![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
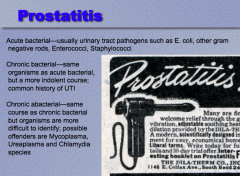
What are some pathogens that cause acute prostatitis?
What will you see a common history of in chronic bacterial version?
What are some offenders of chronic "abacterial?" |
|
|
|
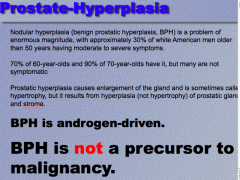
How many white men over age 50 have moderate to severe symptoms of nodular hyperplasia (BPH)?
What percent of 60 year olds have it? 70 year old? Are most symptomatic?
Is BPH hypertrophy or hyerplasia?
Is it androgen driven? Is it a precursor to malignancy? |
|
|
|
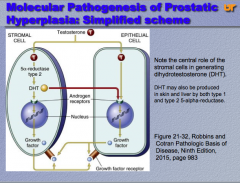
Prostatic hyperplasia is driven by ______ and is believed to mainly stem from impaired cell death, resulting in the accumulation of ______ cells.
|
Prostatic hyperplasia is driven by androgen and is believed to mainly stem from impaired cell death, resulting in the accumulation of senescent cells. |
|
|
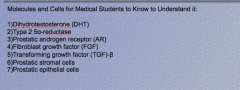
Draw out the pathway of prostatic hyperplasia:
|
|
|
|
|
|
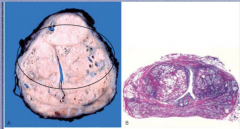
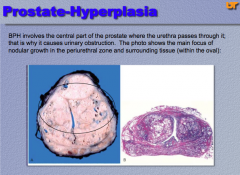
BPH involves which zone of the prostate? Why does it cause urinary obstruction? |
|
|
|
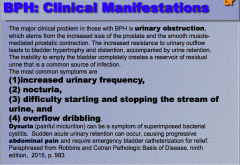
What is the major clinical problem in those with BPH? What major complications does this lead to (think higher up the tract)?
The most common symptoms of BPH (4)? 2 other non specific symptoms? |
|
|
|
“Mild cases of BPH may be treated without medical or _____ therapy, such as by ______ fluid intake, especially before ______; moderating the intake of ____ and caffeine-containing products; and following timed voiding schedules. The most commonly used and effective medical therapy for symptoms relating to BPH are _____-blockers, which ______ prostate smooth muscle tone via inhibition of _______ -adrenergic receptors. Another common pharmacologic therapy aims to decrease symptoms by physically shrinking the prostate with an agent that inhibits the synthesis of DHT. Inhibitors of ______ fall into this category. For moderate to severe cases recalcitrant to medical therapy, a wide range of more invasive procedures exist. ________ of the prostate (TURP) has been the gold standard in terms of reducing symptoms, improving flow rates, and decreasing post-voiding residual urine. It is indicated as a first line of therapy in certain circumstances, such as recurrent urinary _____. As a result of its morbidity and cost, alternative procedures have been developed. These include high-intensity focused ______, laser therapy, hyperthermia, transurethral _______, and transurethral needle _______ using radiofrequency.” |
“Mild cases of BPH may be treated without medical or surgical therapy, such as by decreasing fluid intake, especially before bedtime; moderating the intake of alcohol and caffeine-containing products; and following timed voiding schedules. The most commonly used and effective medical therapy for symptoms relating to BPH are α-blockers, which decrease prostate smooth muscle tone via inhibition of α 1 -adrenergic receptors. Another common pharmacologic therapy aims to decrease symptoms by physically shrinking the prostate with an agent that inhibits the synthesis of DHT. Inhibitors of 5-α-reductase fall into this category. For moderate to severe cases recalcitrant to medical therapy, a wide range of more invasive procedures exist. Transurethral resection of the prostate (TURP) has been the gold standard in terms of reducing symptoms, improving flow rates, and decreasing post-voiding residual urine. It is indicated as a first line of therapy in certain circumstances, such as recurrent urinary retention. As a result of its morbidity and cost, alternative procedures have been developed. These include high-intensity focused ultrasound, laser therapy, hyperthermia, transurethral electrovaporization, and transurethral needle ablation using radiofrequency.” |
