![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
253 Cards in this Set
- Front
- Back
|
A form of cytomegalovirus acquired during adulthood.
|
acute acquired CMV:
|
|
|
Immunity achieved through previous exposure to infectious microorganisms.:
|
active immunity
|
|
|
The least severe form of poliomyelitis, in which short-lived symptoms include fever, uneasiness, sore throat, headache, anorexia, vomiting, and abdominal pain; also known as unapparent poliomyelitis.
|
abortive poliomyelitis:
|
|
|
The body’s defense mechanism; occurs when B lymphocytes transform into plasma cells and manufacture antibodies. Also known as the humoral immune response.
|
antibody immune response:
|
|
|
:Cells that are responsible for humoral immunity; they mature in the bone marrow and become memory cells or plasma cells that lead to antibodies.
|
B cells
|
|
|
arthralgias:
|
Instances of joint pain.
|
|
|
atelectasis:
|
Lung collapse.
|
|
|
Single-celled microorganisms that may produce disease.
|
bacteria:
|
|
|
The body’s defense mechanism that occurs when T lymphocytes turn into cytotoxic killer T cells to attack pathogens.
|
cellular immune response:
|
|
|
A gram-positive, spore-forming bacterium that allows microorganisms to spread through direct contact, resulting in fever, diarrhea, and nausea.
|
Clostridium difficile:
DX: Stool testing or Imagery lookin for psuedomembranes |
|
|
Spreading from the trunk to the face and proximal extremities, as in the case of a rash.
|
centripetal:
|
|
|
An infection caused by several species of gram-negative bacteria transmitted via contaminated food or water; common symptoms include diarrhea, dehydration, nausea, vomiting, and fever.
|
cholera:
tx=tetracycline- to reduce duration of diahrrea |
|
|
A highly contagious disease caused by the Varicella zoster virus; also known as varicella. Spread primarily through airborne respiratory secretions or person-to-person contact; symptoms include fever and a characteristic rash.
|
chicken pox:
2-3 weeks incubation period tx=cool baths calamine lotions benadryl tylenol Acycolvir |
|
|
chancre:
|
A painless lesion at the site of an infection.
|
|
|
A form of bacteria found in animal food sources and transmitted via fecal-oral means; one of the main causes of food-borne illness.
|
Campylobacter:leads to Enterotoxin release
main cause of foos borne disease dx: stool sample/culturing tx: supportive measures toward symptoms |
|
|
A process by which circulating plasma proteins produced in the liver are activated when an antibody couples with an antigen, or when endotoxins are released; ultimately results in cell lysis and death.:
|
complement system
|
|
|
The most severe form of congenital cytomegalovirus; symptoms may include jaundice, enlarged liver and spleen, a purplish rash, and fever.:
|
cytomegalic inclusion disease
|
|
|
A herpes-family virus with many strains; transmitted through person-to-person contact. The leading cause of congenital viral infections in North America.
|
cytomegalovirus (CMV):
handwashing is the best defense |
|
|
A form of cytomegalovirus in which infected women transmit the virus to their babies during birth.
|
congenital CMV:
|
|
|
coryza:
|
Upper respiratory infection.
|
|
|
An illness caused by Corynebacterium diphtheriae; transmitted through direct contact with the respiratory secretions of an infected host. <BR><BR>Symptoms may include nasal discharge, sore throat, fever, cough, and swollen lymph nodes, bluish tint to skin due to inadequate oxygenation
|
Diphtheria:
TX=penicillin or erythtomycin and can cause myocarditis/neuritits dx: sympotoms then confirmed with throat swab and cultures |
|
|
Particles one to five micrometers in diameter that, when suspended in the air, may be inhaled by susceptible individuals, resulting in illness.
|
droplet nuclei:
|
|
|
Indigestion is also known as ___________________ ?
|
dyspepsia:
|
|
|
desquamation:
|
Peeling of the skin.
|
|
|
A form of cytomegalovirus acquired by individuals who are immunosuppressed, especially those who have had a transplant.
|
generalized systemic CMV:
leukopenia pneumonitis best preventive measure is good handwashing |
|
|
Tissue masses composed of living and dead bacilli.
|
granuloma:
|
|
|
A protozoan transmitted through contaminated food, drink, or water containing viable cysts of the organism.:
|
Giardia lamblia
SX; Abd pain with watery stools, fatigue and weight loss TX: Albenzazole, Flagyl, Furizolidone |
|
|
The center of the fibrous tissue mass that surrounds a granuloma.
|
Ghon’s tubercle:
|
|
|
An illness caused by the rubella virus that is transmitted primarily through nasopharyngeal secretions; also known as rubella. Symptoms can include fever, malaise, headache, upper respiratory infection, and rash.14-21 days incubation
|
German measles:
bedrest tylenol isolation |
|
|
The hepatitis B core antigen; presence of an antibody to this antigen indicates the continuing presence of hepatitis B in the liver during the acute phase of illness.
|
HBcAg:
|
|
|
A viral infection of the liver usually passed through fecal-oral transmission; typically associated with contaminated food, but may also be sexually transmitted.
|
hepatitis A:
|
|
|
A surface antigen; detection of the antibody to this antigen indicates late convalescence, recovery, and the development of immunity to hepatitis B.
