![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
139 Cards in this Set
- Front
- Back
|
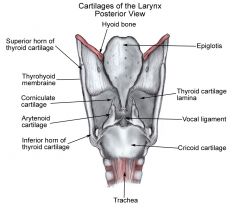
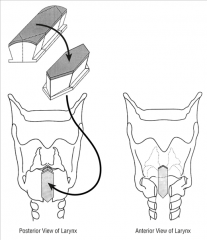
The posterior thyroid cartilage has a superior and inferior cornuae. What do they both attach to?
|
Superior cornuae - thyroid ligaments connect it to the hyoid bone
Inferior cornuae - articulates with the cricoid cartilage |
|
|
Which cartilage is the strongest of the laryngeal cartilages?
|
Cricoid cartilage (the only complete ring in the airway)
|
|
|
What does the shape of the cricoid cartilage resemble?
|
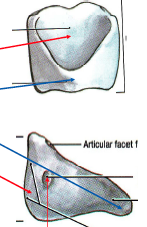
A signet ring (flat and wide posteriorly)
|
|
|
What shape does the epiglottis resemble?
|
Leaf shapped
- petiole is the point of attachment to the thyroid cartilage |
|
|
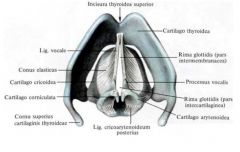
What are the two processes on the arytenoid cartilages?
|

