![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
1.To be able to explain and describe the hypothalamic-pituitary portal system. what controls both the anterior and posterior pituitary and how? deakin post box with ants in it |
hypothalamus controls both the anterior and posterior pituitary via secretion of hormones |
deakin post box with ants in it is controlled by hypo thal by secreting ant kill inside it |
|
|
what do the neurons in hypothalamus do and what is the effect on the anterior pituitary gland? |
neurons in hypothalamus release regulatory factors carried by hypothalamic pituitary portal system(HPPS) to the anterior pituitary gland where they control the release of anterior pituitary hormones |
|
|
|
where are posterior pituitary homrones made and where are they transported to?
deakin mail |
Posterior pituitary hormones are synthesized in cell bodies of the supraopticand paraventricular neurons in the hypothalamus, and then transported down axonal pathways to terminals in the posterior pituitary gland. |
deakin post mail is made at home and transported to the post |
|
|
where are posterior pituitary hormones stored and released? where deakin mail is stopred and released to |
posterior pituitary hormones are stored in the posterior pituitary gland, from which they are released into the systemic circulation. |
deakin mail is stored in post box and released to public |
|
|
2.To be able to explain and describe the hypothalamic-pituitary growth hormone axis. what is not always a 1:1 ratio? deakin cafateria |
theres a number of hypothalamic releasing and inhibiting factors, which are not always 1:1 ratio |
egg and a yolk at deakin cafateria |
|
|
what controls release of growth hormone but also inhibits release of TSH and prolactin? |
e.g. Somatostatin primarily controls release of growth hormone, but it can also inhibit release of thyroid stimulating hormone (TSH) and prolactin. |
|
|
|
what stimulates release of TSH but also causes release of prolactin? |
Additionally, thyrotropin-releasing hormone (TRH) stimulates the release of TSH, but it can also cause release of prolactin. |
|
|
|
all known hypothalamic releasing factors are peptides with exeption of what hormone? Which hormones are proteins and glycoproteins? |
With the exception of dopamine all known hypothalamic releasing factors (HRFs) are peptides. The anterior pituitary hormones are proteins and glycoproteins. |
|
|
|
what are the three groups of hormones? sun over deakin, shoe in deakin lolly book shop, tree in front of deakin river |
"there are three groups of hormones: (i) omatotrophic hormones: growth hormone (GH), prolactin. (ii) Glycoproteins hormones: luteinizing hormone (LH), follicle-stimulating hormone (FSH), and thyroid stimulating hormone (TSH). (iii) adrenocorticotropin (ACTH). Separate class on its own." |
omatotrophic homrones causes sun to grows like a breast over deakin. Glycoprotein hormones in a shoe like a sugar lollypop have a little(LH) fish (FSH) thigh(TSH) leg inside it in candy shop at uni. Adrenocorticotropin on a tree near river outside ij building are like monkeys that are a separate class to ground animals |
|
|
how must peptide therapy occur and why? asparin at deakin medical centre |
"Peptides (hormones) are subject to peptidase degradation so therapy must occur by IV, notorally." |
asparin at deakin medical centre |
|
|
what do HRF bind to and where and what does it result in? hands bind to deakins café fridge in book shop before camping |
HRF's (hypothalamic releasing factors aka peptides) bind to G-proteins in the anterior pituitary cell type causing increased intracellular Ca2+ & cAMP levels. |
hands binding on deakins café fridge handle) G protein) before camping to get milk out(Ca2+) |
|
|
how are most HFR;s released? deakin fridge handles |
Most HRFs are released in a cyclic or pulsatile, rather than continuous manner. |
most deakin fridges are cyclic in shape or with little knobs on it rather thana continueous handle |
|
|
what kind of feedback controls the hormones? dusa controls food allowance |
negative feedback tightly controls the release of hormones |
dusa tighyl controls the food allowance |
|
|
what negatively regulates the pituitary and hypothalamus to maintain equilibrium level of hormone release? |
systemic hormones produced by target organs negatively regulate the pituitary and hypothalamus to maintain an equilibrium level of hormone release |
|
|
|
what is primary endocrine disorder caused by? |
A primary endocrine disorder is caused by target organ pathology |
|
|
|
what does a secondary disorder reflect? |
a secondary disorder reflects pituitary disease |
|
|
|
what does a tertiary endocrine disorder result from? |
a tertiary endocrine disorder results from hypothalamic pathology |
|
|
|
what do stimulatory hypothalamic factos stimulate? |
Stimulatory hypothalamic factors (corticotroph/CRH in this case) stimulate the release of pituitary hormones (Adrebicorticotropin/ACTH in this case). |
