![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
Carotid body tumors are also known as what?
|
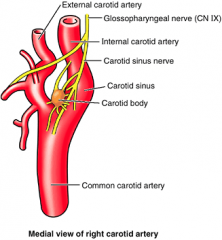
Globus caroticum
They are benign neuroendocrine tumors arising from carotid body paraganglia |
|
|
What are the normal functions of carotid body?
|
As a chemoreceptor for changes in blood oxygen, carbon dioxide, and hydrogen ion concentration.
|
|
|
What are the two cells types of the carotid body?
|
Chief cells (Type I) - neural crest derived and are the cells capable of releasing neurotransmitters
Sustentacular cells (Type II) - supporting cells similar to glia |
|
|
What is the "zellballen" configuration of carotid body tumors?
|

Tumors nests surrounded by fibrovascular stroma
|
|
|
What is the most common paraganglioma of the head & neck?
|
Carotid body tumors (45-60%)
|
|
|
What are the three types of carotid body tumors?
|
Sporadic - most common; usually in children; rarely bilateral
Familial - presents even younger than sporadic; increased incidence of bilaterality (30%) and other paraganglia including pheo Hyperplastic - in populations living at higher altitudes; though to be due to chronic hypoxia; more commonly in women (may be related to anemia from menses) |
|
|
What is the physical exam presentation of a carotid body tumor?
|
Most common presentation is neck mass (deep mass high in the neck)
Tethered vertically but mobile horizontally (Fontaine sign) May be pulsatile or have a bruit |
|
|
What are the Shamblin classifications of carotid body tumors?
|
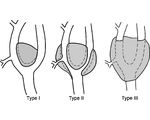
Type I - small tumor easily separated from carotid
Type II - tumor partially encircles carotid and is difficult to separate Type III - tumor completely encircles carotid and is densely adherent |
|
|
How common are carotid body malignancies and what is the most predictive feature?
|
Rare, 5-10%
PAIN is the most predictive feature, along with young age and rapid enlargement No histologic criteria of malignancy for primary tumor Malignancy is defined as the presence of regional or distant mets; local invasion or destructive behavior does not establish malignancy. |
|
|
What is the incidence of a carotid body tumor turning functional?
|
Rare, 1-3%
If hx of HTN or flushing consider workup for catecholamine byproducts (best screening test is plasma free metanephrines, second best is 24hr urine fractionated metanephrines) Sx may be due to another, synchronous tumors (ie. pheo) |
|
|
What is the best initial imaging study for carotid body tumor?
|
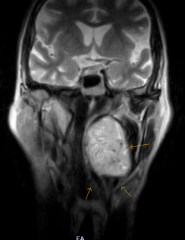
CT or MRI with contrast (hypervascular mass, usually splaying internal and external carotid)
MRI appearance described as "salt and pepper" Halo between carotid and tumor suggests a good plane of separation. - remember, if the tumor is located ABOVE the bifurcation, even it it splays the carotids, an entity other than a carotid body tumor should be expected. |
|
|
What is the "lyre" sign?
|
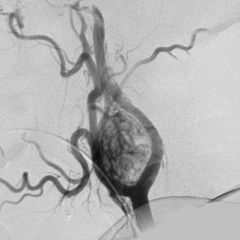
The lyre sign refers to the splaying of the internal and external carotid by a carotid body tumour. Classically described on angiography it is also visible on CT angiography.
|
|
|
Is preoparative embolization necessary prior to carotid body tumor excision?
|
Has not been shown to reduce intraoperative blood loss and is usually not necessary
|
|
|
What is the preferred treatment modality for small carotid body tumors in healthy pts?
|
Surgical resection
- transcervical approach with level II and II selective neck dissections to improve exposure and sample nodes - vascular surgery should be available for carotid replacement as decision to resect the carotid made intraoperatively. |
|
|
Which nerves are more commonly injured during surgical resection of carotid body tumors?
|
CN 10 & 12, incidence is low for most tumors
|
|
|
What is first bite syndrome?
|
Complication of carotid body tumor resection
- intense parotid pain on initiating eating due to injury of cervical sympathetics; usually worst in the morning and tends to improve with time. |
|
|
What is baroreflex failure?
|
Complication of carotid body tumor resection
- tachycardia and blood pressure lability due to loss of carotid sinus reflex mediated by Hering's nerve (branch of CN 9); more significant for pts with bilateral surgery |
|
|
Is radiation therapy an option for carotid body tumors?
|
Yes, an option for unresectable cases, poor operative candidates, or by pt preference
- tumors typically DO NOT regress but remain radiologically stable - Post-op XRT should be considered for metastatic cases |
|
|
What are vagal paragangliomas also known as?
|
Glomus vagale
|
|
|
How do vagal paragangliomas typically present?
|
Can extend to skull base or intracranially
Typically arise from the inferior (nodose) ganglion but can arise fro mimddle or superior ganglion Represent 5-9% of head and neck paragangliomas Histopathology same as for carotid body tumors Higher incidence of malignancy that carotid body tumors (16%) Preop weakness of CN X occurs in 1/3 of pt's |
|
|
How are vagal paragangliomas diagnosed?
|
Contrast-enhanced CT or MRI
- vascular tumor typically displacing carotids anteromedially without splaying - Vagal tumors tent to separate the jugular vein from the carotid sheath, whereas sympathetic tumors typically do not - Can splay carotids and mimic a carotid body tumor.. |
|
|
How are vagal paragangliomas treated?
|
Surgical resection
- essentially guarantees vagal paralysis - used for aggressive tumors invading the skull base and for pts with preexisting vagal paralysis - cervical approach used for lower tumors and lateral skull base approach for higher tumors - If dx of vagal paraganglioma made intraoperative when carotid body tumor is suspected, it is reasonable to abort procedure and either give radiation or observation. Radiation therapy or observation - preferred for pts with small tumors and no preexisting vagal weakness - otherwise same as for carotid body tumors |
|
|
What are schwannomas tumors also called?
|
Neurilemomas or neurinomas
|
|
|
What are schwannomas?
|
Encapsulated tumor composed of Schwann cells
Schwann cells normally produce myelin for extracranial nerves; derived from neural crest cells. |
|
|
What are the two histological patterns of schwannomas?
|
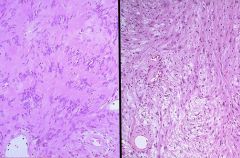
Antoni A - pAlisading Schwann cells arranged in Verocay bodies; more cellular and organized (left image)
Antobi B - random arrangement within loose stroma (right image) |
|
|
Most schwannomas of the head and neck occur in which cervical space?
|
parapharyngeal space (second most common tumor in this space)
|
|
|
How are schwannomas diagnoses and treated?
|
Nerve weakness - can occur in nerve of origin, however, not diagnostic as nerve weakness may be due to compression or invasion by a tumor arising from another local structure (ie. carotid body tumor causing Horner's syndrome)
CT or MRI with contrast - tumors demonstrates enhancement during venous phase, but do not show as intense enhancement as paragangliomas. Surgical resection is preferred modality and usually curative. |
|
|
What are the two types of hemangiomas?
|
Congenital and infantile
|
|
|
What are the two types of congenital hemangioma's?
|
Rapidly involuting and noninvoluting
- rare tumor present at birth - Glucose transporter 1 (GLUT1) negative |
|
|
What is the most common vascular anomaly in the head and neck?
|

