![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
What is the most common neoplasm of the middle ear?
|
Glomus Tumor (paraganglioma) - aka chemodectoma
|
|
|
What is the second most common neoplasm of the temporal bone/cerebellopontine angle?
|
Glomus Tumor (paraganglioma)
|
|
|
What are the three types of glomus tumors of the temporal bone?
|
Glomus tympanicum (GT) - on tympanic promontory
Glomus jugulare (GJ) - along jugular dome Glomus vagale (GV) - along Jacobson's and Arnold's nerves |
|
|
Are glomus tumors typically benign or malignant?
|
Benign - only 2-4% malignant
|
|
|
Are glomus tumors typically functioning or nonfunctioning?
|
nonfunctioning - only 5% or less secrete neuroactive peptides
|
|
|
What type of cells do glomus tumors arise from?
|
chemoreceptor cells of the neuroendocrine system
|
|
|
Which two classification systems are used for glomus tumors?
|
Fisch
Glassock-Jackson - GT and JG only |
|
|
What are some symptoms in a pt with glomus tumor?
|
Pulsatile tinnitus (80%) - GT and GJ
Hearing loss, conductive or mixed (60%) - GT or GJ Aural fullness (32%) - GT and GJ Hoarseness/dysphagia (15%) - GJ Facial weakness (15%) - GT and GJ Otalgia (13%) - GT and GJ Functional tumors will present with palpitations, unexplained weight loss, and poorly controlled hypertension. |
|
|
Brown sign is seen in glomus tympanicum. What is this sign?
|
blanching of middle ear mass with pneumatic otoscopy
|
|
|
What laboratory workup is needed for glomus tumor workup?
|
Urine for vanillylmandelic acid (VMA), metanephrines
- must be 5x higher than normal to be symptomatic - used to exclude a functional component |
|
|
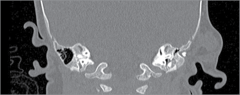
What is the imaging modality of choice for glomus tumors of the temporal bone?
|
CT of the internal auditory canal
|
|
|
What classic appearance is there of glomus tumors on MRI's?
|
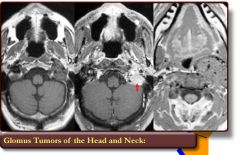
"salt and pepper" apperance due to flow voids within the tumor
|
|
|
What must be done 24-48 hrs prior to surgical resection of a glomus tumor to improve intraoperative blood loss?
|
four-vessel angiography with embolization of the feeding vessels
|
|
|
How is glomus tympanicum treated?
|
Glomus tumors in general are surgical diseases unless patient's comorbidities prevent operation.
Small glomus tympanicum tumors to the promontory can be removed via a transcanal or anterior tympanostomy approach Large tumors require wider exposure via mastoidecetomy and posterior tympanostomy |
|
|
How is glomus jugulare treated?
|

Glomus tumors in general are surgical diseases unless patient's comorbidities prevent operation.
Requires proximal control of the great vessels in the neck and the sigmoid sinus. Large tumors = may require transposition of the facial nerve to exposure the tumor anteriorly Method of choice for removal = Infratemporal fossa approach. |
|
|
What role does radiation play in glomus tumors of the temporal bone? What about stereotactic radiosurgery?
|
Used in pts who cannot withdtand surgery or refuse surgery.
Used to prevent further tumor growth. Likely efficacious due to fibrosis of the arterioles rather than direct effect on tumor cells. Lower doses are sued for malignancies (15 Gy) Stereotactic radiosurgery has reported 80% rate of tumor control. ***Risks: radiation-induced malignancy, osteoradionecrosis of the skull base, temporal lobe necrosis, cranial nerve injury |
|
|
What is the general info on endolymphatic sac tumors?
|
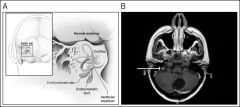
locally aggressive tumors of the endolymphatic sac
can be sporadic or associated with von Hippel-Lindae (VHL) dz - pts with VHL can have bilateral tumors and should be screened for this. |
|
|
What are the symptoms of a pt with an endolymphatic sac tumor?
|

That of endolymphatic hydrops - likely due to obstruction of the normal flow and resorption patterns of endolymph
- SNHL - Tinnitus - Aural fullness - Vertigo - Late sx include facial paralysis, sx of brainstem compression, and lower cranial neuropathies. |
|
|
What will you see on CT imaging of an endolymphatic sac tumor?
|
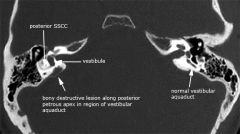
bony destruction of the posterior fossa plate with central calcification's
may extend into the mastoid as well |
|
|
What will you see on MRI imaging of an endolymphatic sac tumor?
|
T1 - isointense to hyperintense when compared to cerebellar white matter
T2 - heterogenous (suggesting its highly vascular nature) T1 with contrast - strongly enhancing |
|
|
What treatments do you recommend to a pt with an endolymphatic sac tumor?
|
Surgery is the method of choice
Should involve removal of both surfaces of the dura to ensure complete removal For small tumors, may use hearing sparing approaches, such as retrolabyrinthine-transdural approach. For pts with nonserviceable hearing - translabyrinthine approach. Large tumors can be preoperatively embolized to minimize blood loss |
|
|
What does a hemangioma of the temporal bone typically present like?
|
It's a rare (<1% of temporal bone tumors) benign tumor that arises from blood vessels.
Typically associated with the facial nerve, particularly the geniculate ganglion Slowly progressive or recurrent facial weakness with twitching. Locally aggressive resulting in bony destruction. - erosion into the cochlea results in SNHL - dilation of the fallopian/internal auditory canal |
|
|
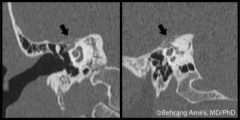
Which CT and MRI findings are seen in a pt with hemangioma of the temporal bone?
|
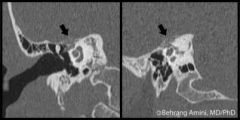
CT- infiltrative erosive lesion centered at the geniculate ganglion
- may erode into cochlea or labyrinth - intratumor calcifications are common MRI - on T1 imaging hypo to isointense to brain and enhance avidly with contrast |
|
|
What treatment do you recommend to a pt with hemangioma of the temporal bone?
|
Small lesiosn can be meticulously dissected free from the nerve when centered at the geniculate with full preservation of facial function.
Larger lesions or those with complete facial paralysis, tx is resection with nerve nerve grafting. For IAC lesions, unless face is paralyzed, surgical tx involves decompression of the IAC as resection requires nerve resection and nerve grafting. |
|
|
What is a chordoma?
|

