![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
327 Cards in this Set
- Front
- Back
|
Under normal conditions, fertilization occurs in which part of the female reproductive tract?
|
Ampulla of the uterine/fallopian tube
|
|
|
Benign hyperplasia (excessive growth of cells) of which part of the male reproductive system would be most likely to interfere with the passage of urine?
|
Prostate (periurethral zone)
|
|
|
Which pair of structures does NOT differentiate from comparable embryonic structures in the male and female?
a. Bulb of corpus spongeosum and vestibular bulb b.Shaft of penis and labia majora c. Glans of penis and glans of clitoris d. Crus of corpus cavernosum penis and crus of corpus cavernosum clitoris |
b. shaft of the penis and the labia majora
The shaft of the penis is analogous to the shaft of the clitoris whereas the labia majora is analagous to the scrotum |
|
|
Which structure is found only in males?
a. Anterior recess of ischoianal fossa b. Genital Hiatus c. Ischiocavernosus muscle d. Rectovesical pouch e. Sphincter urethrae muscle |
d. rectovesicular pouch is the space between the rectum and the bladder. Females cannot have this since the uterus lies between the rectum and the bladder.
|
|
|
Which of the following is considered a part of the broad ligament?
a. Mesovarium b. Ovarian ligament c. Round ligament of the uterus d. Suspensory Ligament of the ovary |
a. mesovarium
The msovarium, mesometrium and mesosalpinx make up the braod ligament |
|
|
Which of the following does not conduct spermatozoa?
a. Ampulla of the ductus deferens b. Duct of the seminal vesicle c. Epididymis d. Prostatic Urethra |
b. Duct of the seminal vessicle carries seminal fluid (fructose)
|
|
|
A 27-year-old woman is examined by her gynecologist. Upon rectal examination, a firm structure, directly in front of the rectum in the midline, is palpated through the anterior wall of the rectum. This structure is the:
|
cervix of the uterus (directly anterior to the rectum)
|
|
|
The most inferior extent of the peritoneal cavity in the female is the:
|
rectouterine pouch
|
|
|
Structures within the lower gastrointestinal tract specialized for physical support of fecal material are the:
|
transverse rectal folds
|
|
|
During a hysterectomy, the uterine vessels are ligated. However, the patient's uterus continues to bleed. The most likely source of blood still supplying the uterus is from which artery?
|
Ovarian a. anastamoses with the uterine a.
|
|
|
During a hysterectomy, care must be taken in ligation of the uterine vessels because they cross the _________ superiorly.
|
ureter
|
|
|
The part of the broad ligament giving attachment and support to the uterine tube is the:
|
mesosalpinx
|
|
|
The male pelvis tends to differ from the female pelvis in that the male pelvis often has a:
a. larger pelvic inlet b. smaller subpubic angle c. straighter sacral curvature d. larger pelvic outlet |
b. smaller subpubic angle
|
|
|
In a CT scan of the pelvis, where is the uterus loacted in relation to the bladder and rectum?
|
Posterior to the bladder and anterior to the rectum
|
|
|
urethra
|

Identify the structure at the tip of the arrow
|
|
|
cervix
|
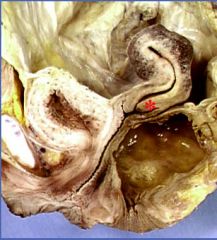
Idenify the structure marked by the asterix
|
|
|
anal triangle
|
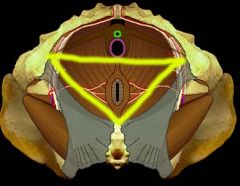
The yellow line forms the border of what strucutre?
|
|
|
vesicouterine pouch
|
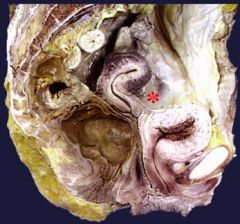
The asterisk lies in what structure?
|
|
|
What three muscles form the levator ani?
|
puborectalis
pubococcygeus ileococcygeus |
|
|
Which male and female structures, respectively, travel through the urogenital hiatus?
|
male: urethra
female: urethra and vagina |
|
|
Why does testicular cancer rarely spread to the inguinal region?
|
because the testicular artery, branches off near the renal arteries (vs the uterine and ovarian arteries that branch off the iliac)
|
|
|
From where do primordial germ cells originate?
|
yolk sac
|
|
|
The primordial gonad consists of a cortex and medulla. Which part of the primordial gonad forms the male and female gonads, respectively?
|
Testes - medulla
Ovaries - cortex |
|
|
What is the function of the rete testes?
|
to drain the seminiferus tubules and flow the contents to the efferent ductules
|
|
|
What is the term for the first cells on the pathway to become mature sperm? Oocytes?
|
Spermatagonia
Oogonia |
|
|
What androgen is responsible for the degeneration of mullerian ducts in males?
|
Antimullerian hormone (Mullerian Inhibitory Factor)
|
|
|
What is the function of testosterone and DHT in male sexual development?
|
masculinization of the external genetalia
|
|
|
Which embryologic structure will eventually form the channels whereby sperm exits the testes?
|
mesonephric ducts
|
|
|
Trace the development (proximal to distal) of the male reproductive channels formed from the mesonephric duct.
|
epidiymis (most proximal), vas deferens, seminal vesicle, ejactulatory duct
|
|
|
From which other structure does the prostate gland develop?
|
prostatic urethra
|
|
|
Trace the development (cranial to caudal) of the femal reproductive structures formed from the mullerian ducts.
|
fallopian tubes with fimbria (cranial), fundus and body of the uterus from the fusion of L&R tubes, upper 1/3 of vagina
|
|
|
T/F: Normal male development requires the testes, but development of fallopian tubes and uterus does not require the ovaries.
|
True
|
|
|
AMH is secreted by which cells of the testes?
|
Sertoli
|
|
|
Testosterone is secreted by which cells of the testes?
|
Leydig
|
|
|
For the follwoing embryologic structure name the male and female reproductive structures that are derived from it: genital tubercle
|
Male: glans penis
Female: clitoris |
|
|
For the follwoing embryologic structure name the male and female reproductive structures that are derived from it: urogenital folds
|
male: ventral penis
female: labia minora |
|
|
For the follwoing embryologic structure name the male and female reproductive structures that are derived from it: genital swellings
|
male: scrotum
female: labia majora |
|
|
What type of receptors are androgen receptors?