|
HBsAg:
|
|
|
A gene product of hepatitis B DNA; presence of antibodies to this antigen indicates ongoing replication of hepatitis B.
|
HBxAg:
|
|
|
A condition in which red blood cells are destroyed and the kidneys fail
|
hemolytic uremic syndrome (HUS)
usually in children under 5 who have suffered from E. Coli |
|
|
A form of viral hepatitis transmitted by blood through a percutaneous or mucosal route; replicates in the liver, but lingers in the blood serum.
|
hepatitis B (HBV):
SX: Arthralgia, Dyspepsia |
|
|
An independent protein and hepatitis B antigen circulating in the blood; presence of antibodies to this antigen usually indicates reduced infectivity.
|
HBeAg:
|
|
|
An illness caused by the Sin nombre virus; transmitted to humans through direct or indirect contact with rodents.
|
hantavirus pulmonary syndrome (HPS):
if left untreaded can cause SOB, Resp. Problems Low BP, Low Platelet count Ribivirin may be given to slow the Virus |
|
|
A virus that causes various types of skin infections characterized by blister-like lesions;transmitted through direct contact.
|
herpes simplex:
|
|
|
A viral infection resulting in blister-type lesions in the genital area.
|
herpes simplex 2 (HSV-2):
|
|
|
A viral infection resulting in blister-type lesions around the mouth.
|
herpes simplex 1 (HSV-1):
|
|
|
The body’s defense mechanism; occurs when B lymphocytes transform into plasma cells and manufacture antibodies. Also known as the antibody immune response.
|
humoral immune response:
|
|
|
The state in which a person is protected from specific microorganisms.
|
immunity:
|
|
|
A pathological condition of the body that occurs when a host becomes ill due to infection and presents a group of clinical signs, symptoms, and laboratory findings.
|
infectious disease:
|
|
|
Localized hardening of the skin.
|
induration:
|
|
|
: A multisystem illness caused by Legionella pneumophila, a gram-negative bacteria transmitted to the respiratory tract through inhalation of aerosols produced by an environmental source. Commonly referred to as Legionnaires’ disease.
|
legionellosis
2-10 days incubation contracted thru aerosols produced by water towers, humidifiers, shower heads, water coolers SX; Malaise, Dry cough DX: Sputum, Blood or Urine antibiotic therapy zithromax erythtomycin levoflaxcin |
|
|
A condition in which there is a low number of circulating white blood cells.
|
leukopenia:
|
|
|
A disease caused by the spirochete Borrelia burgdorferi; transmitted to humans by ticks. Symptoms range from rash and lymphadenopathy to serious neurological manifestations such as Bell’s palsy and Guillain-Barré-like syndrome.
|
Lyme disease:
lab diagnoses not specific ABO treatment |
|
|
Swelling of the lymph nodes.
|
lymphadenopathy:
|
|
|
Small, irregular red spots with a tiny, bluish-white center; seen on the buccal mucosa opposite the molars two days before measles rash appears.
|
Koplik’s spots:
|
|
|
A severe bacterial infection that affects the blood and meninges; transmitted via the nose or throat discharge of infected individuals.
|
meningococcal meningitis:
|
|
|
The main diagnostic test for tuberculosis in which a purified protein derivative of the TB bacillus is given intradermally to evaluate cell-mediated immunity.
|
Mantoux test:
|
|
|
A virus that causes symptoms including fever, malaise, upper respiratory infection, Koplik’s spots, and rash; may be transmitted through the respiratory secretions, blood, and urine of an infected person. Also known as rubeola.
10-20 days incubation |
measles
tx=bedrest fever reducing drugs |
|
|
The means by which disease spreads from one host to another.
|
mode of transmission:
|
|
|
An illness caused by paramyxovirus and transmitted by direct contact with the saliva or respiratory secretions of an infected person. Common symptoms include fever, headache, earache, and parotitis.
|
Mumps
14-21 days incubation may cause epididymo-orchitis tx=IBU,Tylenol and Bedrest |
|
|
Inflammation of the middle muscle layer of the heart.
|
myocarditis:
a complication of diptheia |
|
|
A severe form of poliomyelitis; symptoms include pain and stiffness in the neck, back, and legs.
|
nonparalytic poliomyelitis:
|
|
|
A syphilitic infection of the central nervous system that can lead to dementia, psychosis, paresis, stroke, or meningitis.
|
neurosyphilis:
|
|
|
Nerve degeneration accompanied by pain.
|
neuritis:
|
|
|
Infections by organisms that wouldn’t normally cause disease, but are able to do so because of a patient’s already weakened state.
|
opportunistic infections:
|
|
|
An illness caused by Bordetella pertussis and transmitted through direct contact with or via droplets from the respiratory tract of an infected person;
primary symptom is forceful coughing. Also known as whooping cough. (paroxsym) |
pertussis
5-21 days incubation zithromax erythtomycin bedrest |
|
|
Rapid cough followed by sudden inspiration.
|
paroxysm:
|
|
|
The most severe form of poliomyelitis; complications can include permanent central nervous system paralysis, respiratory arrest, hypertension, and kidney stones.