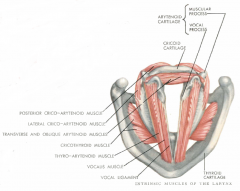
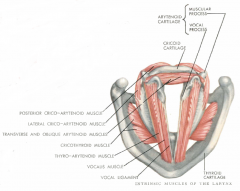
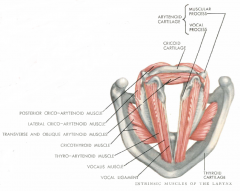
Vocal process - anterior projection of each arytenoid; site of attachment for thyroarytenoid muscle
Muscular process - lateral projection; site of insertion of the lateral and posterior cricoarytenoid muscle The interarytenoid muscle connects the medial surfaces of these cartilages |
|
|
What are the two laryngeal sesamoid cartilages?
|
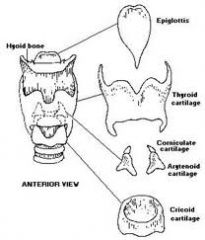
Small cartilages above the arytenoid in the aryepiglottic fold.
- Corniculate cartilages (aka cartilages of Santorini) - Cuneiform cartilages (aka cartilages of Wrisberg) |
|
|
What is a triticeous cartilage?
|
Small elastic cartilage in thyrohyoid ligament
Not always present Sometimes mistaken for a foreign body on soft tissue x-ray films |
|
|
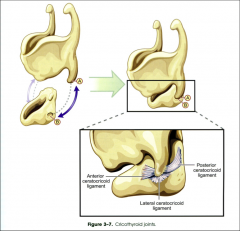
What are the two main laryngeal joints?
|
Cricoarytenoid joint - motion is primarily rotational, about a variable axis, with little gliding motion.
- Arytenoid rotates EXternally to move vocal process upward and outward - Arytenoid rotates Cricothyroid joints - primary motion is like a visor, or bucket handle, with minimal sliding. |
|
|
The thyrohyoid membranes is pierced on each side by what vessels/nerves?
|
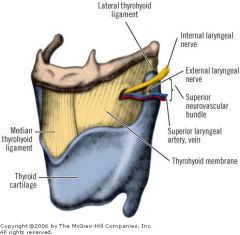
internal branch of superior laryngeal nerve and accompanying artery
|
|
|
What is the thickened median portion of the thyrohyoid membrane called? What about lateral?
|
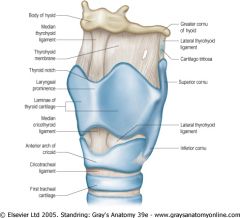
Median thyrohyoid ligament
Lateral thyrohyoid ligament |
|
|
Which membrane is pierced during an emergency tracheotomy?
|
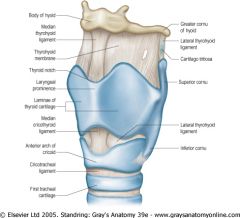
Cricothyroid membrane
(the median cricothyroid ligament overlies the membrane anteriorly) - relatively avascular |
|
|
What attaches the cricoid cartilage to the first tracheal ring?1
|
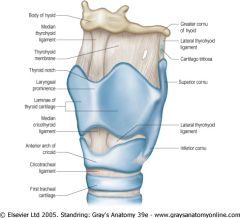
Cricotracheal ligament
|
|
|
The hyoepiglottic ligament connects what?..
|
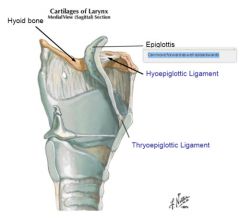
Posterior surface of the hyoid bone and the lingual side of the epiglottis
|
|
|
What is the quadrangular membrane and what are it's attachments?
|
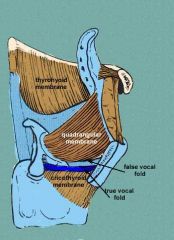
Horizontal extent: from epiglottis to the arytenoids and corniculate cartilages
- extendes inferiorly to the false vocal cords - forms upper part of the elastic membrane (the fibrous framework of the larynx) |
|
|
What is the conus elasticus?
|
AKA cricovocal membrane or triangular membrane (lateral portion of the cricothyroid ligament)
- inferior attachment - superior border of the cricoid cartilage inferiorly - superior anterior attachment - deep surface of apex of the thyroid cartilage - superior posterior attachment - vocal process of the arytenoid cartilage - forms lower potion of elastic membrane (below the ventricle) |
|
|
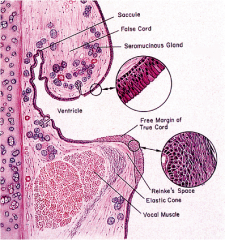
What is the vocal ligament?
|
Free upper edge of the conus elasticus
- inserts onto the anterior thyroid cartilage as Broyle's ligament |
|
|
List the depressor muscles (and innervations) of the larynx
|
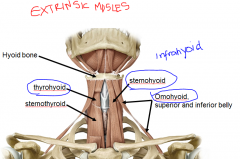
The three muscles that are attach to the inferior hyoid:
Sternohyoid (C2, C3) Thyrohyoid (C1) Omohyoid (C2, C3) |
|
|
List the elevator muscles (and innervations) of the larynx
|
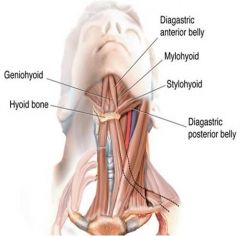
Geniohyoid (C1)
Digastric (anterior belly V; posterior belly VII) Mylohyoid (V) Stylohyoid (VII) |
|
|
What are the innervations of the pharyngeal constrictor muscles and where are their laryngeal attachments?
|
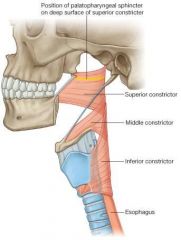
All innervated by pharyngeal plexus; all insert on posterior midline raphe.
Superior constrictor - does not attach to the larynx Middle constrictor - arises from hyoid and stylohyoid ligament Inferior constrictor - arises from oblique line on thyroid cartilage. |
|
|
Which muscle makes up the upper esophageal sphincter?
|

