multiple neurofibromas -Iris hamartomas / Lisch nodules -Optic nerve glioma -Sphenoid dysplasia |
|
|
Neurofibroma-tosis 1- dx tests
|
-Sequencing of NF1 gene
-Plain films to detect bony abnormalities -Baseline CT -Annual eye exam |
|
|
Neurofibroma-tosis 1- tx
|
-Surgical removal of neurofibromas that press on vital structures, obstruct vision, or grow rapidly
|
|
|
Neurofibroma-tosis 1- progn
|
-Most live long and healthy lives,
-Life expectancy may be reduced by as much as 15 years -May increase HTN, sequelae of spinal cord lesions, and malignancy |
|
|
Neurofibroma-tosis 1- pathophys
|
-Autosomal dominant mutation in chromosome 17q12 (neurofibromin gene – tumor suppressor)
-Assoc. w/ pliocytic astrocytomas, optic nerve gliomas, malignant peripheral nerve sheath tumors (MPNST), osseous lesions, juvenile CML, pheochromocytoma, peripheral neuropathy, ADHD -Can become malignant, can grow on spinal cord |
|
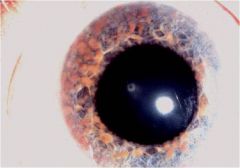
What type of disease does this person have
|
Neurofibroma-tosis 1
|
|
|
Neurofibroma-tosis 2-dif
|
-NF1
-Ependymoma -Meningioma -Juvenile cararacts |
|
|
Neurofibroma-tosis 2- hx
|
-Typical onset in early adulthood
-First degree relative affected -Tinnitus -Gradual hearing loss -Vestibular / balance dysfunction |
|
|
Neurofibroma-tosis 2- phys
|
-Bilateral acoustic neuromas (Schwannomas)
-Sensory motor polyneuropathy -Optic nerve sheath meningiomas -CN palsies d/t compression from expanding schwannoma -Subcutaneous neurofibromas |
|
|
Neurofibroma-tosis 2- dx test
|
-MRI: Bilateral eighth nerve masses
-Hearing evaluations |
|
|
Neurofibroma-tosis 2- prognosis
|
-Prognosis of NF2 depends on age of onset of symptoms, degree of hearing deficit, and number and location of various tumors
-Typically decreased lifespan |
|
|
Neurofibroma-tosis 2- pathophys
|
-Summary: AD multisystem genetic disorder associated with bilateral vestibular schwannomas, spinal cord schwannomas, meningiomas, gliomas, and juvenile cataracts with a paucity of cutaneous features
-Mutation in chromosome 22q12 (Merlin/schwannomin gene product, tumor suppressor) -Tumor grows along the nerve |
|
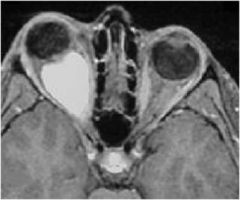
What type of tumor is seen here?
|
NFT2
|
|
|
Paraneoplastic neurological syndrome- phys
|
-Autonomic neuropathy: orthostatic hypotension, impaired pupillary light response, abnormal valsalva response, impotence
|
|
|
Paraneoplastic neurological syndrome- pathophys
|
- Small cell lung neoplasm Ca2+ ion channel Lambert-Eaton
-Thymoma ACh MG -Caused by or associated w/ a malignancy – antibodies against tumor & CNS -Paraneoplastic antibody (IgG) has a neural antigen target membrane dysfunction or focal damage to nerve or muscle |