|
paralytic poliomyelitis:
|
|
|
Protection achieved through natural or innate immunity against microorganisms, or by vaccination.
|
passive immunity:
|
|
|
Microorganisms that infect the body by attaching to systems, infecting those systems, and causing symptoms.
|
parasites:
|
|
|
The body’s defense mechanism; occurs when white blood cells (granulocytes and macrophages) move to the site of infection where they engulf and destroy the foreign invaders.
|
phagocytic immune response:
|
|
|
Illness caused by enteroviruses (type 1, 2, or 3); transmitted by contact with the saliva or feces of an infected person. Symptoms can range from fever and malaise to central nervous system paralysis.
|
poliomyelitis:
7-14 days incubation period Eradicated in US TX=Analgesics and in worse cases Ventilators |
|
|
A virus that carries genetic material in ribonucleic acid (RNA) instead of deoxyribonucleic acid (DNA).
|
retrovirus:
|
|
|
Supplements that contain beneficial bacteria to help restore the colon’s natural flora.
|
probiotics:
|
|
|
A virus that occurs after permanent infection is established.
|
provirus:
|
|
|
A condition that occurs when an infection in one part of the body serves as a source of blood contamination.
|
secondary bloodstream infection:
|
|
|
Gram-negative bacteria that invade the lumen of the intestine; spread through oral-fecal transmission. Severe diarrhea is the most common symptom.
|
Shigella:
poor hygiene most contributing factor'pediatric population being the most affected TX: fluids ABO therapy |
|
|
A gram-negative bacillus with many species, including the pathogenic S. typhi (typhoid fever). The organism lives in the intestines and is shed in the feces; commonly found in chicken, eggs, raw milk, and sometimes beef. Symptoms of infection can include nausea, vomiting, diarrhea, and abdominal pain.
|
Salmonella:
|
|
|
Cells that reside in lymphoid tissue and migrate to the thymus gland where they directly attack foreign invaders and produce cellular or cell-mediated immunity
T- for Thymus |
T cells:
|
|
|
An organism that does not by itself cause disease, but harbors a microorganism that leads to infection.
|
vector:
|
|
|
List the three immune responses in which the body attacks foriegn invaders.
|
The phagocytic immune response occurs when WBCs move to the site of invasion and engulf and thereby destroy the foreign invaders.
The humoral or antibody immune response occurs when B lymphocytes transform themselves into plasma cells and manufacture antibodies. These antibodies are then transported in the bloodstream to disable the invaders. The cellular immune response occurs when T lymphocytes turn into cytotoxic killer T cells and attack pathogens. |
|
|
When does HIV go to full blown AIDS?
|
T4 count drops to 200 cells per mm3 or less and/or he or she has an opportunistic infection.
|
|
|
The main diagnostic test for tuberculosis is the tuberculin skin test, also called the?
|
Mantoux test. .
|
|
|
WHo is at risk for bacterial meningitis?
|
Adolescents, especially college students living in dormitories, are at increased risk for bacterial meningitis. Other people at increased risk include those who have contact with the household of a person known to have had this disease, those who are immunocompromised, and those who are traveling to parts of the world where meningococcal meningitis is prevalent.
|
|
|
Chlamydia is treated with antibiotics, such as?
|
doxycycline taken twice a day for seven days or azithromycin (Zithromax) taken in a single dose. Persons being treated for chlamydia should not have sexual contact for seven days after single-dose therapy or until completion of all days of treatment in multidose therapy.
|
|
|
Some reasons for the increase in emerging infections include the following:
|
An increase in global travel
Globalization of the food supply Population growth Human migration and overcrowding Risky human behavior Increased antimicrobial resistance Breakdown in public health measures that ensure safe food protection and handling |
|
|
A condition in which passive flexion of a lower extremity produces similar action on the opposite extremity.
|
Brudzinski’s sign:
|
|
|
An abnormal passage within the body.
|
fistula:
|
|
|
A condition in which the leg cannot be completely extended when the thigh is flexed.
|
Kernig’s sign:
|
|
|
Blood in the stool
|
melena:.
|
|
|
Skin lesions that are less than 0.5 centimeters in width and solid, such as warts.
|
papules:
|
|
|
Stiffness in the neck.
|
nuchal rigidity:
|
|
|
Pus-filled vesicles, as seen in acne, impetigo, furuncle, or carbuncles.
|
pustules:
|
|
|
Tumorlike skin lesions seen in cases of carcinoma.
|
nodules:
|
|
|
Pus in the urine.
|
pyuria:
|
|
|
The outer layer of the epidermis that serves to regulate water balance and provide a barrier to chemicals, microbes, insect bites, and trauma.
|
stratum corneum:
|
|
|
Skin lesions that are less than 0.5 centimeters in diameter and circumscribed with an elevated palpable mass containing serous fluid.
|
vesicles:
|
|
|
a dry, irritating cough is characteristic of
|
an upper-airway viral infection;
|
|
|
a high-pitched cough is characteristic of
|
obstruction
|
|
|
brassy cough
|
tracheal infections
|
|
|
Coughing at night may be more indicative of
|
left-sided heart failure or bronchial asthma,
|
|
|
In the morning, a productive cough may indicate
|
bronchitis
|
|
|
coughing in a supine may indicate
|
Sinusitis
|
|
|
Intermittent fever vs. remittent fever
|
Intermittent fever may return to normal once or several times in a twenty-four hour period; on the other hand, remittent fever fluctuates but does not return to normal.