Cricopharyngeus muscle - continuous muscle that surrounds the esophageal inlet and attaches to each side of the cricoid cartilage.
|
|
|
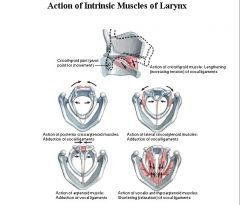
Which nerve innervates most if the intrinsic laryngial muscles?
Which is the one muscle that is not innervated by this nerve? Which nerve is it innervated by? |
Recurrent laryngeal nerve
Cricothyroid muscle - supplied by the external branch of the superior laryngeal nerve |
|
|
Thyroarytenoid muscle
What is the origin and insertion? |
Origin: anterior interior surface of thyroid cartilage
Insertion: vocal process and anterior surface of the arytenoid |
|
|
Thyroarytenoid muscle
What are the lateral and medial portions? |
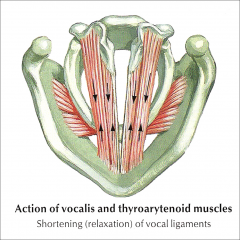
Lateral portion is just called the lateral thyroarytenoid muscle, which adducts the vocal fold.
Medial portion is the vocalis muscle, which controls length, tension and stiffness. |
|
|
Lateral cricoarytenoid muscle
What is the origin and insertion? |
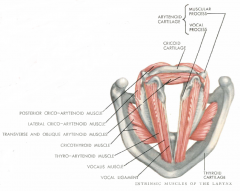
Origin: lateral cricoid arch
Insertion: muscular process of arytenoid cartilage |
|
|
Lateral cricoarytenoid muscle
What is the action? |
Pulls the muscular process anterior, which rotates the arytenoid so that the vocal process (with attached vacalis and thyroarytenoid muscles) move inward and down
|
|
|
What is the only unpaired muscle in the larynx?
What is it's action? |
Interarytenoid muscle (including transverse or oblique arytenoid fibers)
- connects the two arytenoid muscles = adduction - transverse fibers assist in closing the posterior glottis - Oblique fibers constrict the layngeal inlet |
|
|
Which muscle lies in the free edge of the aryepiglottic fold?
|
aryepiglottic muscle
|
|
|
What is the ONLY abductor muscle of the larynx?
|
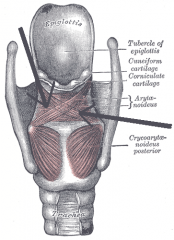
Posterior cricoarytenoid muscle
|
|
|
Posterior cricoarytenoid muscle
What is the original and insertion? |
Origin: posterior cricoid lamina
Insertion: muscular process of the arytenoid cartilage |
|
|
Posterior cricoarytenoid muscle
What is it's action? |
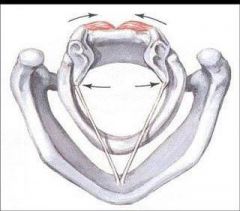
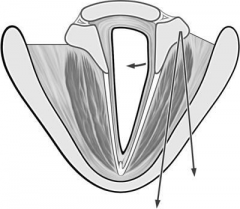
Two compartments: medial (transverse) & lateral (oblique)
Actions: the only abductor in the larynx - pulls muscular process down and back to rotate arytenoid so that vocalis process moves up and out - Co-contracts with adductor muscles during phonation |
|
|
Cricothyroid muscle
What is the origin and insertion? |
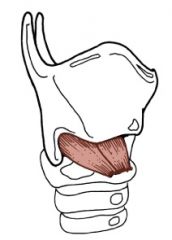
Origin: anterior arch of the cricoid cartilage
Insertion: thyroid cartilage |
|
|
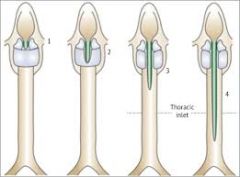
Cricothyroid muscle
What is the action? |
Closes the cricothyroid space and increases the distance between the anterior commissure and the posterior cricoid
Increases length and tension in vocal fold |
|
|
What are the following boundaries of the laryngeal vestibule?
Anterior: Posterior: Lateral: |
Laryngeal vestibule: from the inlet of the larynx to the edges of the false vocal folds
Anterior: posterior surface of the epiglottis Posterior: interarytenoid area Lateral: false vocal folds |
|
|
What are the laryngeal ventricles?
|
aka ventricles of Morgagni - a deep recess between the false and true vocal folds
- saccule is a conical pouch that ascends from the anterior part of the ventricle - numerous minor salivary glands open into the ventricle |
|
|
When are the times that the glottis closes completely?
|
During swallowing, valsalva and cough
|
|
|
How would you describe the location of the pyriform fossa/sinus?
|
It's a pharyngeal recess within the thyroid lamina but lateral to paraglottic space
|
|
|
What are the three divisions of the larynx?
|
Supraglottis
Glottis Subglottis |
|
|
What are the borders of the supraglottis?
|
From the tip of the epiglottis to the beginning of squamous epithelium at the jnct between the lateral wall and the floor of the ventricle (above the true VC)
|
|
|
What are the borders of the glottis?
|
The true vocal folds and the posterior commissure
Membranous vocal fold - from ant commissure to vocal process of arytenoid - composed of soft tissues: vocal ligament, muscle and the vocal cover - from ant commisure to the vocal process of the arytenoid cartilage - these structures vibrate to preduce the voice Cartilaginous vocal fold - arytenoid cartilages Posterior commissure - mucosa and the interarytenoid muscle |
|
|
What are the borders of the subglottis?
|
from undersurface of the true vocal folds to the inferior cricoid edge
|
|
|