|
|
|
what happens to the target organ in response to pituitart hormone? |
In response to pituitary hormone signals, the target organ (the adrenal gland in this case) produces a hormone (cortisol in this case). |
|
|
|
in addition to its systemic physiologic actions, what does cortisol do? |
In addition to its systemic physiologic actions (not shown), cortisol negatively regulates the hypothalamic-pituitary–adrenal axis by inhibiting CRH and ACTH. |
|
|
|
what also negatively regulates CRH, what does it provide? |
ACTH also negatively regulates CRH, providing more sensitive control of the axis. |
|
|
|
what does the hypothalamic-pituitary–growth hormone axis (HPGHA) regulate? |
hypothalamic-pituitary–growth hormone axis (HPGHA), regulates general processes that promote growth. |
|
|
|
when is GH first expressed at high levels? |
GH is first expressed (secreted) at high levels during puberty. |
|
|
|
how is GH secreted, and when? |
GH is secreted in Pulses and occur at night/sleep. |
|
|
|
most anabolioc effects are mediated by? how is this certain hormone released and expressed? |
Most anabolic effects are mediated by Insulin-like Growth Factor 1 (IGF-1). Released by the liver in response to GH. Stable and expressed for long periods so IGF-1 is a better measure of acromegaly. |
|
|
|
what regulate GH? |
Exogenous factors regulate GH. Environmental factors, exercise, & nutrition. |
|
|
|
what acts with GH to promote GH release? |
Endogenous factors sex steroids, dopamine, ghrelin, somatostatin (acts with GH to promote GH release). |
|
|
|
how is Ghrelin expressed during what periods of time? ghremlin fasting |
"Ghrelin expressed by gastric fundal cells during periods of fasting.(targeted by mimics for appetite control)." |
grhemlin fasting during christmas |
|
|
what does pegvisomathas do? |
Pegvisomanthas high IGF-1 reducing potential, but also increases GH levels by reducing IGF-1 mediated feedback inhibition. |
|
|
|
3.To be able to explain and describe the hypothalamic-pituitary prolactin axis. what do the lactotrophs of the anterior pituitary gland produce? |
Lactotrophs of the anterior pituitary gland produce and secrete prolactin. |
|
|
|
what is secretion of prolactin inhibited by? |
Secretion of prolactin by anterior pituitary gland lactotrophsis tonically inhibited by hypothalamic dopamine. |
|
|
|
what is Hypothalamic TRH and circulating estrogens do to prolactin release? |
Hypothalamic TRH and circulating estrogens stimulate prolactin release. |
|
|
|
what do stimulatory and inhibitory inputs on lactotrphs result in? |
These stimulatory and inhibitory inputs on lactotrophs result in a baseline equilibrium of prolactin production. |
|
|
|
what does distruption of the equilibrium result in? |
Disruption of this equilibrium results in an imbalance of prolactin production; for example, interruption of the pituitary stalk diminishes hypothalamic dopamine delivery to lactotrophs, resulting in elevated prolactin secretion. |
|
|
|
what is a disease condition that interrupts the hypothalamic pituitary portal system? |
A disease condition that interrupts the hypothalamic-pituitary portal system results in decrease secretion of most anterior pituitary gland hormones but causes increased prolactin release. |
|
|
|
what is observed in people taking antipsychotics? |
In patients taking antipsychotics elevations of prolactin are observed. |
|
|
|
what does increased prolactin levels do to estrogen synthesis, how? |
Increased prolactin levels suppress estrogen synthesis by antagonizing hypothalamus release of GnRHand by decreasing gonadotrophsensitivity to GnRH. |
|
|
|
To be able to explain and describe the hypothalamic-pituitary Thyroid axis. |
The hypothalamus secretes TRH, which promotes secretion of thyroid stimulating hormone (TSH). |
|
|
|
4. To be able to explain and describe the hypothalamic-pituitary adrenal axis. how is thyroptin used for thyroid cancer? |
Recombinant TSH (thyrotropin) is used during radioactive iodine treatment of thyroid cancer. |
|
|
|
where does the adrenal axis have neurons from? |
Adrenal Axis have Neurons from the paraventricularnucleus of the hypothalamus secrete corticotropin-releasing hormone (CRH). |
|
|
|
what does th adrenal axis stimulate release of? what does that do? |
Adrenal Axis Stimulates release of ACTH, which stimulates release of gluccocorticoids, androgens, and mineralocorticoids |
|
|
|
5. To be able to explain and describe the hypothamalic-pituitary gonadal axis. |
Gonadotrophsare unique among anterior pituitary gland cells because they secrete two glycoporteinshormones-LH and FSH. (gonadotrophins) |
|
|
|
where is GnRH secreted? what is the effect of that? |
Gonadotropin-releasing hormone (GnRH) is secreted by the hypothalamus in a pulsatile fashion, stimulating gonadotrophcells of the anterior pituitary gland to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH). |
|
|
|
what do LH and FSH stimulate? what does it produce?