Unusual locally aggressive neoplasm of the clivus; impacts the temporal bones by lateral extension of the tumor into the CPA or lower cranial nerves
Mets are rare |
|
|
From what does a chordoma develop from? Which cells are seen on histology?
|
Develops from the notochord remnant
Histology: physaliferous cells |
|
|
How does chordoma present?
|
With diplopia due to involvement of CN 6 as it passes through Dorello canal and headaches
- involvement of CN 5 also common Five year survival rate = 51% |
|
|
How do you treat a patient who presents with chordoma?
|
Surgical resection is the gold standard
- incomplete resection should be followed with adjuvant radiation - biactive chemotherapeutic agents are in clinic trials) - approaches include infratemporal fossa - can also be managed with transnasal endoscopic resections in combination with lateral skull base approaches |
|
|
What is a choristoma? How does it present?
|
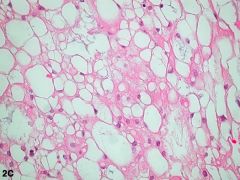
by definition, it's a mass of histologically normal tissue in an abnormal location.
most common histologic type is salivary tissue other types include lipoma's, and glial choristoma's (image) presents with CHL and middle ear effusion Tx is surgical excision |
|
|
What is the most common overall malignancy of the temporal bone?
What's the mc of the EAC? What's the mc of the middle ear? What's the mc of the pinna/conchal bowl |
What is the most common overall malignancy of the temporal bone? = SCCA
What's the mc of the EAC? = SCCA What's the mc of the middle ear? = SCCA What's the mc of the pinna/conchal bowl = basal cell ca |
|
|
What is the frequency of temporal bone SCCA?
|
Rare tumor representing <0.2% of all H&N malignancies
|
|
|
List a few possible risk factors or causations of temporal bone SCCA.
|
Older literature associated chronic inflammator/otorrhea of the EAC or middle ears as in chronic otitis externa or chronic otitis media.
HPV Prior radiation for unrelated dz |
|
|
What is the most common Sx of temporal bone SCCA?
|
Otorrhea - most common complaints (60-80%)
Others include: Otalgia (50-60%) Hearing loss (20-60%) Bleeding (5-20%) |
|
|
Any pt with primary SCCA of the ME/mastoid is automatically in T__ stage disease
|
T3-T4 (advanced-stage dz)
|
|
|
From the EAC, where is the pattern of spread for the following locations?
Anteriorly - Laterally - Medially - Posteriorly - Inferiorly - Superiorly - |
Anteriorly - into the TMJ; parotid via direct bony erosion, invasion of the fissures of Santorini (cartilaginous EAC) or patent foramen of Huscke (bony EAC)
Posteriorly - into the mastoid via direct bony erosion Laterally - into the meatus and conchal bowl Medially - through the TM/annulus in the middle ear and attic Inferiorly - into mastoid and stylomastoid foramen usually through direct bony erosion but may have perineural spread along the facial nerve into the foramen. Superiorly - into the root of zygoma and intracranial space through direct bony erosion |
|
|
What is the 5-year prognosis of all pt's with SCCA of the temporal bone?
|
30-45%
|
|
|
In pts with SCCA of the temporal bone, at which T stages is adjuvant radiation recommended?
|
T2, T3, T4
(in T1, no XRT if negative margins) |
|
|
What are the surgical options for treatment of SCCA of temporal bone?
|
Lateral temporal bone resection (T1, T2)
Subtotal temporal bone resection (T3, T4) Total temporal bone resection (T4) - rarely performed |
|
|
Why is en bloc total temporal bone resection rarely performed?
|
due to significant operative mortality and postop morbidity
|
|
|
What is the mc malignancy of the temporal bone in childhood?
|
rhabdomyosarcoma
|
|
|
What are the subtypes of rhabdomyosarcoma of the temporal bone?
|
Embryonal (mc)
Alveolar Boytroid Spindle cell Anaplastic |
|
|
What is the immunohistochemistry staining of rhabdomyosarcoma of the temporal bone?
|
Desmin
MyoD1 Myogenin Muscle-specific actin |
|
|
What is the mainstay of treatment for rhabdomyosarcoma of the temporal bone?
|
Chemotherapy
- surgery is used for diagnostic biopsy - radiation is used in conjunction with chem |
|
|
What are the top 3 cancers that mets to the temporal bone?
|
1) breast
2) lung 3) GI |