The paraglottic space is located between which structures?
|
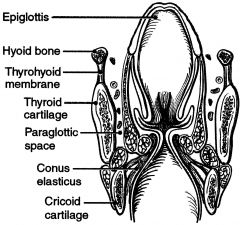
thyroid ala, conus elasticus and quadrangular membrane
|
|
|
The pre-epiglottic space is bounded by which structures?
|
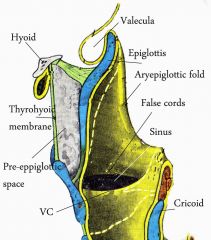
vallecula, thyroid cartilage, thyrohyoid membrane, and epiglottis
|
|
|
What kind of epithelium is there in the larynx?
|
Stratified squamous epithelium over vocal folds and upper vestibule
Ciliated columnar epithelium elsewhere |
|
|
What are the layers of the membranous vocal fold from superficial to deep?
|
Epithelium
Superficial lamina propria Intermediate layer lamina propria Deep layer lamina propria Conus elasticus Vocalis muscle |
|
|
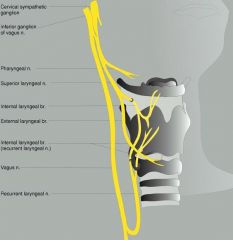
What are the two main branches of vagus nerve?
|
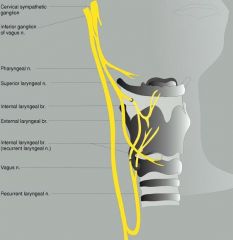
Superior laryngeal nerve
Recurrent laryngeal nerve |
|
|
What are the two branches of the superior laryngeal nerve and what do they supply?
|
Internal (SENSORY) branch pierces thyrohyoid membrane and carried afferent sensation from the larynx at and above the glottis. No muscle innervation.
The external (motor) branch supplies cricothyroid muscle. |
|
|
What does the recurrent laryngeal nerve supply?
|
Motor innervation to all pisilateral intrinsic laryngeal muscles except cricothyroid (external branch of SLN)
- interarytenoid muscle receives bilateral innervation |
|
|
On both sides, the RLN enters the larynx near the _______________________-
|
cricothyroid joint
|
|
|
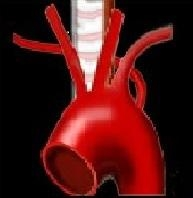
On the right side, the recurrent laryngeal loops around what? How about on the left?
|
Right - around subclavian artery
Left - around ligamentum arteriosum |
|
|
Nonrecurrent RLN is associated with what?
|
Anomalous retroesophageal subclavian artery
|
|
|
Which nerve connects the SLN and RLN?
|
Nerve of Galen (ramus communicans) or aka laryngeal nerve
|
|
|
What is the arterial blood supply to the larynx?
|
Superior laryngeal artery - arises from the superior thyroid artery (branch of ECA)
Inferior thyroid artery - arises from the thyrocervical trunk |
|
|
What is the venous blood supply from the larynx?
|
Superior thyroid vein - drains into internal jugular vein
Inferior thyroid vein - drains into the innominate vein |
|
|
What is the lymphatic drainage of the larynx?
|
Supraglottic lymphatics drain to upper jugular LN, some cross over
Infraglottic lymphatics drain to pretracheal or lower jugular nodes with some crossover Glottic lymphatic drainage is very sparse drinage, and only ipsilateral. |
|
|
Why does ossification of the hyoid bone begin and finish?
|
Begins after birth in six centers, and finished by 2 yrs of age
|
|
|
Explain the mechanism of phonation
|
Exhaled air increases subglottic pressure to push vocal folds apart
Airflow through glottis creates negative pressure, pulling vocal folds back together (Bernoulli effect) Myoelastic forces also pull the vocal folds back together Cycle begins again as glottis closes |
|
|
Atrophy of what part of the vocal cord may cause decreased vocal fold bulk?
|
Vocalis muscle - may become atrophic with aging, neuropathy and disuse
|
|
|
List some common causes of acute laryngitis?
|
URI - laryngeal inflammation usually due to cough, not direct infxn (forceful closure can result in interarytenoid edema)
Vocal abuse - due to tight closure = interarytenoid edema GERD - due to direct irritation of posterior glottis Often a combination of all of the above Interarytenoid edema limits glottic closure = voice may be rough, weak or breath and increased adductor effort is required to speak. |
|
|
List symptomatic and supportive treatments for acute laryngitis
|
Vocal hygiene - absolute silence not required
Hydration Decongestant for nasal obstruction Cough suppression Mycolytic Avoid drying antihistamines H2 blockers or PPI's if acid reflux suspect Steroids only for urgent need to use voice (performance). Steroids mask symptoms, therefore performers should be monitored closely to detect injury due to overuse. |
|
|
What do vocal nodules present like when looking at the vocal cords?
|
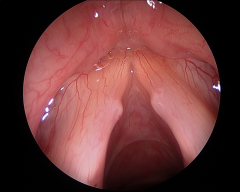
Usually symmetric swelling or masses of the middle portion of the membranous vocal fold
|
|
|
What is the cornerstone of tx of vocal nodules?
|
Voice therapy (not just voice rest) - need to correct vocal habits
- occasionally early surgical removal may be recommended - tx decisions should be based on vocal function, NOT appearance |
|
|
What is the histology of a vocal fold polyp?
|