|
nuclear
|
|
|
What does the SRY gene produce upon translation?
|
TDF - testis determining factor
|
|
|
The development of which mesonephric structures are determined by testosterone?
|
epididymis, vas deferens and seminal vesicle
|
|
|
The development of which mesonephric structures are determined by dihydrotestosterone?
|
prostate and penis/scrotum
|
|
|
What is a gonadal streak?
|
elongate structure in the ususal site of the ovary; dx of one of the syndromes of dysgenesis and indication that both X chromasomes are needed for normal development of ovary
|
|
|
If one gonad was a streak and the other was a testis what would the internal genitalia look like?
|
There would be a hemiuterus on the same side of the streak (remember: the effects of testicular products is ipsilateral)
|
|
|
What is the difference between gonadal dysgenesis and hermaphroditism?
|
Gonadal dysgenesis is maldevelopment in which one or both glands are streaks; Hermaphroditism is maldevelopment in which gonads have male/female/both gonadal tissue and there is ambiguous internal/external genitalia
|
|
|
What is the most common genotype of a pt with Turner Syndrome?
|
45XO
|
|
|
A 12-year-old girl of short stature comes to your office. You note that she is hypertensive in her upper extremities and hypotenisve in her lower extermities. What is your next dx procedure?
|
Karyotyping; girls with Turner Syndrome are often short statured and may have a coarcted aorta producing the sx your pt is experiencing
|
|
|
What is the genotype of a pt with mixed gonadal dysgenesis?
|
45X/46XY
|
|
|
If a person has both testicular and ovarian tissue, that person is a _________.
|
True hermaphrodite
|
|
|
Testicular Feminization Syndrome is an androgen insensitivity syndrome where a phenotypically normal female has testes and high levels of testosterone. What is the pathophys of this syndrome?
|
hyperplasia of the Leydig cells and defective or absent androgen carrier proteins and/or androgen receptors
|
|
|
What is the phenotypic fate of a newborn with 47XXX?
|
compatible with normal femal phenotype, including fertility
|
|
|
47XXY is also called:
|
Klinefelter Syndrome; tall, feminine features, atrophic testes (infertility)
|
|
|
Which sex is the default pathway for reproductive development?
|
female
|
|
|
What is the significance of the SRY gene's location on the p segment of the Y chromosome?
|
it is in an area highly susceptible to recombination; can have XX with phenotypically male traits or mosaicism (hermaphroditism)
|
|
|
Which cells make testosterone?
|
Leydig cell
|
|
|
What happens developmently in males in the absence of testosterone?
|
wolfian ducts involute
|
|
|
In males and females, respectively, which cells constitute the interstitial cells?
|
Leydig and Theca cells
|
|
|
Leydig and Theca cells produce which type of hormones?
|
androgens
|
|
|
Gametogenic cells (Sertoli and Granulosa) secrete which hormones of the hypothalamic-pituitary-gonadal axis?
|
inhibin and estrogens(from testosterone)
|
|
|
What is the effect of pulsatile secretion of GnRH? Constant secretion?
|
Pulsatile: stimulates receptors and increased LH and FSH
Constant: inhibits receptors and gives chemically induced menopause |
|
|
Which gonadal cells are receptive to LH?
|
Leydig and Theca cells (the other one's the other one)
|
|
|
Describe the two cell model of sex steroid synthesis in female cells
|
Theca cells take in LH --> upregulates LDL receptors to take in cholesterol --> makes androsteindione (granulosa cells cannot make androstenedione because they lack 17 a-hydroxylatase)
Andosteindione must go to granulosa cell (theca lacks aromatase) to produce testosterone/estradiol |
|
|
What is the regulated variable in the inhibin system?
|
FSH
|
|
|
What is usually the first sign of Kallmann's Syndrome?
|
Anosmia (lack of sense of smell); GnRH can't migrate from olfactory system
|
|
|
What is the treatment for uterine leiomyoma?
|
Constant infusion of GnRH to shrink the tumor for resection (also with prostatic hyperplasia)
|
|
|
Which forms of inhibin are found in the plasma in women?
|
Inhibin B and A (only B in men:B for Boys)
|
|
|
Outline the pattern of GnRH release from the hypothalamus from birth through puberty.
|
rise in GnRH for first 6 months, then sudden drop; stays low for about 8 years, then rises through early puberty to reach adult levels
|
|
|
What is the first sign of pubertal onset in girls? Boys?
|
Breast buds; testicular enlargement > 3ml
|
|
|
What is the most common cause of delayed puberty?
|
Constitutional delay of growth and puberty
|
|
|
What are the congenital causes of hypOgonadotropic hypogonadism seen in delayed puberty?
|
GnRH deficiency, Kallman's syndrome, Congenital hypopit, midline CNS defects, Prader-Willi
|
|
|
What things can cause functional hypogonadotropic hypogonadism, resulting in delayed puberty?
|
chronic illness, malnutrition, stress, excessive exercise/anorexia, hyperPRL, hypothyroidism
|
|
|
What are the acquired causes of hypogonadotropic hypogonadism seen in delayed puberty?
|
Pit or Hypothalamus tumor or trauma, CNS infection, irradiation, Hemochromatosis, AI hypophysitis
|
|
|
What accounts for compromised final height in a child with precocious puberty?
|
increased estrogens -> bone age advancement -> premature sealing of epiphyseal plates in long bones
|
|
|
What series of events occur in male pubertal development?
|
testicular enlargement -> pubic hair -> penile enlargement -> growth acceleration
|
|
|
What series of events occur in female pubertal development?
|
breast buds -> growth acceleration -> menarche (1.5-3 years after onset)
|
|
|
What defines delayed puberty in boys? Girls?
|
no testicular enlargement at 14; no breast development at 13 or no menarche at 16 or 5 yrs after onset
|
|
|
What are the acquired causes of hypERgonadotropic hypogonadism seen in delayed puberty?
|
chemotherapy, irradiation to pelvis, galactosemia, AI oophoritis, mumps orchitis, testes torsion/trauma, cpyptorchidism
|
|
|
What are the congenital causes of hypERgonadotropic hypogonadism seen in delayed puberty?
