![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Low potency, short duration |
💊 Procaine 💊 Chloroprocaine |
|
|
|
Intermediate potency and duration |
💊 lidocaine 💊 prilocaine |
|
|
|
High potency, long duration |
Tetracaine (Amethocaine) Bupivacaine Ropivacaine Dibucaine (Cinchocaine) |
|
|
|
Surface anaesthetic Soluble |
💊 Cocaine 💊 Lidocaine 💊 Tetracaine 💊 Benoxinate |
|
|
|
Surface anaesthetic Insoluble |
💊 Benzocaine 💊 Butylaminobenzoate (Butamben) 💊 Oxethazaine |
|
|
|
Ester-linked LAs . |
💊 Cocaine, 💊 procaine, 💊 chloroprocaine, 💊 tetracaine, 💊 benzocaine |
|
|
|
Amide-linked LAs |
💊 Lidocaine, 💊 bupivacaine, 💊 dibucaine, 💊 prilocaine, 💊 ropivacaine. |
|
|
|
Mechanism of action |
➖ block nerve conduction by decreasing the entry of Na+ ions during upstroke of action potential ➖ local depolarization fails to reach the threshold potential and conduction block ensues |
|
|
|
Mechanism of action |
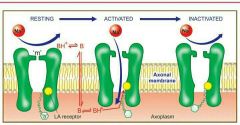
|
|
|
|
Lidocaine |
💥 good both for surface application as well as injection 💥 Injected around a nerve it blocks conduction within 3 min 💥 Vasodilatation occurs in the injected area 💥 Cross sensitivity with ester LAs is not seen 💥 early central effects of lidocaine are depressant 💥 Lidocaine is a popular antiarrhythmic 💥 ADR same as others |
|
|
|
Uses of lidocaine |
💉 surface application, 💉 infiltration, 💉 nerve block 💉 epidural, 💉 spinal and intravenous regional block anaesthesia |
|
|
|
Eutectic lidocaine/prilocaine |
📖 This is a unique preparation which can anaesthetise intact skin after surface application 🎆 lidocaine and prilocaine are mixed in equal proportion at 25°C. 🎆 The resulting oil is emulsified into water to form a cream 🎆 applied under occlusive dressing for 1 hr before i.v. cannulation, split skin graft harvesting and other superficial procedures. 🎆 Anaesthesia up to a depth of 5 mm lasts for 1–2 hr after removal. 🎆 used as an alternative to lidocaine infiltration. |
|
|
|
Bupivacaine |
potent and long-acting amidelinked LA used for infiltration, nerve block, epidural and spinal anaesthesia of long duration 0.25–0.5% solution injected epidurally produces adequate analgesia without significant motor blockade Uses :obstetrics and postoperative pain relief by continuous epidural infusion ADR :prolong QTc interval and induce ventricular tachycardia or cardiac depression |
|
|
|
Why bupivacaine is popular in obstetrics |
💉 produces adequate analgesia without significant motor blockade so mother can actively cooperate in vaginal delivery 💉 has high lipidsolubility; distributes more in tissues than in blood after spinal/epidural injection. Therefore, it is less likely to reach the foetus to produce neonatal depression |
|
|
|
Conduction block |
The LA is injected around nerve trunks so that the area distal to injection is anaesthetised and paralysed. Choice of the LA and its concentration is mainly dictated by the required duration of action; lidocaine(1–2%) with intermediate duration of action is most commonly used, but for longer lasting anaesthesia bupivacaine may be selected. |
|
|
|
Spinal anesthesia |
The LA is injected in the subarachnoid space between L2–3 or L3–4 Lower abdomen and hind limbs are anaesthetised and paralysed Nerve roots rapidly take up and retain the LA, therefore, its concentration in CSF falls quickly after injection The level of anaesthesia does not change with change of posture (becomes fixed) after 10 min. |
|
|
|
Women during late pregnancy require less drug for spinal anaesthesia, |
because inferior vena cava compression leads to engorgement of the vertebral system and a decrease in the capacity of subarachnoid space |
|
|
|
Advantages of spinal anaesthesia over general anaesthesia are: |
(i) It is safer. (ii) Produces good analgesia and muscle relaxation without loss of consciousness. (iii) Cardiac, pulmonary, renal disease and diabetes pose less problem. |
|
|
|
Complications of spinal anesthesia |
Respiratory paralysis Hypo tension Headache Cauda equina syndrome Septic meningitis Nausea and vomiting |
|
|
|
Pre anaesthetic medication |
Opioids, H2 blockers, Sedatives, Anticholinergics, Neuroleptics Antiemetics |
OHSANA |