|
|
|
To determine the effects of illness on a patient’s self-concept, the nurse can ask questions such as
|
“How do you feel about your life in general?” and “Do you have any concerns about your body?”
|
|
|
White blood cells that fight invasion by releasing cell mediators to engulf foreign or toxic substances
|
granular leukocytes:
|
|
|
Monocytes and macrophages that function as phagocytic cells to engulf, ingest, and destroy foreign invaders.
|
nongranular leukocytes:
|
|
|
Cells that work to engulf, ingest, and destroy foreign invaders.
|
phagocytic cells:
|
|
|
With natural immunity, certain natural and chemical barriers prevent pathogens from gaining access to the body; these include ?
|
physical barriers, the cilia of the respiratory tract, natural responses, acidic gastric juices, enzymes in tears and saliva, substances in sebaceous and sweat secretions, and interferons.
|
|
|
An allergic reaction characterized by toxic epidermal necrolysis in which the epidermis separates from the dermis.
|
Stevens-Johnson syndrome:
|
|
|
A technique developed by Dolores Kreiger and Dora Kunz in the early 1970s; involves a therapist moving his or her hands over the body of the patient to achieve relaxation and promote healing.
|
therapeutic touch:
|
|
|
The following problems with the cardiovascular system may be indicative of infection:
|
Sepsis
Elevated temperature Hypotension Tachycardia Dysrhythmia Vasculitis Anemia |
|
|
Acute inflammation of the gallbladder as a result of trauma, burns, major surgery, cystic duct obstruction, primary bacterial infection, or multiple blood transfusions.
|
acalculous cholecystitis:
|
|
|
Also known as sliding hernia; occurs when the upper stomach and the gastroesophageal junction are displaced upward and slide in and out of the thorax.
|
axial hernia:
|
|
|
The administration of agents that bind with metals in the blood and convert them to a chemically inert form that can be excreted without further interaction with the body.
|
chelation therapy:
|
|
|
A surgical procedure in which an incision is made into the common duct for removal of gallstones; usually requires insertion of a tube to drain bile and edema.
|
choledochostomy:
|
|
|
A condition in which a gallstone obstructs the gallbladder’s bile outflow.
|
calculous cholecystitis:
|
|
|
A condition in which the gallbladder is filled with purulent fluid.
|
empyema:
|
|
|
Also known as ulcerative colitis; a recurrent ulcerative and inflammatory disease of the mucosal layer of the colon and rectum.
|
granulomatous colitis:
|
|
|
An endoscopic medical procedure that uses extracorporeal shock waves to fragment gallstones so that they then can pass out of the body.
|
intracorporeal lithotripsy:
|
|
|
A medical procedure that uses extracorporeal shock waves to fragment gallstones so that they then can pass out of the body.
|
lithotripsy:
|
|
|
A type of physical trauma that occurs when all or part of the stomach pushes up through the diaphragm.
|
paraesophageal hernia:
|
|
|
An autoimmune disease brought about by a combination of genetic, hormonal, and environmental factors; can be acute or insidious and may involve multiple body systems.
|
systemic lupus erythematosus (SLE):
|
|
|
The urge to defecate.
|
tenesmus:
|
|
|
A substance created by the conversion of bilirubin in the small intestine, partly excreted in feces and urine and partly absorbed into portal blood.
|
urobilinogen:
|
|
|
The two types of Hiatal Hernias?
|
Hiatal hernia can be classified as either axial or paraesophageal.
Axial or sliding hernia occurs when the upper stomach and the gastroesophageal junction are displaced upward and slide in and out of the thorax. Paraesophageal hernia occurs when all or part of the stomach pushes up through the diaphragm. This condition is less common than axial hernia. |
|
|
The best H2 receptor antagonist for critically ill patients with peptic ulcer disease is?
|
famotidine (Pepcid), because it is known to have the lowest risk of interaction with drugs other than cimetidine and does not alter drug metabolism in the liver.
|
|
|
The amount of tension the ventricles develop before contraction to eject blood to the arteries.
|
afterload:
|
|
|
The volume of blood that fills the ventricles at the end of diastole.
|
preload:
|
|
|
Also known as normal anion gap acidosis; metabolic acidosis that results from the direct loss of bicarbonate.
|
hyperchloremic acidosis:
|
|
|
A clinical disturbance characterized by a high blood pH and a high plasma bicarbonate concentration; can be caused by a gain of bicarbonate or a loss of H+.
|
metabolic alkalosis:
|
|
|
A clinical disturbance characterized by a low blood pH and a low plasma bicarbonate concentration; can be subcategorized as high anion gap acidosis or normal anion gap acidosis.
|
metabolic acidosis:
|
|
|
Metabolic acidosis vs. Metabolic alkalosis
|
Metabolic acidosis is characterized by a low blood pH (increased H+ concentration) and a low plasma bicarbonate concentration. Conversely, metabolic alkalosis is characterized by a high blood pH (decreased H+ concentration) and a high plasma bicarbonate concentration.