|
Klinefelter's, Turner's syndrome, gonadal dysgenesis, vanishing testes (don't blame me, I don't even know what that means), Noonan
|
|
|
What findings characterize Turner's syndrome?
|
short stature, shield chests, web neck, aortic coarctation, bicuspid aortic valve
|
|
|
Why are LH and FSH elevated in hypergonadotropic hypogonadism?
|
because gonadal failure means there is no negative feedback on pituitary gonadotropin release
|
|
|
What are congenital causes of hypergonadotropic hypogonadism ONLY IN GIRLS?
|
aromatase, 17-alpha-OHase, or 20,22-desmolase deficiency
|
|
|
How will LH and FSH levels differ in constitutional delayed puberty vs. hypogonadotropic hypogonadism?
|
in both, prepubertal levels seen
|
|
|
How is isosexual precocious puberty defined in boys? Girls?
|
testicular enlargement before 9, breast development before 8 or menses before 10
|
|
|
What commonly causes isosexual precocious puberty in girls? Boys?
|
idiopathic: CNS lesion
|
|
|
What causes peripheral precocious puberty in boys?
|
CAH, Adrenal tumor, Leydig tumor, hCG tumor, testotoxicosis, exogenous androgens
|
|
|
What causes peripheral precocious puberty in girls?
|
ovarian cysts, granulosa tumor, sertoli-leydig tumor, exogenous estrogen
|
|
|
What causes peripheral precocious puberty in both boys and girls?
|
McCune-Albright, primary hypothyroidism
|
|
|
What is the classic triad of McCune-Albright?
|
precocious puberty, polyostotic fibrous dysplasia, café-au-lait spots
|
|
|
What is premature thelarche?
|
normal variant, isolated breast dvlpmt in girls <2, spontaneous regression
|
|
|
What is premature adenarche?
|
normal variant, pubic/axiallary hair in girls <8 or boys<9; premature activation of DHEA-S synthesis, natural pubertal course follows
|
|
|
Describe the drainage of mature sperm from the testes.
|
seminiferous tublules -> rete testes -> epididymis -> ductus deferens -> seminal vesicle
|
|
|
How is the blood-testis barrier formed?
|
By the tight junctions of the Sertoli cells
|
|
|
What are the three sequential phases of spermatogenesis?
|
proliferative -> meiotic -> spermiogenic
|
|
|
What type of spermatogonial cells are capable of self-renewal?
|
Ad
|
|
|
What are the four stages of spermiogenesis?
|
golgi, cap, acrosomal, maturational
|
|
|
What are the primary functions of the epididymis?
|
post-testicular maturation and storage of spermatozoa
|
|
|
What spermaozoal maturational events occur in the epididymis?
|
motility develops, spermatozoa become capable of fertilization, and capacitation
|
|
|
Why are the spermatozoa more concentrate by the time they reach the end of the epididymis?
|
Seminiferous tubule fluid is resorbed in caput
|
|
|
What happens to spermatozoa in the epididymis during sexual inactivity?
|
After only a few days, they start to lose the capability to fertilize, then motility, then vitality
|
|
|
Why is androgen-binding protein, secreted by Sertoli cells, critical to spermatogenesis?
|
Maintains high testosterone levels in seminiferous tubules
|
|
|
Where must primary spermatocytes migrate?
|
to the adluminal compartment (protected by BTB)
|
|
|
What becomes of the Wolffian duct?
|
Seminal vesicles, vas deferens, epididymis
|
|
|
Wolffian development is dependent on what factors?
|
testosterone derived from ipsilateral testis
|
|
|
What is Sertoli only syndrome and is there treatment available?
|
Complete lack of germ cells found in seminiferous tubule, no tx unless cause was toxin
|
|
|
What hormone does the Leydig cell respond to?
|
LH
|
|
|
What hormone does the Sertoli cell respond to?
|
FSH
|
|
|
What important proteins are produced by the Leydig cell?
|
SCP - streol carrier protein, transports cholesterol to mitochondria; SAP - sterol activating protein, stimulates steroidogenesis
|
|
|
Where are androgens converted to estrogen? By what enzyme?
|
sertoli cell (mostly); aromatase
|
|
|
What are the functions of Inhibin? Where is it produced?
|
neg feedback on ant. Pit (effect on FSH > LH) and growth factor for leydig cells, produced in sertoli
|
|
|
What happens when androgens bind the androgen receptor?
|
AR is a transcription factor, binds to DNA binding element, regulates target genes
|
|
|
Development of external genetalia is dependent on what factor?
|
DHT
|
|
|
What pituitary hormone dominates before puberty? After?
|
FSH > LH before, LH > FSH after
|
|
|
Describe the interactions between the HPT and GH axes.
|
GH/ IGF-1 stimulates gonadal fxn and GnRH release, Testosterone and E2 stimulate GH release
|
|
|
What symptoms are present in a boy with Kallman's?
|
Delayed puberty due to GnRH deficiency, anosmia due to failure of olfactory neurons to migrate
|
|
|
Why does hemochromatosis result in hypogonadotropic hypogonadism?
|
Iron selectively deposits in gonadotropes in the anterior pituitary
|
|
|
What is a glycoprotein tumor of the pituitary?
|
overproduces inactive gonadotropins, pt has headaches, blurred vision, hypogonadism
|
|
|
What are the options for administering androgen replacement therapy?
|
Depo form, patch, topical gel
|
|
|
What therapy can be used to induce maturation of the testis and spermatogenesis?
|
hCG mimics LH and hMG mimics FSH
|
|
|
How long does it take to recapitulate puberty with exogenous GnRH administration? How is it given?
|
18-24 months; pulsatile pump through a catheter
|
|
|
What is the dDx of someone with ED?
|
Vascular disease, diabetes (or other neurogenic cause), hormonal disturbance, psychogenic, iatrogenic
|
|
|
What drugs can contribute to symptoms of ED?
|
androgen receptor blocker: spironalactone, psychotropic meds (↑PRL), narcotics, marijuana, cocaine, cemitidine
|
|
|
What drugs can be used to treat ED?