Infantile hemangioma
- GLUT1 positive (stain used to confirm dx if in question) |
|
|
What are the three anatomic locations of infantile hemangioma's?
|

Superficial - bright red , clobblestoned, cutaneous, or mucosal mass
Deep - no cutaneous/mucosal component, bluish hue of overlying skin (IMAGE) Compound - superficial and deep components |
|
|
What are the phases of growth of an infantile hemangioma?
|
Proliferative - first 9-12 month of life
Involution - variable course of regression over many years; graying of lesion, "herald spot" is usually first sign of involution Involuted - almost all by 9yo (classically = "50% involuted by 5yrs, 70% by 7yrs and 90% by 9yrs) |
|
|
What are the three distribution patterns of infantile hemangioma's?
|
Focal - classic solitary mass
Multifolcal - multiple masses Segmental distribution - multiple cervicofacial subunits or large areas of upper aerodigestive tract |
|
|
If a kid has multifocal infantile hemangioma and has more than five cutaneous masses, what must you rule out?
|
Liver and GI involvement with abdominal US
|
|
|
Segmental infantile hemangiomas usually follow which nerve pattern?
|
Trigeminal (V1, V2 and/or V3)
- 2/3rd of children with V3 ("beard") distribution will have synchronous subglottic hemangioma - MUST eval airway! |
|
|
What is the most common parotid tumor of infancy?
|