Out-pouching of mucosa, distended by edema and loose stroma
|
|
|
What is the etiology of a vocal polyp?
|
Unknown, sometimes due to resolving hematoma
|
|
|
What is the primary sx of a vocal fold polyp?
|
hoarseness
|
|
|
What is the tx of a vocal fold polyp?
|
Voice therapy - polyps do NOT regress, but voice may improve
Surgery - excision via direct microlaryngoscopy |
|
|
What are the causes of laryngeal ulcers and granulomas?
|

Vocal abuse
Throat clearing Intubation GERD |
|
|
Is surgery used for laryngeal granuloma's?
|

Only for symptomatic lesions which do not respond to medical therapy, or when a tumor or other pathology is suspected. Recurrence rate very high and are more recalcitrant than original lesions.
|
|
|
What are vocal cysts?
|

Vocal cysts - epithelial lined spaced; may be mucus retention or epidermoid
|
|
|
How are vocal cysts tx?
|
Direct laryngoscopy and microsurgical excision
-Hoarseness may persist or be worse, due to scarring or persistent deficiency -Pt must be counseled about this risk and surgery must be carefully considered |
|
|
What are vocal sulci? What are the two types?
|

Vocal sulci - depression in mucosa of vocal fold edge. Two types:
- epithelial lined pocked (Z could be a ruptured cyst) - area of deficient lamina propria |
|
|
How are vocal sulci treated?
|
Unreliable outcome of surgery
Approaches include excision, collagen or steroid injection, mucosa "slicing" technique, or mucosal elevation with submucosal grafting. |
|
|
Describe etiologies of keratosis and leukoplakia of laryngeal mucosa
|

They are premaligantn epithelial lesions of laryngeal mucosa
Etiologies include smoking, vocal abuse, chronic laryngitis, GERD and vitamin deficiencies. |
|
|
How do you diagnose laryngeal keratosis and leukoplakia, and what is the tx?
|
Diagnosis requires biopsy, but a trial of conservative measures may be indicated if malignancy is not strongly suspected.
Treatment may be conservative with cessation of smoking, antireflux therapy and voice therapy. May also perform a direct microlaryngoscopy with excisional biopsy. |
|
|
What are laryngoceles and what are the two types?
|