|
PDE inhibitors (block breakdown of cGMP, maintains smooth muscle relaxation)
|
|
|
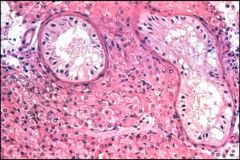
Prostate: branching glands surrounded by fibromuscular stroma
|
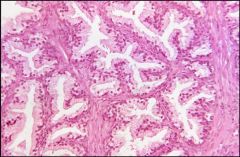
Tissue shown here is normal tissue from what organ?
|
|
|
Prostate; normal aging prostate with more fibromuscular stroma
|
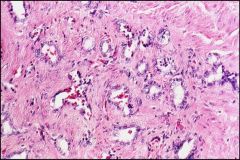
Tissue shown here is normal tissue from what organ?
|
|
|
Acute prostatitis: most commonly from E. coli or S. aureus (PMN inflammation)
|
Which organisms are most likely to cause the pathology you see here?
|
|
|
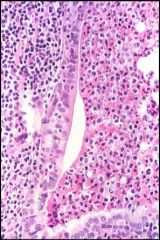
Malakoplakia: Michalis-Gutmann bodies (defective histiocytes with remnants of Gram -ive rods)
|

The dark red cell with the dark center is pathognemonic for what disease?
|
|
|
Malakoplakia: Michalis-Gutmann bodies (defective histiocytes with remnants of Gram -ive rods)
|

The dark red cell with the dark center is pathognemonic for what disease?
|
|
|
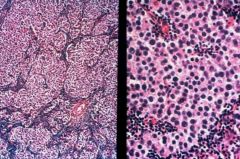
The circles are seminiferous tubules containing developing germ cells and Sertoli cells
|
What is contained inside the demarcated circles in this slide?
|
|
|
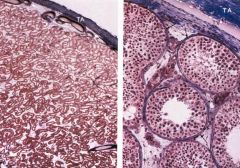
Sertoli only: no germ cells present at all.
|
What is the form of testicular atrophy shown here?
|
|
|
Klinefelter's: Leydig cell hyperplasia, sclerosing/degenerating seminiferous tubules
Presents with high FSH/LH and low testosterone |
What are the FSH/LH and testosterone levels of a pt who presents with the dz shown here?
|
|
|
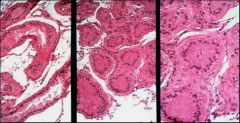
This is TB orchitis, producing caseating granulomas seen in gross path here. It differs from Syphilis in that it almost always begins in the epididymis and then spreads to the testes (opposite for syphilis)
|

What is the disease shown here? How does it differ from Syphilis?
|
|
|
Fish flesh appearance of a Seminoma (testicular tumor); you are seeing the fried egg appearance of polygonal cells surrounded by lymphocytes
|
What would you expect to see on gross appearance from this disease?
|
|
|
These are the mature differentiated cells of a variety of tissues from a teratoma in the testis. 40% of testicular tumors in infants are teratomas
|
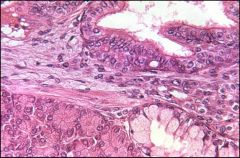
Describe the cells present in this picture
|
|
|
Choriocarcinoma (nl placental tissue shown on the left) produces hCG which can be a useful marker
|
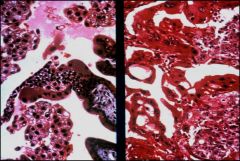
What is the useful diagnostic test for the disease shown on the right side of the picture?
|
|
|
What are the two difference between oogenesis and spermatogenesis?
|
1. The timing of meiosis I and II: spermatozoa undergoe both in 64 days, oogonia in 12-50 years
2. Meiosis produces 4 male gametes but only one female gamete |
|
|
At which phase in meiosis are female gametes arrested until the LH surge before ovulation? What are these gametes called?
|
Arrested in prophase of meiosis I; primary oocytes
|
|
|
Explain what occurs in reduction division. What are the products of reduction division?
|
Homologous chromosomes are segregated into two distinct cells each with a haploid number of duplicate DNA (2N); reduction division produces the secondary oocyte and the first polar body
|
|
|
The secondary oocyte is arrested at meiosis II, when is meiosis II completed?
|
only if fertilization occurs
|
|
|
What is the result of meiosis II prioir to arrest?
|
a secondary oocyte (23, 1N) and the second polar body
|
|
|
What are the components of the preantral and antral follicles?
|
Preantral: primoridal follicle, primary follicle, secondary follicle
Antral: tertiary and graafian follicle |
|
|
Describe the structure of a primary follicle.
|
A primary oocyte surrounded by a zona pellucida
|
|
|
What is the function of the zona pellucida?
|
a glycoprotein coat facilitating sperm attachment to and fertilization of the secondary oocyte
|
|
|
What does a secondary follicle have that a primary follicle does not?
|
a layer of cuboidal granulosa cells (FSH) and theca cells (LH) in the surrounding stroma
|
|
|
What differentiates a secondary follicle from a teritary follicle?
|
Mainly, the presence of an antrum (hence, the antral phase)--a fluid filled space within the granulosa layer
|
|
|
What is the corpus luteum and what is its function?
|
the remaining shell of hte dominant follicle once ovulation has occured; its main job is to secrete progesterone for the first 9 weeks of fetal life, until the placenta can produce it independently
|
|
|
What happens to the corpus luteum if fertilization does not occur?
|
it begins to regress about 11 days after ovulation
|
|
|
Generally, when does the LH surge occur and what causes this surge?
|
LH surge occurs at the end of the follicular phase right before ovulation. It is caused by the increase in pulsatility rate of GnRH due to a conversion of negative feedback to positive feedback by estradiol.
|
|
|
At which part of the mentrual cycle is FSH secreted preferentially over LH?
|
At the end of the luteal phase
|
|
|
Aside from being a powerful inhibitor of FSH, what other regulation mechanisms does inhibin have?
|
enhances LH stimulation of androgen synthesis in theca cells, thereby providing more substrate for estrogen synthesis in the granulosa cell.
|
|
|
Amenorrhea caused by the hypothalamus will have what relative hormone levels?
|
low LH, FSH, estrogen
|
|
|
What is the most common cause of hypothalamic amenorrhea?
|
acquired GnRH pulse generator problem from exessive exercise, eating disorders or stress
|
|
|
What are the 4 most common causes for hypothalamic amenorrhea?