Parotid hemangioma
|
|
|
Intervention is imperative for hemangiomas under which conditions?
|
Symptomatic - ie. bleeding, ulcerated, massive and resulting in CHF or Kasabach-Merritt phenomenon (consumptive coagulopathy)
Critical anatomic locations - eyelids, lips, ears, airway |
|
|
What are options for medical management of hemangiomas?
|
Intralesional steroid injections
Systemic steroids or chemotherapy (alpha-interferon, vincristine, have significant side effects, but are used for symptomatic or critically located tumors) Most recently propranolol has shown success in causing regression |
|
|
What are vascular malformations categorized by?
|
Blood flow: slow flow or fast flow
|
|
|
What are the three different types of slow flow vascular malformations?
|

Capillary vascular malformation (ie. "stork bite"; image)
Venous vascular malformation Lymphatic vascular malformation |
|
|
What are the two different types of fast flow vascular malformations?
|
Arteriovenous malformations (AVM's)
Arteriovenous fistulas (AVF's) |
|
|
List some examples of capillary vascular malformations
|
Telangiectasias
Nevus flammeus (port wine stain) Spider angioma Sturge-Weber syndrome (port wine stain of face with pisilateral inctracranial angiomas/AVM's) |
|
|
What is the most common site in body for lymphatic vascular malformations?
|

Cervicofacial region
|
|
|
What are the two classifications of lymphatic vascular malformations?
|
Macrocystic and microcystic
Macrocytic is easier to treat and have a better prognosis - some small, posterior triangle, macrocystic lymphatic malformations regress spontaneously within the first year of life |
|
|
How do AVM's typically form?
|
Form from a nidus of abnormal capillary beds
|
|
|
How are arteriovenous malformations (AVM's) diagnosed?
|
Lesions usually present as a vascular blush that expands as the pt grows
Lesion can be pulsatile to palpation and have a bruit Advanced lesions can have local tissue and bone destruction, bleeding and pain. Often misdiagnosed as hemangioma in infancy until regression does not occur, with considerable additional morbidity. Can present much later in life (4-5th decades) with evidence of a posttraumatic etiology Most dx in infancy or childhood and grow intermittently secondary to environmental stimuli. |
|
|
How are arteriovenous fistula (AVM's) diagnosed?
|
Posttraumatic
Defined by single AV connection, rather than a nidus of multiple connections |
|
|
How are slow-flow vascular malformations diagnosed?
|
Slow-flow vasc malformations = capillary, venous, lymphatic
- US is most useful for dx - MRI is helpeful for delineating extent of lesions |
|
|
What are the tx options for slow-flow vascular malformations diagnosed?
|
Conservative management: elevate head of bed; warm compresses and NSAIDs
Sclerotherapy (ie ethanol, bleomycin, OK-434 (inactivated Strep pyogenese)) Laser therapy (KTP and Nd:YAG are first-line) Surgery - best option for "cure" |
|
|
How are AVM's diagnosed?
|
Doppler US will demosntrate rapid blood flow, and MRI will usually show flow voids
CT angiogram is useful for operative planning |
|
|
How are AVM's treated?
|
Tx is difficult and multidisciplinary
Embolization of nidus with alcohol or polymers Surgical resection following embolization - small, easily resectable lesions - life-threatening, destructive lesions; often requires massive resection with adjacent or free tissue transfer Recurrence is common |
|
|
How are AVF's diagnosed?
|
Angiography or CT angiography demonstrates single AV connection
|
|
|
How are AVF's tx?
|
Embolization only for deep, inconspicuous lesions
Surgical resection in highly visible lesions (ie. lip) to eliminate residual scar and return of normal function - may consider preop embolization to decrease intraoperative blood ob - if no embolization it is useful to identify and clip feeding artery early in resection |
|
|
OK-432 has been shown to be effective for which type of vascular malformation?
|
macrocystic lymphatic malformations
|