Laryngoceles are dilation of the appendix of the ventricle, filled with air or fluid.
- Internal laryngocele - totally within the thyroid cartilage framework - External laryngocele - extends through the thyrohyoid membrane - May get combined lesions with dilations in both areas |
|
|
List etiologies of laryngoceles
|
- Increased intrapharyngeal pressure (glass blowers and wind instrument players)
- Idiopathic |
|
|
How do laryngocele's present?
|
- Hoarseness
- External laryngocele presents as swelling in the neck that may increase in size with "puffing" maneuvers |
|
|
How do you treat both types of laryngoceles?
|
Internal laryngoceles - endoscopic marsupialization
External laryngoceles or recurrent - external approach |
|
|
What are the early and late signs of laryngeal papillomatosis?
|
Early sign - hoarseness
Late signs - stridor and dyspnea |
|
|
List some treatment options for laryngeal papillomatosis
|
1) Suspension microlaryngoscopy and excision using microdebrider or CO2 laser, or microsurgical instruments
2) Office-based endoscopic procedures with local anesthesia can be used 3) Cryotherapy 4) Photodynamic therapy 5) Injection of antiviral agents (cidofovir) |
|
|
Why is tracheotomy typically avoided in pt's with laryngal papillomatosis?
|
Has been associated with subglottic and tracheal spread of lesion
|
|
|
What are the presentations of laryngeal chondroma?
|
Hoarseness, dyspnea, dysphagia, and globus sensation
More common in men than women Most frequent site is posterior plate of the cricoid cartilage, followed by thyroid, arytenoid and epiglottis |
|
|
How do you diagnose and tx laryngeal chondromas?
|
Dx - submucosal mass may be seen on mirror examination or office endoscopy, but is often only apparent on CT scanning
Tx - surgical excision; thyrotomy for anterior tumors, and lateral approach for other areas. Recurrence common. |
|
|
What are the presentations of unilateral and bilateral laryngeal paralysis?
|
Sx vary greatly
Unilateral paralysis 1) No Sx - immobile vocal fold noted during routine exam 2) Most often, hoarseness due to inadequate glottal closure during phonation 3) Occasionally, aspiration during swallowing Bilateral paralysis 1) Weak voice 2) Stidor |
|
|
What is the percentage of cases of laryngeal paralysis that are idiopathic?
|
about 20% of cases
|
|
|
Does regenerated or repaired nerve restore motion to the vocal folds?
|
Typically no
|
|
|
Why does regenerating RLN still causes vocal folds to lie in the paramedian position?
|
Regenerating RLN preferenially reinnervates the ADductor muscles, so there is inadequate posterior cricoarytenoid muscle force for abduction
|
|
|
In what position doe the vocal folds lie if they are completely denervated (central or high vagus nerve injury)?
|
Flaccid and lies in lateral, cadaveric position
|
|
|
Immediately after nerve injury, in what position do the vocal folds lie?
|
It depends, sometimes they may be lie lateral and shift to paramedian position over a few months
|
|
|
List some treatment options for unilateral vocal fold paralysis
|
Voice therapy
Injection laryngoplasty Type I thyroplasty (permanent medialization laryngoplasty) Arytenoid adduction Laryngeal reinnervation |
|
|
Give a little info on the following vocal fold injectable substances:
- Teflon injection - Gelfoam - Autologous fat - Commercial substances |
Teflon - was the most widespread tx through the 1970's but no longer used as granulomas eventually developed
Gelfoam - temporary, off-label tx, effective for 8-10 weeks and indicated when recovery is expected within a short time Autologous fat - harvested by liposuction or excision. Unpredictable survival--sometimes dissipates within a short time, but may survive for yrs Commercial substances - hydroxyapatite, collagen, etc - may persist for months to years. |
|
|
What is a type I thyroplasty?
|