|
congenital
mass effects acquired cranial irradiation |
|
|
Amenorrhea caused by the pituitary will have what relative hormone levels?
|
nl.low FSH,LH, low E
|
|
|
What are the two main causes of pituitary-derived amenorrhea?
|
prolactinoma
infiltrative: hemochromatosis |
|
|
What dopamine agonist is used for the treatment of pituitary-derived amenorrhea?
|
bromocriptine
|
|
|
What would the relative hormone levels be for a woman with an ovarian-derived amenorrhea?
|
high FSH, LH, low E due to the LOSS OF INHIBIN
|
|
|
What is the criteria for a diagnosis of premature ovarian failure?
|
Cessation of menses before 40
|
|
|
What other comorbidities are associated with ovarian-derived amenorrhea?
|
other autoimmune diseases (addison's, hashimotos, graves, lupus, mg, ra, sprue)
|
|
|
What are the four main causes of hyperandrogenic anovulation?
|
1. congenital adrenal hyperplasia
2. tumors 3. pcos 4. obesity induced anovulation |
|
|
Rapid onset of hirsutism, obesity and virilization in a female patient is associated with what cause of hyperandrogenic anovulation?
|
ovarian/adrenal tumors
|
|
|
What are the main signs and symptoms of PCOS?
|
early menarche
always have had irregular periods insulin resistance |
|
|
What is the pathophys of PCOS?
|
abnl GnRH secretion resulting in high LH/FSH ratio > 2.5-3
also a defect in ovarian steroidogenesis, increase in p450c17 alpha activity |
|
|
Which antiandrogen drug is frequently used in hyperandrogenic anovulation disorders?
|
Spironolactone
|
|
|
What would be the consequence of NOT stopping spironolactone 3 months prior to attempting conception?
|
lack of androgens: if male, he would be born with ambiguous genetalia
|
|
|
Name the segments of the fallopian tube moving from the uterus to the fimbriae.
|
interstitial, isthmic, ampullary, infundibular
|
|
|
The mucosal folds of the ampulla have a layer of supporting tissue (collagen) surrounded by what cell type?
|
single layer of tall columnar epithelial
|
|
|
What are the three types of columnar cells of the ampulla epithelium?
|
ciliated, nonciliated/secretory, intercalated
|
|
|
Moving from lumen of the uterus to the myometrium, name the three layers of the endometrium
|
stratum compactum, stratum spongiosum and stratum basalis
|
|
|
Which layers are shed during menstruation? what is the name of these combined layers?
|
stratum spongiosum and stratum compactum; together they are called the stratum functionalis
|
|
|
What causes the stratum functionalis to shed in menses?
|
contriction of the spiral arteries in response hormonal changes causes the functionalis to be ischemic and shed
|
|
|
How does the myometrium increase in size during pregnancy?
|
hypertrophy and, to a lesser extent, hyperplasia
|
|
|
What are the three functions of the cervix?
|
1. passage of sperm
2. protecting the upper genital tract from microbial invasion 3. dilation for the passage of the fetus and placenta |
|
|
What substance, secreted from the stratified squamous epithelium, inhibits the growth of vaginal pathogens?
|
lactate
|
|
|
What percentage of 15-19 year olds in the US report having intercourse at least once?
|
Nearly half - 46%
|
|
|
By 21 yo, how many people in the US have had sex at least once?
|
82%
|
|
|
For the following age groups, state the percentage of people still sexually active:
57-64 65-74 75-85 |
57-64: 73%
65-74: 53% 75-85: 26% |
|
|
What are the most prevalent reported sexual problems in men and women, respctively?
|
Men: ED
Women: low desire |
|
|
What are the 6 routes of transmission for HIV?
|
Milk
Blood Semen Perinatal Parenteral Sexual |
|
|
What is the #1 way to transmit HIV?
|
unprotected anal intercourse
|
|
|
why in nonoxynol-9 (spermicide) not an appropriate prophylactic for HIV transmission from anal sex?
|
It actually makes the rectal mucosa more tender and more prone to tear.
|
|
|
Which anal sex position (receptive vs. insertive) is more at risk for acquiring HIV?
|
Receptive
|
|
|
Which of the following is only a possibly safe form of sexual contact:
a. light S&M b. frottage (dry humping) c. mutual masturbation d. French kissing e. Fellatio to climax |
D. french kissing (choice e is an unsafe sexual practice and all of the rest are safe)
|
|
|
What is the most common sexually transmitted infection?
|
Chlamydia trachomatis
|
|
|
What can be said about the relative acute and chronic sequelae of Chlamydia infections?
|
fewer acute manifestations and more severe long-term complications
|
|
|
What is the strongest predictor of chlamydia infection?
|
Age
|
|
|
Which age group is at the highest risk for Chlamydial infection? Why?
|
adolescents and young adults; increased exposure to cervical columnar epithelium to the vagina may enhance the ability of the organism to infect new cells
|
|
|
What is the most common chlamydial syndrome in women?
|
cervical infection (clinical diagnosis based on mucopurulent discharge from the cervix)
|
|
|
What percentage of women will develop PID if their Chlamydia infection is left untreated?
|
15%
|
|
|
What are the two most common pathogens associated with epididymitis in men?
|
N. gonorrhoeae and C. trachomatis
|
|
|
What are hte two known initiating pathogens of PID?
|
N. gonorrhoeae and C. trachomatis
|
|
|
What is the pathophys of PID?
|
disturbance of the normally protective endocervical canal provides vaginal bacteria with access to the upper genital organs via canalicular routes infecting the organs of the upper genital tract
|
|
|
What percentage of women with endocervical gonorrhoeae will develop PID?
|
15-30%
|
|
|
What is the most common reported infectious disease?
|
Chlamydia trachomatis
|
|
|
In terms of the microbiology, what type of infection is PID?
|
mixed (facultative and anaerobic) polymicrobial infections
|
|
|
What sign is diagnostic for the most severe form of PID?
|
TOA: tubo-ovarian abcesses
ovary may adhere to the fimbria of hte infected oviduct and become the lateral wall of the abcess or a primary ovarian infection my initiate the abscess (bringing leukocytes to the area) |
|
|
What are the three main sequelae of PID?