|
|
|
Clinical manifestations include tingling of the fingers and toes, dizziness, and hypertonic muscles, which are all related to decreased calcium ionization. The patient’s respiratory rate will also be decreased as a compensatory mechanism. As the patient’s blood pH rises above 7.6 and hypokalemia develops, ventricular disturbances may occur, decreased GI motility may occur, and paralytic ileus may develop.
|
acute metabolic alkalosis
|
|
|
Pediatric patients are at risk for more serious problems following tissue trauma because ?
|
they have less surface area to dissipate the injury, more rapid metabolism, and a greater risk for accidents or ingestion of toxic products.
|
|
|
Specific nursing responsibilities related to chelating agents include the following:
|
Seeking information about possible penicillin allergies (these drugs are related to chelating agents)
Monitoring the patient’s symptoms (especially joint pain) Reviewing liver function tests Monitoring urinalysis, complete blood counts, and platelet levels |
|
|
Massive dilation of blood vessels attributable to a neurological cause.
|
neurogenic shock:
|
|
|
A position in which the patient is placed on his or her back with knees and hips flexed and feet in stirrups; allows surgery of the perineum, rectum, and vagina.
|
lithotomy position:
|
|
|
Excess carbon dioxide in the blood.
|
hypercapnia:
|
|
|
An inherited muscle disorder chemically induced by anesthetic gases that trigger a set of actions leading to hypermetabolism of the muscles and, ultimately, to hyperthermia.
|
malignant hyperthermia:
|
|
|
increased amounts of ________________are critical for tissue synthesis and immune function, and they increase a person’s resistance to infection. Thus, deficiency can lead to impaired healing related to decreased collagen synthesis; impaired immune function; and increased risk of infection.
|
vitamin A
|
|
|
Impaired coordination of movement.
|
ataxia:
|
|
|
Also known as Lou Gehrig’s disease; a chronic, fatal, rapidly progressive motor neuron disease that eventually causes paralysis of the respiratory system.
|
amyotrophic lateral sclerosis (ALS):
|
|
|
akathisia:
|
Motor restlessness.
|
|
|
The inability to perform a previously learned action.
|
apraxia:
|
|
|
Removal of the atherosclerotic plaque or thrombus from the carotid artery.
|
carotid endarterectomy:
|
|
|
Uncoordinated dancelike motions of the trunk and extremities; often characteristic of Huntington’s disease.
|
chorea:
|
|
|
A type of ischemic stroke that has no known cause.
|
cryptogenic stroke:
|
|
|
A partial seizure in which the patient remains motionless or moves automatically but inappropriately for the time and place; the patient may also experience exaggerated emotions.
|
complex partial seizure:
|
|
|
Muscle rigidity associated with Parkinson’s disease; characterized by resistance to passive limb movement.
|
cogwheel rigidity:
|
|
|
Difficulty speaking or demonstration of poor intelligible speech due to paralysis of the speech-related muscles following a stroke.
|
dysarthria:
|
|
|
Also known as small penetrating artery thrombosis; a type of ischemic stroke that affects one or more small vessels. The most common form of ischemic stroke.
|
lacunar stroke:
|
|
|
A type of ischemic stroke that occurs due to atherosclerosis of the large blood vessels within the brain and thrombosis formation.
|
large artery thrombosis:
|
|
|
A variant of Guillain-Barré syndrome that primarily affects the eyes; it also causes loss of reflexes and severe ataxia.
|
Miller-Fischer syndrome:
|
|
|
An autoimmune disorder of neuromuscular transmission at the myoneural junction in which an antibody destroys normal postsynaptic receptors located on voluntary skeletal muscle.
|
myasthenia gravis (MG):
|
|
|
An episode of neurological dysfunction that occurs when there is an impairment of blood flow to a particular area of the brain, It last longer than twenty-four hours, but resolve within twenty-one days and do not involve neurological deficit.
|
reversible ischemic neurological deficits (RINDs):
|
|
|
a chronic, degenerative, progressive disease of the central nervous system characterized by patches of demyelination in the brain and spinal cord. Onset is more common among young adults (twenty to forty years of age) living in northern climates, and more women are affected than men.
|
Multiple sclerosis (MS) is
|
|
|
a chronic, progressive, hereditary disease of the nervous system that results in progressive involuntary choreiform (dancelike) movements and dementia. With this disease, choking is a problem because swallowing and chewing are difficult. Choreiform movements persist but diminish during sleep. Cognitive changes involve dementia as well as mental and emotional irregularities. Patients may be angry, depressed (often suicidal), nervous, irritable, and impatient. Judgment and memory are also affected. Paranoid thinking, delusions, and hallucinations may precede the appearance of disjointed thinking.
|
Huntington’s disease (HD) is
|
|
|
The three cardinal signs of Parkinson’s disease are
|
tremor
rigidity bradykinesia. |
|
|
extreme skeletal muscle weakness and fatigue, which worsens with activity and may be relieved by rest. The muscle groups most commonly affected are those involved with breathing, swallowing, head control, chewing, speech, and eye movement (leading to diplopia and ptosis). Patients have a sleepy and masklike appearance because of the effects of MG on these muscle groups. Laryngeal involvement leads to dysphonia, which gives a nasal sound to speech and makes articulation difficult. Weakness of the bulbar muscles presents swallowing difficulties and danger for choking. Progressive weakness of the diaphragm and intercostals makes breathing more difficult.