Vocal fold is medialized by permanent implant placed in paraglottic space, via a window in thyroid cartilage
- usually performed under local anesthesia, so that results can be monitored during the procedure NOT effective in pts with flaccid paralysis and a large, posterior gap, or with vocal processes on different levels |
|
|
Describe the arytenoid adduction procedure
|
Suture through muscular process is passed through anterior thyroid cartilage, and traction applied to rotate arytenoid internally.
Indications - large glottal gap, vocal processes on different levels, aspiration. May be performed in combination with injection or thyroplasty. |
|
|
Describe laryngeal reinnervation procedure for vocal fold paralysis
|
Most commonly, a branch of the ansa cervicalis is anastomosed to the distal recurrent laryngeal nerve.
An alternate approach is to use a neuromuscular pedicle. Reinnervation by either technique is reported to restore bulk and tone to the reinnervated muscles, but not functional motion. It is less effective in patients over the age of 51. |
|
|
List treatments for bilateral vocal fold paralysis
|
1) Tracheotomy = gold standard
2) Arytenoidectomy - external or endoscopic, and total, medial or subtotal 3) Endoscopic cordotomy, cordectomy, or suture lateralization 4) Arytenoid abduction by external approach 5) Reinnervation dos not restore abductor function 6) Laryngeal "pacing" with an implantable stimulator is still experimental |
|
|
What is the pathophys and etiology of spasmodic dysphonia
|
Spasmodic dysphonia is intermittent involuntary spasms of intrinsic laryngeal muscles during speech
Etiology is unknown |
|
|
What are the two forms of spasmodic dysphonia?
|
Adductor form
- most frequent form - strained and strangled voice with frequent voice breaks - Breaks commonly occur at onset of words beginning with vowels (ie, "---eggs") Adductor form - About 1 in 10 pts with SD - Whispering or breathy voice - Voice breaks between plosive consonants and vowels (ie. "pu--pp--y") |
|
|
What is the most common tx used for adductor SD?
|
Botulinum toxin injection
- very small amounts are injected to weaken but not paralyze the vocal fold (may be used for adbductor SD, but less effective; toxin injected into posterior cricroarytenoid muscle) |
|
|
What is the "Berke" procedure for spasmotic dysphonia?
|
aka Selective Laryngeal Adductor Denervation-Reinnervation (SLAD-R), described by Dr. Berke
- transects adductor branches of the RLNs and reinnervates with branches of the ansa cervicalis |
|
|
Does a cuffed trach tube prevent aspiration?
|
No, but allows for suctioning and may decrease amount of material reaching lungs
|
|
|
List some procedures aimed at pts with dysphagia with severe aspiration
|
1) Tracheotomy
2) Surgical separation of the larynx and trachea and creation of a tracheostomy 3) Epiglottic flap to arytenoids 4) Lindeman's tracheoesophageal diversion procedure with proximal trachea to esophagus anastomosis and creation of a distal permanent tracheostoma. 5) Suturing vocal folds together via a laryngofissue. Theoretically a reversible procedure. 6) Total laryngectomy |
|
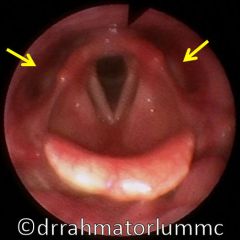
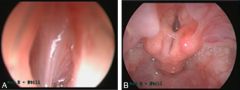
What is the dx?
What is the tx? |
Laryngeal candidasis
- Tx - need systemic antifungal tx. Topical and swallowed nystatin is ineffective - withhold steroids (especially if inhaled) |
|

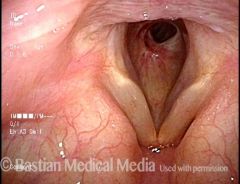
Pt has dyspnea. What is the dx?
|
Epiglottitis (infectious inflammation and edema of the supraglottis)
|
|
|
List the possible infectious etiologies of croup
|
Parainfluenza virus types 1 to 4
H. influenza Streptococci Staphylococci Pneumococci |
|

Pt has dyspnea. What is the dx?
|
Croup - "steeple" sign
|
|
|
What are some agents causing bacterial tracheitis?
What are sx of bacterial tracheitis? |
Staph & Strep
High fever, stridor and sx of severe croup |
|
|
What does the tracheal look like on its visualization in a pt with bacterial tracheitis?
|