|
Infertility
Ectopic pregnancy Chronic Pelvic Pain (CPP) |
|
|
What is believed to be the cause for the syndrome of chronic pelvic pain?
|
adhesions and the resultant tethering/fixation of organs
|
|
|
Of all of the unintended pregnancies in the US, how many are terminated by abortions?
|
4 out of 10
|
|
|
What pattern of cryptorchidism is more common?
|
Unilateral
|
|
|
Does surgical correction of cryptorchidism return malignancy risk to normal?
|
NO: patients are born with increased risk and surgery doesn't change risk
|
|
|
Name some of the congenital causes of male infertility.
|
cryptorchidism, immotile cilia syndrome, absent deferentia, anorchia, hormonal deficiency, Klinefelter's
|
|
|
Name some of the acquired causes of male infertility.
|
torsion, variococele, obstruction, inflammation
|
|
|
Does mumps orchitis generally result in infertility?
|
no, even with severe cell destruction, usually only unilateral
|
|
|
What are the common causes of epididymitis in kids? Sexually active men? Elderly?
|
Anatomic anomalies, GC/CT, enterobacteria
|
|
|
What is the one inflammatory disease that involves testes before epididymis?
|
Syphilis
|
|
|
What is the most common testicular tumor?
|
Seminoma
|
|
|
What variant of seminoma is seen in pts >65 y.o.?
|
Spermatocytic seminoma
|
|
|
What testicular tumors are described grossly as "fresh fish" and microscopically as "fried eggs"?
|
Seminoma
|
|
|
What is most common tumor found in the testicles of men over 60 y.o.?
|
Lymphoma
|
|
|
What percent of infantile testicular tumors are teratomas?
|
forty
|
|
|
What type of tumor might produce gynecomastia or precocious puberty secondary to hormone production?
|
Sex Cord Stromal Tumor (Leydig cell)
|
|
|
What tumor has syncytiotrophoblasts and cytotrophoblasts in it?
|
Choriocarcinoma
|
|
|
What hormone can be used as a tumor marker in choriocarcinoma?
|
hCG
|
|
|
What is the most common testicular tumor in infants and children?
|
yolk sac tumor
|
|
|
What tumor marker can be used for a yolk sac tumor of the testis?
|
alpha-fetoprotein
|
|
|
What chemoresistant tumor presents with cysts on ultrasound and a cytologic mix of mature and immature cells?
|
Teratoma
|
|
|
What three patterns are common to embryonal cancer of the testis?
|
glandular, papillary, trabecular
|
|
|
What percent of testicular tumors are mixed?
|
sixty
|
|
|
Compare the strength of the estrogen compounds.
|
Estradiol > estrone > estriol
|
|
|
What does inhibin do? Activin?
|
inhibits FSH, stimulates FSH
|
|
|
What are the options for administration of exogenous testosterones?
|
IM injections weekly or bi-weekly, gels or patch, buccal tablet
|
|
|
Why are mestranol, ethinyl estradiol and quinestrol degraded less in the liver than endogenous estradiol?
|
there is an ethinyl group added at C16
|
|
|
What are the potential adverse consequences of estrogen use?
|
increase stroke/MI risk, increase uterine/breast Ca risk, increases TGs, clots, gallbladder dz, migraines, HTN (at high doses)
|
|
|
What selective ER antagonist can be used to treat breast cancer but may increase endometrial Ca risk?
|
tamoxifen (also toremifene?)
|
|
|
What selective ER antagonist acts as an agonist at bone but not at the endometrium?
|
Raloxifene
|
|
|
What is meant by "selective ER modulation"?
|
estrogens may be full antagonists, full agonists, or have different effects at different tissues
|
|
|
What drug can be used to treat infertility in women? How?
|
Clomiphene; blocks E2 feedback at pituitary, stimulates the GnRH pulse, stimulating ovulation
|
|
|
Why are aromatase inhibitors superior to tamoxifen in treatment of breast cancer?
|
blocks estrogen synthesis, which limits breast Ca growth, without increasing endometrium Ca risk
|
|
|
What hormone is mainly responsible for maintaining a pregnancy?
|
progestins
|
|
|
What hormone is essential for contraception efficacy?
|
progestins
|
|
|
For whom are hormonal contraceptives contraindicated?
|
pts with hx of CAD, clots or MI, congentical hyperlipidemia, liver tumor/failure, hormone dependent neoplasm, and women over 35 who smoke
|
|
|
How is RU-486 used to terminate a pregnancy? What drug is co-administered?
|
competitively binds uterine receptor, preventing pregnancy growth; given with prostaglandins
|
|
|
At what testosterone level is a man considered hypogonadal?
|
< 290
|
|
|
At what stages of life do males have a testosterone surge?
|
fetal at 6-8 weeks, neonatally, and pubertally (stays high)
|
|
|
Why are testosterone levels hard to maintain when administering exogenous hormones?
|
they are rapildy degraded by the liver
|
|
|
What chemical modification results in slowed liver metabolism of testosterones?
|
alkylation at 17α
|
|
|
What is the consequence of esterification at the 17β-OH site on exongenous hormones?
|
increased lipid solubility
|
|
|
What are the uses of exogenous testosterone administration?
|
tx hypogonadism, breast cancer, osteoporosis, endometriosis, hormone replacement and erythropoeisis stimulation
|
|
|
What androgen receptor antagonist results in increased GnRH, FSH, LH, and androgens? How?
|
flutamide blocks negative feedback
|
|
|
What androgen receptor antagonist results in decreased GnRH, FSH, LH, and androgens? How?
|
cyproterone acetate; mimics progesterone
|
|
|
What are the potential uses of anti-androgenic agents?
|
Tx prostate Ca, acne, male baldness, female virilizing syndromes, and precocious puberty in boys
|
|
|
What are the agents with a anti-androgenic effect?
|
GnRH agonists, ketoconazole (blocks p450 Ezs), spironolactone (anti-aldo), finasteride (blocks 5α reductase)
|
|
|
What are the anabolic effects of androgen that promote hormone abuse?
|
increases muscle mass, bone mass and nitrogen retention
|
|
|
What are the potential adverse consequences of exogenous testosterone use?