|
myasthenia gravis (MG) are
|
|
|
Nursing care for patients with ALS should focus on
|
supporting self-care abilities and family resources. Care activities include supporting nutrition, sleep, general health, and comfort. Ethical end-of-life issues have to be considered before the use of a gastrostomy tube or a ventilator. These efforts will prolong but not preserve the patient’s life. The family and the patient need to understand the nature and progress of the disease and make decisions before the patient’s inevitable decline.
|
|
|
The five emergency interventions necessary when dealing with a potential spinal cord injury at the scene of the accident are as follows:
|
Rapid assessment
Immobilization of the head and spine (assume injury until ruled out) Extrication Stabilization of life-threatening injuries Transportation to an appropriate care facility |
|
|
Slow, squirming, writhing movement.
|
athetosis:
SX: of basal ganglia damage |
|
|
Occurs when Cushing’s reflex is no longer effective;
consists of: bradycardia hypertension bradypnea. |
Cushing’s triad:
|
|
|
Cushing’s reflex:
|
In the event of autoregulation failure, the brain’s attempt to restore blood flow by increasing arterial blood pressure to overcome rising intracranial pressure.
|
|
|
The ability of the brain to automatically change the diameter of its blood vessels to maintain constant cerebral perfusion pressure.
|
autoregulation:
|
|
|
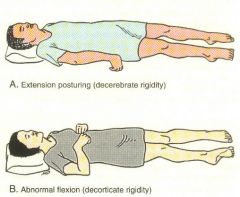
Decebrate
Decorticate |
|
|
A vertical band of cells within each cerebral hemisphere that governs the voluntary movements of the body.
|
motor cortex:
|
|
|
A relationship illustrating that if there is a change in one cranial compartment, there must be reciprocal changes in the other compartments to maintain equilibrium by displacing or shifting the contents. If a compensatory change does not occur, intracranial pressure will rise, thus precipitating a number of changes.
|
Monro-Kellie hypothesis:
|
|
|
What role does the Thalmus play in sensation?
|
The thalamus is a major receiving and transmitting center for the afferent sensory nerves and serves to integrate sensory impulses (except olfaction). It thereby plays a prominent role in conscious awareness of pain; recognition of variations in temperature and touch; sensation of movement; sensation of position; and recognition of the size, shape, and quality of objects.
|
|
|
Immediate treatment of increased intracranial pressure is aimed at decreasing cerebral edema, lowering the volume of cerebrospinal fluid, or decreasing blood volume while maintaining cerebral perfusion. This involves ?
|
administering osmotic diuretics (sometimes corticosteroids), restricting fluids, draining CSF, hyperventilating (with caution), controlling fever, and/or reducing cellular metabolic demands.
|
|
|
The five main steps in a comprehensive neurological examination are
CCMSR (CHECK and C if MY SENSORYS are RIGHT) |
assessment of cerebral function
assessment of cranial nerve function assessment of the motor system assessment of the sensory system assessment of reflexes. |
|
|
An X-ray of cerebral circulation taken after a contrast agent has been injected into a selected artery.
|
cerebral angiogram
|
|
|
Grafting tissue harvested from a donor.
|
allograft:
|
|
|
Grafting tissue harvested from the patient.
|
autograft:
|
|
|
A complication that occurs when bone loses its blood supply and dies; treatment may entail bone grafts, prosthetic replacement, or joint fusion.
|
avascular necrosis of bone:
|
|
|
Inflammation of the iris and ciliary body.
|
iridocyclitis:
|
|
|
Serum concentration of uric acid greater than 7mg/dL.
|
hyperuricemia:
|
|
|
Increased forward curvature of the thoracic spine.
|
kyphosis:
|
|
|
Also known as osteochondritis deformans juvenilis; a self-limiting disorder in which there is aseptic necrosis of the femoral head. Affects children between the ages of three and twelve.
|
Legg-Calvé-Perthes disease:
4 stages Avascular-Femoral head becomes more dense with possible fracture of supporting bone Fragmentation or Revascularization-Fragmentation and reabsorption of bone Reparative-Reossification when new bone has regrown Regernerative-Healing, when new bone reshapes |
|
|
Accumulations of sodium urate crystals.
|
tophi
|
|
|
Muscle contraction in which the length of the muscles remains constant, but the force generated by the muscles increases with no joint movement.
|
isometric contraction:
|
|
|
Muscle contraction characterized by shortening of the muscles with no increase in muscle tension and with joint movement.
|
isotonic contraction:
|
|
|
Isolation procedures are generally discussed in terms of what two tiers?
|
Standard precautions and transmission-based precautions
|
|
|
Nursing care for a patient with a stage 1 pressure ulcer should take into account that the ulcer
|
will heal once pressure is removed
|
|
|
Frostbite is a form of thermal tissue trauma. The nurse should know which of the following about immediate treatment of frostbite?