|
|
______ of the prostate is the most common form of cancer in men, who have a one in ______ lifetime probability of being diagnosed with it. Cancer of the prostate is typically a disease of men over _____. The incidence increases from 20% in men in their 50s to __% in men between the ages of 70 and 80. Prostatic cancer is uncommon in _____ and most common among _____. Environment plays a role, as evidenced by the rise in the incidence in _____ immigrants to the US, though not nearly to the level of that of native-born Americans. Increased consumption of ___ or carcinogens present in charred red meats has been implicated. Dietary products suspected of preventing or delaying prostate cancer development include _____ (in cooked tomatoes, for instance), soy products, and vitamin ___. |
Adenocarcinoma of the prostate is the most common form of cancer in men, who have a one in six lifetime probability of being diagnosed with it. Cancer of the prostate is typically a disease of men over 50. The incidence increases from 20% in men in their 50s to 70% in men between the ages of 70 and 80. Prostatic cancer is uncommon in Asians and most common among blacks. Environment plays a role, as evidenced by the rise in the incidence in Japanese immigrants to the US, though not nearly to the level of that of native-born Americans. Increased consumption of fats or carcinogens present in charred red meats has been implicated. Dietary products suspected of preventing or delaying prostate cancer development include lycopenes (in cooked tomatoes, for instance), soy products, and vitamin D. |
|
|
______ play an important role in prostate cancer . Like their normal counterparts, the ______ and survival of prostate cancer cells depends on ______, which bind to the androgen receptor (AR) and induce the expression of ___-growth and pro-______ genes.
CAG Repeats |
Androgens play an important role in prostate cancer . Like their normal counterparts, the growth and survival of prostate cancer cells depends on androgens, which bind to the androgen receptor (AR) and induce the expression of pro-growth and pro-survival genes. CAG Repeats |
|
|
Molecular mechanisms of resistance to anti-androgen therapy:
The importance of ______ in maintaining the growth and survival of prostate cancer cells can be seen in the therapeutic effect of ______ or treatment with antiandrogens, which usually induce disease ______.
Most tumors eventually become resistant to ______ blockade through acquisition of hypersensitivity to ______ levels of androgen (e.g., through AR gene ______) ligand-independent AR activation (e.g., via splice variants that lack the ligand binding domain) mutations in ___ that allow it to be activated by ______ ligands, and other mutations or epigenetic changes that activate alternative signaling pathways, which may bypass the need for AR altogether including increased activation of the ______ signaling pathway (such loss of the ______ tumor suppressor gene), which is observed most often in tumors that have become resistant to ______ therapy. |
Molecular mechanisms of resistance to anti-androgen therapy The importance of androgens in maintaining the growth and survival of prostate cancer cells can be seen in the therapeutic effect of castration or treatment with antiandrogens, which usually induce disease regression. Most tumors eventually become resistant to androgen blockade through |
|
|
Familial Risk of Prostate Cancer
Compared with men with no family history, men with one first-degree relative with prostate cancer have _____ the risk and those with two first-degree relatives have ______ times the risk of developing prostate cancer.
Men with a strong family history of prostate cancer also tend to develop the disease at an ______ age.