|
jaundice, hepatic carcinoma, increases LDL, may increase risk of BPH or prostate Ca
|
|
|
What hormone predominates in the proliferative phase of the menstrual cycle?
|
Estrogen
|
|
|
What main event happens in the secretory phase of the menstrual cycle? What hormone predominates?
|
graafian follicle discharges a single ovum; corpus luteum begins to secrete progesterone
|
|
|
What are the main histologic features one sees during the proliferative phase of the menstrual cycle?
|
cuboidal and columnar cells show increasing stratification of nuclei; mitotic fiures in glands and stromal cells
|
|
|
What are the main histologic features one sees during the secretory phase of the menstrual cycle?
|
16: small, subnuclear vacuoles in the epithelium lining the glands
20: luminal cells become more cuboidal in shape and their border becomes frayed 24: eosinophilic cytoplasm in the stroma |
|
|
What are the main histologic features one sees during the decidual (pregnancy) phase of the menstrual cycle?
|
Arias-Stella phenomenon: endometrial glands become hypersecretory and are widely dilated and lined by cells with glycogen; bizarre nuclear changes in the epithelial cells and crowding of the glands
|
|
|
What is the definition of menopause?
|
6 months of amenorrhea occuring in the 5th or 6th decades of life
|
|
|
What are the histological changes seen in menopause?
|
thinning of the endometrium witha reduxn in the # of glands and amount of stroma; glands are lined with low cuboidal epithelium; no mitoses
|
|
|
What is the most common organic lesion causing abnormal uterine bleeding in postmenopausal women?
|
Carcinoma
|
|
|
What is the definition of Dysfunctional Uterine Bleeding (DUB)?
|
abnl bleeding in the abscence of an organic lesion (tumor) of the endometrium
|
|
|
What is the most common form of DUB?
|
anovulatory bleeding - excessive and prolonged estrogenic stimulation without the development of the progestational phase
|
|
|
What is seen in the stroma of an endometrium with endometritis?
|
Plasma cells, lymphocytes and macrophages
|
|
|
With endometrial hyperplasia, increased cancer risk corresponds to what other factor accomanying the hyperplasia?
|
the degree of cytologic (cellular) atypia
|
|
|
What percentage of atypical endometrial hyperplasia progress to carcinoma?
|
30%
|
|
|
What does atypical endometrial hyperplasia appear as, cellularly?
|
cytomegally, loss of polarity, hyperchromatism, altered nuclear:cytoplasmic ratio; many mitotic figures
|
|
|
What is the treatment for atypical endometrial hyperplasia?
|
hysterectomy is the therapy of choice in women who have completed childbearing; high dose progestins can induce remission, but recurrence is possible
|
|
|
From which layer of the endometrium do endometrial polyps arise?
|
Zona basalis
|
|
|
What is the most common invasive cancer of the female genital tract?
|
endometrial carcinoma; 7% of all invasive cancers in women
|
|
|
A higher frequency of endometrial carcinoma is seen with what other comorbidities?
|
1. obesity
2. Diabetes 3. HTN 4. Nulliparity, infertility 5. FHX |
|
|
What specific findings in the family history would cause concern for endometrial carcinoma?
|
1. cancer family syndrome (Lynch Syndrome II)
2. increased incidence of breast and endometrial cancer in 1st degree relatives 3. predisposition for endometrial carcinoma alone |
|
|
What seems to be the pathophys of endometrial carcinoma?
|
prolonged estrogen stimulation
|
|
|
Describe the two types of endometrial cancer (Type I and II)
|
Type I: estrogen-related neoplasm, slightly younger, obese women; 80% of cases, well differentiated "endometriod" type
Type II: unrelated to estrogen stimulation, occurs in older postmenopausal women, much more aggressive; unusual histologic types |
|
|
State the two facets of the dualistic model on the molecular pathology of endometrial carcinogenesis
|
1. replication errors, microsatelite instability and subsequent accumulation of oncogenes and tumor suppressors
2. alterations of p53 and loss of heterozygosity |
|
|
What are the 4 main molecular alterations supporting the 1st component of dualistic model for endometrial carcinogenesis?
|
microsatelite instability
PTEN gene (Ch10) k-RAS Beta-catenin |
|
|
What are the two ways that an endometrial carcinoma can present, grossly?
|
1. localized polypoid tumor
2. Diffuse tumor involving the entire endometrial surface |
|
|
Define adenomyosis. What is the common age range?
|
Presence of endometrial glands and/or stroma beneath the endometrial-myometrial jnxn; affects 30-40 yo age group
|
|
|
What are the two myometrial smooth muscle tumors?
|
1. leiomyoma
2. leiomyosarcoma |
|
|
In which 3 locations of the uterus are leiomyoma found?
|
1. submucosal
2. intramural 3. subserosa |
|
|
What do leiomyomas look like in gross pathology?
|
grey-white whorled, well-circumscribed
|
|
|
What is the treatment for leiomyoma?
|
myomectomy
hysterectomy uterine artery embolization |
|
|
What is the most common uterine sarcoma?
|
leiomyosarcoma
|
|
|
What are the 3 CLASSIC features of a leiomyosarcoma?
|
1. increased number of mitosis
2. marked cytologic atypia 3. tumor necrosis |
|
|
What is the 5-year survival rate for leiomyosarcoma?
|
40%
|
|
|
What are the 4 main categories of Gestational Trophoblastic Disease?
|
1. Hydatidiform Mole
2. Invasive Mole 3. Choriocarcinoma 4. Placental Site trophoblastic tumor |
|
|
Which form of gestational trophoblastic disease is the most common precursor for choriocarcinoma?
|
Hydatidiform Mole
|
|
|
What is the age group and CLASSIC symptoms of Hydatidiform moles?
|
reproductive age group
Sx: "passing grapes," absent fetal heart sounds, markedly increased bHCG |
|
|
What is the karyoptype of a complete hydatidiform mole
|
46XX - all from paternal DNA
|
|
|
What is the karyotype for a partial hydatidiform mole?
|
triploid (69 chrs) with one maternal and two paternal haploid sets (normal egg fertilized by two sperm
|
|
|
What percentage of moles remain benign? develop into choriocarcinoma?