|
Rewarming should be done in a warm tub of water
|
|
|
In preoperative teaching for the geriatric patient, the nurse should consider
|
that older adults continue to function and understand.
|
|
|
A client with multiple sclerosis experiences nocturnal urinary incontinence. Which of the following interventions is most appropriate in this situation?
|
Encourage the client to wear incontinence pads.
|
|
|
A patient with myasthenia gravis is experiencing a myasthenic crisis. The nurse will expect which of the following to happen after the patient receives a dose of Tensilon IV?
|
Muscle weakness will get better.
|
|
|
Which of the following contributes to a cholinergic crisis in a patient with myasthenia gravis?
|
Too much anticholinesterase medicine
|
|
|
Osteoporosis, a metabolic bone disorder, is characterized by
|
bone loss and deformity
|
|
|
Older adults have an increased incidence of infections and diseases such as cancer. What is the most significant factor related to this increased mortality and morbidity?
|
Decreased production of white blood cells
|
|
|
A patient with hepatitis B is admitted to the nursing unit. The nurse knows that
|
one portal of entry is by needlestick.
|
|
|
A patient is admitted to the nursing unit with mononucleosis. The nurse knows that
|
the virus is transmitted by airborne droplets.
|
|
|
In the case of an accidental fall with profuse bleeding of the leg, the first action that should be taken is to
|
apply direct pressure to the bleeding area.
|
|
|
A five-year-old child has been diagnosed with juvenile rheumatoid arthritis, and the parents are very concerned about whether the child will be able to play and progress in school. The nurse can assist the family by discussing exercise plans. Which of the following would benefit the child?
|
Encourage normal play and range-of-motion exercises when joints are not inflamed.
|
|
|
When a patient is confined to bed rest, problems of immobility may develop. One problem associated with immobility is
|
contractures
|
|
|
Mr. Adams has just had surgery for hip joint replacement. He is at risk for joint displacement due to his existing conditions, which include diabetes mellitus, hypertension, and obesity. The nurse should be concerned if he complains of
|
abnormal motion (external or internal rotation of the joint).
|
|
|
Tissue trauma produces an inflammatory reaction in the body regardless of the cause. All but which of the following are associated with the inflammatory response?
A. A chemotactic gradient is formed. B. Blood vessels remain constricted. C. Protein-rich exudates enter the injured area. D. White blood cells enter the injured area. |
B. Blood vessels remain constricted.
|
|
|
Stage 1 pressure ulcers may be assessed by which of the following parameters?
|
Warmth, edema, and hardness
|
|
|
A temperature elevation in the first twenty-four hours after surgery probably indicates which of the following:
|
Atelectasis
|
|
|
A patient who had abdominal surgery three days ago and has been receiving opioids for pain control (fifty milligrams of Demerol every four hours) is complaining of a distended abdomen and cramping gas pains. Her bowel sounds are hypoactive. The most immediate nursing action would be to
|
assist the patient to ambulate in the hall.
|
|
|
When caring for a patient with deep vein thrombosis who suddenly complains of chest pain, the nurse should do which of the following?
|
Elevate the head of the bed and call the physician.
|
|
|
Metabolic acidosis is characterized by
|
a low pH of less than 7.4 and a low plasma bicarbonate.
|
|
|
Which of the following topics would be a priority in teaching a patient who takes immunosuppression drugs for the management of multiple sclerosis?
|
Stress management techniques
|
|
|
The nurse should recognize that an early clinical sign of multiple sclerosis is
|
weakness of the legs
|
|
|
The most important nursing responsibility associated with administration of myasthenia gravis medications is
|
giving the drugs on time and before activities.
|
|
|
A client with myasthenia gravis has a very weak cough and impaired swallowing. To prevent respiratory complications, which nursing intervention is most appropriate?
|
Assist the patient to a sitting position with head upright while eating.
|
|
|
A patient has been discharged from the emergency department after being hit in the head with a baseball. The patient has a headache and no memory of the accident. There are no other neurological deficits. The nurse should instruct the patient and family to
|
come back immediately if the patient cannot be awakened.
|
|
|
As part of the neurological exam for a patient who is unconscious, the nurse tests the patient’s gag and swallow reflex to assess
|
cranial nerves IX and X (glossopharyngeal and vagus).
|
|
|
After two weeks in a rehabilitation unit, a patient with a T10 spinal cord injury becomes verbally abusive to the staff and demands to be transferred to a place where the staff knows what it is doing. The nurse should respond by
|
accepting the client’s anger and asking for input into his plan of care.
|
|
|
A nurse can best assist a patient with a chronic neurological problem by
|
assisting the patient toward independence.
|
|
|
The family members of a patient with tuberculosis need
|
treatment with Isoniazid as a precaution.
|
|
|
Passive immunity can be achieved through
|
immunizations.
|
|
|
If a preteen girl or boy begins to limp and experience pain, the child should be referred to a physician for possible diagnosis of hip problems. The nurse should be aware of common complaints that warrant referral or treatment. Which of the following sets of problems require referral?