Men with germline mutations of the tumor suppressor _____ have a 20-fold increased risk of prostate cancer, and a germline mutation in _______ , a homeobox gene encoding a transcription factor that regulates prostatic development, also confers substantially increased risk in the small percentage of families that carry it. However, the vast majority of familial prostate cancers are due to ______ in other loci that confer a small ______ in cancer risk. Family and genome-wide association studies have identified more than 40 risk-associated loci, which explain approximately ___% of the familial risk. |
Familial Risk of Prostate Cancer Compared with men with no family history, men with one first-degree relative with prostate cancer have twice the risk and those with two first-degree relatives have five times the risk of developing prostate cancer. Men with a strong family history of prostate cancer also tend to develop the disease at an earlier age. Men with germline mutations of the tumor suppressor BRCA 2 have a 20-fold increased risk of prostate cancer, and a germline mutation in HOXB13 , a homeobox gene encoding a transcription factor that regulates prostatic development, also confers substantially increased risk in the small percentage of families that carry it. However, the vast majority of familial prostate cancers are due to variation in other loci that confer a small increase in cancer risk. Family and genome-wide association studies have identified more than 40 risk-associated loci, which explain approximately 25% of the familial risk. |
|
|
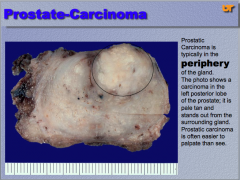
What is this? Where is prostatic carcinoma typically located? It is often easier to _____ than see. |
|
|
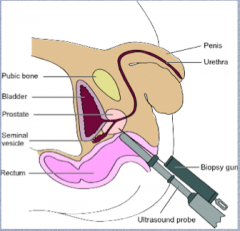
Prostate carcinoma diagnosis:
Detected by elevated level of _____ in blood or by physical examination (digital rectal examination) _____ is essential to make the diagnosis; here is a schematic diagram of the standard procedure for ______ needle biopsy of the prostate: |
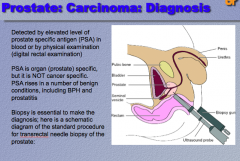
Only 1/10,000 of the prostate removed => high sampling error rate |
|
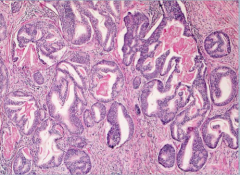
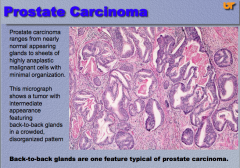
What is shown? Can it be variable in presentation?
What is one features of typical prostate carcinoma? |
|
|
|
Which is normal? Which is prostate cancer? Small glands are a feature of which? |
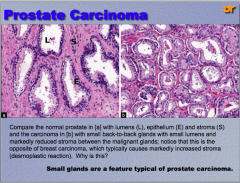
Normal gland also has little spindle-looking basal cells around the periphery of the gland. |
|
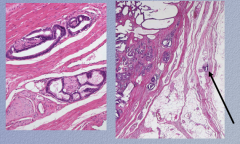
What is shown on the left and the right? |
Left = perineural invasion Right = extra capsular extension of the tumor |
|
|
How is the Gleason score calculated? |

7 and below does much better clinically
1 = best differentiated 5 = worst differentiated
Most predominant + 2nd most predominant |
|
|
1. Prostate biopsies are among the most ______ that pathologists have to diagnose. |
Prostate biopsies are among the most difficult that pathologists have to diagnose. |
|
|
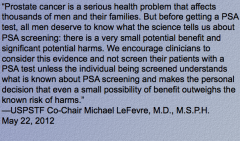
“As a screening test for prostate cancer, the use of ____ remains controversial in that it ______ both sensitivity and specificity. |
“As a screening test for prostate cancer, the use of PSA remains controversial in that it lacks both sensitivity and specificity. |
|
|
“Several refinements in the estimation and interpretation of PSA values are currently used. These include the ratio between the serum PSA value and ______ of prostate gland (PSA density), the rate of ______ in PSA value with time (PSA velocity), the use of ___-specific reference ranges, and the ratio of free and ______ PSA in the serum. Men with enlarged ______ prostate glands have higher total serum PSA levels than men with ______ glands. The measurement of serum PSA density factors out the contribution of benign prostatic tissue to serum PSA levels. It is calculated by dividing the total serum PSA level by the estimated gland ______ (usually determined by transrectal ultrasound measurements) to estimate the PSA produced per ______ of prostate tissue. As men age, their prostates tend to enlarge with ______. One would then anticipate that, overall, older men would have ______ serum PSA levels than younger men. The upper age-specific PSA reference ranges are ___ ng/mL for men 40 to 49 years of age, ___ ng/mL for men 50 to 59 years, ___ ng/mL for men 60 to 69 years, and ___ ng/mL for men 70 to 79 years. Consequently, a serum PSA value of ___, while it will appear as a normal value on a laboratory test, is a worrisome finding in a man in his 40s, warranting additional evaluation.” |