|
LH and FSH stimulate the ovaries or testes to produce the sex hormones estrogen or testosterone, respectively, which inhibit further release of LH and FSH. |
|
|
|
Paradoxically, however, the increasing estrogen levels that are secreted from developing follicles during the follicular phase of the menstrual cycle induce what? |
Paradoxically, however, the increasing estrogen levels that are secreted from developing follicles during the follicular phase of the menstrual cycle induce a positive-feedback, mid-cycle ovulatory surge of LH and FSH secretion. |
|
|
|
ihibin is also produced from gonads in response to what? what does it exert? |
Inhibin is also produced by the gonads in response to FSH and exerts negative feedback on gonadotrophs to inhibit further release of FSH. |
|
|
|
how does locally produced pituitary activin act? Exogenous pulsatile GnRHcan be used how? |
Locally produced pituitary activin acts in a paracrine fashion to stimulate FSH secretion. Exogenous pulsatile GnRHcan be used to induce ovulation in women with infertility of hypothalamic origin. |
|
|
|
6.To be able to explain and describe the role of ADH in mediating vascular volume. |
In contrast to many hormones to the anterior pituitary gland, the posterior lobe of the pituitary gland (neurohpophysis) secretes only two hormones: antidiuretic hormone (ADH), and oxytocin. |
|
|
|
what does ADH regulate? |
ADH: regulates plasma volume and osmolarity. |
|
|
|
7.To be able to explain and describe the pharmacology of the thyroid gland. where is oxytocins secreted from? what is it regulated by? |
Oxytocinis secreted from the posterior pituitary (neurohypophysis) and is regulated by the paraventricularnuclei of the hypothalamus |
|
|
|
One of the target tissues for oxytocin is? |
One of the target tissues for oxytocin is the myometrium of the uterus (smooth muscle). |
|
|
|
When the fetus of a pregnant female starts to exert enough pressure on the cervix this will stimulate mechanoreceptors (pressure receptors) to start doing what? |
When the fetus of a pregnant female starts to exert enough pressure on the cervix this will stimulate mechanoreceptors (pressure receptors) to start generating action potentials to the brain (hypothalamus). |
|
|
|
what will this, generation of action potentials to the brain stimulate? |
Then this will stimulate the secretion of oxytocin |
|
|
|
When oxytocin interacts with its receptors on within the uterus this will stimulate the muscle tissue to? what is the effect on the fetus? |
When oxytocin interacts with its receptors on within the uterus this will stimulate the muscle tissue to contract; forcing the fetus to push even harder against the cervix. |
|
|
|
what happens when more pressure is applioed to the cervis? |
As more pressure is applied to the cervix more action potentials are generated to the brain, which will increase oxytocin levels until the fetus is completely birthed/expelled from the mother |
|
|
|
where is thyroglobulin synthesised? what pathway does it follow? why? by what method? |
Thyroglobulin is synthesized in the rough endoplasmic reticulum and follows the secretory pathway to enter the colloid in the lumen of the thyroid follicle by exocytosis |
|
|
|
what is iodide oxideised to in the colloid? by what enzyme? |
-In the colloid, iodide (I-) is oxidized to iodine (I0) by an enzyme called thyroid peroxidase. |
|
|
|
a) Explain the effects of thyroid hormones on target tissues. how is thyroid hormone synthesised? |
Thyroid hormones are synthesized from two derivatizedtyrosine molecules that are attached by an ether linkage. |
|
|
|
Thyroid Hormone Receptor Actions what happens in the absence of the thyroid hormone? what about in the presence of it? |
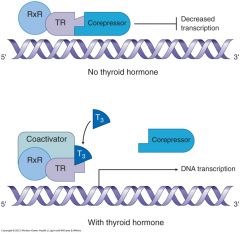
In the absence of thyroid hormone, the thyroid hormone receptor (TR): retinoid X receptor (RXR) heterodimer associates with a corepressorcomplex, which binds to promoter regions of DNA and inhibits gene expression. In the presence of thyroid hormone (T3), the corepressorcomplex dissociates from the TR:RXR heterodimer, coactivatorsare recruited, and gene transcription occurs. This example demonstrates the action of T3 on a TR:RXR heterodimer, but similar mechanisms are probable for TR:TR homodimers |
|
|
|
b) Hypothalamic pituitary thyroid axis. describe the axis |

normal axis, graves disease (stimulatory autoantibody) and hashimoto's thyroiditis (Destructive autoantibody) |
|
|
|
c) Treatment of hypothyroidism |
Levothyroxine (L-T4) is acceptable therapy for most patients. T3 may also be used to treat hypothyroidism. |
|
|
|
d) Treatment of hyperthyroidism. |
In thyrotoxicosis, the catecholamine receptor number is increased, so beta blockers have an important role in blocking catecholamine response. If tolerated, propranolol should be used (usually 40-120 mg in two or three daily doses) because it blocks conversion of T4 to T3. Atenolol can also be used (25-50 mg once a day).In severe thyroiditis, anti-inflammatory agents (NSAIDs, corticosteroids) may be necessary. |
|