|
A limp and pain upon rising in the morning
|
|
|
Mr. Smith, an overweight seventy-five-year-old, complains of intense pain in his big toe. He is diagnosed with gout and placed on Colchine. The nurse knows that part of patient teaching includes
|
taking prescribed medication until pain subsides or GI symptoms begin.
|
|
|
__________________ is a neuromuscular disorder characterized by variable weakness of voluntary muscles, which often improves with rest and worsens with activity. The condition is caused by an abnormal immune response.
|
Myasthenia gravis
|
|
|
A Pt taking Gantrisin (sulfisoxazole) may need to do what?
|
Increase water intake up to 3,000-4,000 cc a day to prevent crystalluria
|
|
|
Initial signs of Shigella are?
|
fever, cramping and abominal pain
|
|
|
Initial signs of Norwalk virus? (no walking if im not hungry and tired)
|
Anorexia and Malaise
|
|
|
Initial signs of Salmonella?
|
N/V
|
|
|
Initial signs of Mono?
|
HA and Fatigue
|
|
|
Pneumocystis (carinii) a PT with AIDS would present with
|
non-productive cough
dyspnea fever |
|
|
How does HSV-type 2 survive in the body?
|
it invades nerve ganglia when its replication diminishes.
|
|
|
Which health problem precedes Rheumatic Fever?
|
streptococcal pharyngitis
|
|
|
Which clinical manifestation is most indicative Lymes disease in children?
|
ring shaped rash at site of the bite
|
|
|
Which observation indicates a UTI in school aged children?
|
enuresis (bedwetting)
|
|
|
Which food is most likely the cause of Salmonella in a child?
1)hotdogs 2)cookie dough 3)tuna fish 4)milk shake |
Cookie dough consit of raw eggs,
|
|
|
A positive response wo that test is the best indicator that a patient with HIV has TB?
|
sputum specimen;
it is common for immunosuprresed patients to test positive to TB skin test. pleural needle bio is too invasive |
|
|
Which vaccine is contraindicated in a child who is HIV positive?
|
Rubella; which contains live attentuated viruses
|
|
|
A precense of a diseased bone would make a pt more prone to what type of fracture?
|
pathological fx
|
|
|
which lab test results indicate positive diagnosis of SLE.
|
positive antinuclear antibodies
|
|
|
spiral fx of the humerus in a child may be indicative of?
|
abuse
|
|
|
most common fx in children
|
oblique fx
|
|
|
pt on prophylactic probencid-cholchicine regimen should be advised to ________________,?
|
drink 8-10 glasses of water a day, to flush out the uric acid that is excreted due to the medication.
|
|
|
visual interpretation resides in what part of the brain?
|
Occipital
|
|
|
Position sense resides in what part of the brain?
|
Cerebellum
|
|
|
judegment, personality and inhibitions reside in what part of the brain?
|
frontal lobe
|
|
|
position of a pt in the acutr stage of a CVA?
|
lateral with head elevated
|
|
|
How is the dx of Myathenia Gravis confirmed?
|
Tensolin test
|
|
|
sensory information and spatial orientation resides in what part of the brain?
|
parietal
|
|
|
hearing resides in what part of the brain?
|
temporal
|
|
|
complication of inhaled disflurane?
|
dysrhythmias
|
|
|
Pain associated woth duodenal ulcer?
|
epigastric pain 1-2 hours after food ingestion
|
|
|
Black stool in a burn pt is indicitive of?
|
the development of Curlings Ulcer;an acute peptic ulcer of the duodenum resulting as a complication from severe burns
|
|
|
What is a clinical manifestation of rubella (German measels)in the prodromal stage?
|
mild conjuncivitis
|
|
|
What is a clinical manifestation of the mumps in the prodromal stage?
|
ear ache
|
|
|
What is a clinical manifestation of chicken pox in the prodromal stage?
|
papules
|
|
|
What is a clinical manifestation of scarlet fever in the prodromal stage?
|
abdominal pain`
|
|
|
Symptoms of RSV are?
|
URI
Mild fever Resp distress w/tachypnea paroxysmal cough wheezing moments of apnea |
|
|
What clinical manifestation is most indicitive of UTI?
|
Frequency
|
|
|
Which health problem may manifest if step pharyngitis goes untreated?
|
glomerulonephritis
|
|
|
A child exhibits white tongue, red papillea, diffuse rash under folds of the joints, what illness would you expect?
|
scarlet fever
|
|
|
An elevated ESR (erythrocyte sedimentation rate) is typical in patients with?
|
inflammatory connective tissue disease and inlammation casued by an infection
|
|
|
What should a nurse do to assess the prescence of pain in a patient with carpal tunnel syndrome?
|
tap lightly over the medial nerve (Tinles Sign)
|
|
|
What complication is associated with Pagets disease of the bone?
|
pathological fracture
|
|
|
is a medical term for a type of partial blindness resulting in a loss of vision in the same visual field of both eyes.
|
Homonymous hemianopsia, or homonymous hemianopia,
|
|
|
Clinets reciving dopamine need continuous __________ monitoring for?
|
Heart; dysrhythmias
|
|
|
What nursing intervention is priority in a post surgical pt who has not regained conciousness, who recived general anesthesia?
|
keep bed flat will limit orthostatic hypotension, maintain integrity of the surgical site and any tubes
|