“Several refinements in the estimation and interpretation of PSA values are currently used. These include the ratio between the serum PSA value and volume of prostate gland (PSA density), the rate of change in PSA value with time (PSA velocity), the use of age-specific reference ranges, and the ratio of free and bound PSA in the serum. Men with enlarged hyperplastic prostate glands have higher total serum PSA levels than men with small glands. The measurement of serum PSA density factors out the contribution of benign prostatic tissue to serum PSA levels. It is calculated by dividing the total serum PSA level by the estimated gland volume (usually determined by transrectal ultrasound measurements) to estimate the PSA produced per gram of prostate tissue. As men age, their prostates tend to enlarge with BPH. One would then anticipate that, overall, older men would have higher serum PSA levels than younger men. The upper age-specific PSA reference ranges are 2.5 ng/mL for men 40 to 49 years of age, 3.5 ng/mL for men 50 to 59 years, 4.5 ng/mL for men 60 to 69 years, and 6.5 ng/mL for men 70 to 79 years. Consequently, a serum PSA value of 3.5, while it will appear as a normal value on a laboratory test, is a worrisome finding in a man in his 40s, warranting additional evaluation.” |
|
|
“Another means of interpreting serum PSA tests is to assess PSA ______ or the rate of ______ of PSA. Men with prostate cancer demonstrate a more rapid ______ in PSA levels over time than do men who do not have prostate cancer. The rate of change in PSA that best distinguishes between men with and without prostate cancer is ____ ng/mL per year. For this measurement to be valid, at least ______ PSA measurements must be performed over a period of 1.5 to 2 years, as there is substantial short-term variability (up to 20%) between repeat PSA measurements. A man who has a significant increase in serum PSA levels, even if the latest serum PSA test is below the normal cut-off (<4 ng/mL), should undergo additional work-up. Studies have revealed that immunoreactive ____ (the form detected by the widely used antibody test) exists in two forms: a major fraction bound to______ -antichymotrypsin and a minor free fraction. The percentage of free PSA (free PSA/total PSA × 100) is lower in men with ______ than in men with benign prostatic diseases.” |
“Another means of interpreting serum PSA tests is to assess PSA velocity or the rate of change of PSA. Men with prostate cancer demonstrate a more rapid increase in PSA levels over time than do men who do not have prostate cancer. The rate of change in PSA that best distinguishes between men with and without prostate cancer is 0.75 ng/mL per year. For this measurement to be valid, at least three PSA measurements must be performed over a period of 1.5 to 2 years, as there is substantial short-term variability (up to 20%) between repeat PSA measurements. A man who has a significant increase in serum PSA levels, even if the latest serum PSA test is below the normal cut-off (<4 ng/mL), should undergo additional work-up. Studies have revealed that immunoreactive PSA (the form detected by the widely used antibody test) exists in two forms: a major fraction bound to α 1 -antichymotrypsin and a minor free fraction. The percentage of free PSA (free PSA/total PSA × 100) is lower in men with prostate cancer than in men with benign prostatic diseases.” |
|
|
“Other genes that may serve as biomarkers in prostate cancer have emerged. ______is a noncoding RNA which is overexpressed in ______ of prostate cancers. A diagnostic test that quantifies urine PCA3 is currently used as an additional biomarker in patients suspected to have prostate cancer because of elevated______ Elevated urine ______ scores have been shown to be associated with an increased risk of a positive ______ biopsy in this setting. The combination of urinary PCA3 with screening of urine for ______ fusion DNA may have increased sensitivity and specificity compared to PSA screening alone.