|
80-90% benign
2.5% to choriocarcinoma |
|
|
Following a hysterectomy for a mole, what does a rise in HCG levels indicate?
|
persistent mole, invasive mole, or choriocarcinoma
|
|
|
Is uterine curettage possible with invasive moles?
|
No, penetration is too deep into the uterine wall
|
|
|
Gestational choriocarcinoma is a malignancy of what type of cells?
|
trophoblastic
|
|
|
Choriocarcinomas are highly sensitive to chemotherapy. Which drug is effective in treating choriocarcinomas?
|
Methotrexate
|
|
|
How do you distinguish a choriocarcinoma from a mole?
|
there are NO villi present
|
|
|
Where is the most common site for an ectopic pregnancy?
|
Fallopian tubes (90%)
|
|
|
What is the most common cause of ectopic pregnancy?
|
PID with salpingitis
|
|
|
When do the signs and sx of an ectopic pregnancy manifest?
|
2 to 6 weeks after implantation
|
|
|
What type of cysts occupy the ovary in PCOS?
|
follicular (not luteal)
|
|
|
What is the histologic difference between a follicular and luteal cyst?
|
Follicular: lined by granulosa cells and filled with clear serous fluid; luteal: lined by bright-yellow luteal tissue
|
|
|
What are the most common presenting symptoms in a patient with ovarian tumor(s)?
|
abdominal pain/distention, vaginal bleeding, urinary or GI complaints
|
|
|
Why do most ovarian tumors only create symptoms when they reach a certain size?
|
most are non-functional (produce no hormone) and therefore are associated with only mild sxs until they are large
|
|
|
What percentage of patients with an ovarian tumor present with a tumor outside the ovary?
|
more than 75%
|
|
|
What component of the the ovary gives rise to the vast majority of tumors?
|
epithelium
|
|
|
What is the significance of an ovarian adenocarcinoma positive for HER-2/-neu mutation?
|
correlates with poorer clinical prognosis
|
|
|
What two important risk factors predispose to the development of ovarian carcinoma?
|
nulliparity and family history (esp BRCA 1 or 2)
|
|
|
What morphologic finding is associated with malignant ovarian tumors but NOT borderline or benign tumors?
|
invasion of the stroma (malignant are more likely to have layered epithelium, nuclear atypia and solid masses of tumor as well)
|
|
|
In what ovarian tumor are Psammoma bodies sometimes found?
|
Serous papillary ovarian adenocarcinoma (Cystadenocarcinoma)
|
|
|
What are Psammoma bodies?
|
round, reddish collection of calcium
|
|
|
What should you do if you find bilateral mucionous ovarian tumors?
|
Check very carefully to make sure that they are not secondary metastases from GI primary
|
|
|
What are three types of ovarian tumor which arise from the surface epithelium?
|
serous, mucinous, and endometrioid
|
|
|
What is the most likely cause of pseudomyxoma peritonei?
|
ruptured appendix (can be due to mucinous ovarian tumor, but less likely)
|
|
|
Which of the ovarian epithelial tumors is most likely to be malignant?
|
endometrioid
|
|
|
What age patient is more likely to have a germ cell tumor of the ovary?
|
child or young adult
|
|
|
What germ cell tumor is the most common?
|
95% are benign cystic teratomas
|
|
|
If most germ cell tumors are benign teratomas, what are the rest?
|
DICEY (Dysgerminoma, Immature Teratoma, Choriocarcinoma, Embryonal, Yolk sac tumor)
|
|
|
What germ cell tumor has hyaline droplets (representing alpha-fetoprotein) and Schiller-Duvall Bodies?
|
yolk sac tumor
|
|
|
What germ cell tumor has long sheets vesicular cells with cleared cytoplasm surrounded by septa?
|
dysgerminoma (seminoma in men)
|
|
|
How might you treat a dysgerminoma? What about a yolk sac tumor?
|
radiotx, combo-chemo tx
|
|
|
What sex-cord stromal tumor has Call-exner bodies (immature follicle structures) and causes precocious puberty?
|
Granulosa cell tumor
|
|
|
What sex-cord stromal tumor has is most likely to cause defeminization?
|
androblastoma
|
|
|
What is a Krukenberg tumor?
|
Metastases of gastric tumor to the ovary, bilateral, has mucin-producing signet ring cells
|
|
|
What three groups of women should continue having annual paps after age 30, even after 3 consecutive NL results?
|
HIV positive, immunocompromised, history of CIN 2 or 3, women who received DES in utero
|
|
|
What type of cancer is most common in the cervix?
|
80% are squamous cell carcinoma
|
|
|
What happens to the Squamocolumnar junction in the presence of high estrogen levels?
|
moves distal to cervical os
|
|
|
Where do most premalignant squamous lesions of the cervix originate?
|
at the squamocolumnar junction
|
|
|
Why is metaplasia a normal finding at the SCJ of the cervix?
|
because reserve cells here can become EITHER squamous or columnar
|
|
|
What findings correlate with a pap result called CIN (cervical intraepithelial neplasia)?
|
squamous cells at surface, which should be flattened and have small nuclei, look like basal cells - cuboidal and large nuclei
|
|
|
What cytologic findings on Pap smear represent the loss of cellular differentiation at the surface of the cervical epithelium?
|
increased nucleus:cytoplasm ratio; decreased cytoplasm overall
|
|
|
What abnormalities are considered part of the LSIL category?
|
condyloma, mild dysplasia, and CIN 1 lesions
|
|
|
What abnormalities are considered part of the HSIL category?
|
CIN 2 (moderate dysplasia), CIN 3 (severe dysplasia) and Carcinoma in Situ
|
|
|
What is meant by Carcinoma in Situ on a pap result?
|
dysplasia has affected the full thickness of the stratified squamous epithelium, but has NOT invaded the basal layer
|
|
|
What strains of HPV have been correlated with low-grade lesions in the U.S?
|
6, 8 and 11
|
|
|
What strains of HPV have been correlated with high-grade lesions in the U.S?
|
16, 18
|
|
|
From a biologic standpoint, what differentiates condylomata and dysplasia from overtly malignant cervical lesions?
|
integration of the viral (HPV) DNA into the Host DNA
|
|
|
What HPV strains are covered by the vaccine?
|
6, 11, 16, and 18
|