Because many small cancers localized to the prostate may never progress to clinically significant invasive cancers, there is considerable uncertainty regarding the management of small lesions that are detected because of an elevated ____ level. This has created controversy about the role of widespread screening for prostate cancer.” |
Because many small cancers localized to the prostate may never progress to clinically significant invasive cancers, there is considerable uncertainty regarding the management of small lesions that are detected because of an elevated PSA level. This has created controversy about the role of widespread screening for prostate cancer.” |
|
|
In October 2011, the USPSTF posted for public comment the draft of its recommendation regarding prostate cancer screening. Since then, Task Force members have read the many comments received and reviewed the most up-to-date evidence. Based on this work, the Task Force concludes that many men are ______ as a result of prostate cancer screening and few, if any, benefit. A better test and better treatment options are needed. Until these are available, the USPSTF has recommended ______ screening for prostate cancer. |
In October 2011, the USPSTF posted for public comment the draft of its recommendation regarding prostate cancer screening. Since then, Task Force members have read the many comments received and reviewed the most up-to-date evidence. Based on this work, the Task Force concludes that many men are harmed as a result of prostate cancer screening and few, if any, benefit. A better test and better treatment options are needed. Until these are available, the USPSTF has recommended against screening for prostate cancer. |
|
|
|
|
|
No screening for men under _____ |
No screening for men under 40 |
|

Bone metastases are very common. Are they almost always osteoblastic or osteolytic? |
Osteoblastic!
BLASTIC METASTASES = PROSTATE CANCER!
|
|

What is shown in this bone metastasis? |
Reactive bone formation in metastasis due to prostate cancer leads to the dense, “osteoblastic” nodular lesions seen in this metastasis to femur. |
|
|
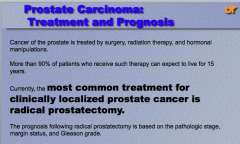
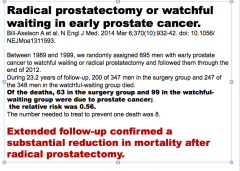
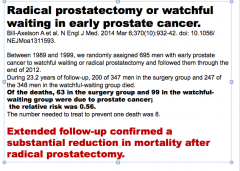
More than 90% of prostate cancer patients who receive therapy can expect to live for how long?
What is the most common treatment for clinically localized prostate cancer? |
|
|
|
Alternative treatments for localized prostate cancer are either ______-beam radiation therapy or _______ radiation therapy, the latter consisting of placing radioactive seeds throughout the prostate (____therapy). External-beam radiation therapy is also used to treat prostate cancer that is too locally ______to be cured by surgery. Androgen deprivation may be achieved by orchiectomy, or by administration of synthetic analogs of ______ hormone-releasing hormone (LHRH) which suppress normal LHRH, achieving, in effect, a pharmacologic orchiectomy. Other agents decrease levels of local and circulating androgens by inhibiting systemic steroid hormone synthesis. Although androgen deprivation therapy induces remissions, eventually tumors become ______ to testosterone withdrawal, an event that is a harbinger of disease progression and death. |
Alternative treatments for localized prostate cancer are either external-beam radiation therapy or interstitial radiation therapy, the latter consisting of placing radioactive seeds throughout the prostate (brachytherapy). External-beam radiation therapy is also used to treat prostate cancer that is too locally advanced to be cured by surgery. Androgen deprivation may be achieved by orchiectomy, or by administration of synthetic analogs of luteinizing hormone-releasing hormone (LHRH) which suppress normal LHRH, achieving, in effect, a pharmacologic orchiectomy. Other agents decrease levels of local and circulating androgens by inhibiting systemic steroid hormone synthesis. Although androgen deprivation therapy induces remissions, eventually tumors become resistant to testosterone withdrawal, an event that is a harbinger of disease progression and death. |
|
|
|