Purulent racheitis, with obstruction due to edema and sloughed necrotic mucosa and mucus casts
|
|
|
What is the incidence of laryngeal involvement in pts with Hansen's disease
|
Hansen's dz = Leprosy (Mycobacterium leprae)
- Involves larynx in 10% of cases |
|
|
Which mycotic infections affect the larynx?
|
Blastomycosis (Blastomyces dermatitidis) and Histoplasmosis (Histoplasma capsulatum)
- tx both with Amphotericin B |
|
|
Pt has granulomas through out the body and are also seen as pale submucosal masses in the epiglottis and larynx. What is the likely diagnosis?
|
Sarcoidosis (dx by biopsy)
|
|
|
How do you diagnose RA as the cause of laryngeal pathology?
|
Rheumatoid arthritis may cause inflammatory fixation of the cricoarytenoid join and/or inflammatory nodules on the volca fold.
Serology - elevated ESR, rheumatoid factor, decreased complement levels and abnormal lupus panel Can get a high-resolution CT scan demonstrating erosion of join and soft tissue swelling |
|
|
How is the larynx affected in pt's with Wegener's granulomatosis?
|
WG affects primarily the lung and kidneys but larynx is affected up to 25% of the time.
Exophytic granulation tissue that often progresses to subglottic stenosis. - biopsy will show necrotizing granulomas and capillary thrombosis - ANA may be positive, but cANCA is more sensitive |
|
|
What are the tx options for relapsing polychondritis?
|
Medical - steroids, dapsone, azathioprine, cyclophosphamide, cyclosporine, penicillimine, and plasma exchange
Surgery - is ineffective; airway dz can progress to death from PNA or obstructive respiratory failure |
|
|
What is the tx for pemphigus and pemphigoid?
|
Dapsone, steroids and azathiaprine
|
|
|
What is the typical head & neck presentation of pemphigus and pemphigoid?
|
Mouth and throat pain and hoarseness
Both disorders usually begin with mouth ulcers that can spread as far caudal as the larynx, but do not involve the subglottis or trachea |
|
|
What is the head & neck presentation of amyloidosis?
|

Hoarseness, stridor, globus and dysphagus
Diagnosis is based on laryngeal examination showing waxy lesions that may be gray or orange, typically on the epiglottis, but sometimes glottic or subglottic. |
|
|
What will the biopsy of a lesion suspected to be due to amyloidosis look like?
|
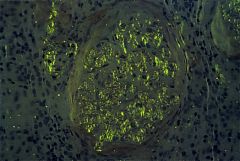
Histology stained with hematoxylin and eosin is nonspecific.
Specimens should be processed with Congo red stain and viewed under polarized light to show apple green birefringence |
|
|
What is the tx of laryngeal amyloidosis?
|
Endoscopic excision or open surgery to remove or debulk symptomatic lesions
Total removal often impossible with frequent recurrence Tracheotomy may be required |
|
|
How do you manage acute airway distress secondary to blunt laryngeal trauma?
|
1) Proceed directly to OR for trach with local anesthesia, followed by direct laryngoscopy under general anesthesia to assess injury
2) Orotracheal intubation not erecomended due to laryngeal distortion and tube may create a false passage |
|
|
How is blunt trauma to the larynx be managed surgically?
|
A midline thyrotomy is used to expose laryngeal mucosa. All lacerations should be carefully sutured. Local flaps or free mucosal grafts may be used to close defects.
If an arytenoid cartilage is completely avulsed and displaced, it is better to remove it than attempt to reposition it. |
|
|
How are laryngeal cartilage fractures managed?
|
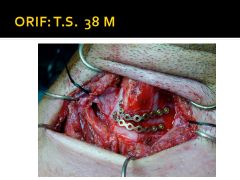
Should be reduced and immobilized with plates if necessary.
Laryngeal stents may be used to add stability, but can stimulate granulation tissue. |
|
|
What are the etiologies of laryngeal/tracheal stenosis?
|
Intubation
External injury Systemic disease Acid reflux Idiopathic |
|
|
What is the most common cause of neonatal stridor?
|

Laryngomalacia - supraglottis is flaccid, and epiglottis or interarytenoid tissue collapse during inspiration to obstruct the airway
|
|
|
What is the etiology of laryngomalacia?
|
Unknown, probably neurologic or structural immaturity
|
|
|
What are the three types of laryngomalacia?
|
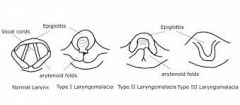
Type 1 - foreshortened or tight aryepiglottic folds
Type 2 - redundant tissue in the supraglottic Type 3 - posterior epiglottic collapse due to underlying neuromuscular disorders |
|
|
What is the typical presentation of laryngomalacia?
|
Stridor is noted soon after birth
Breathing is better in prone position rather than supine |
|
|
How do you diagnose laryngomalacia?
|
Flexibile endoscopy in the office
"omega" shaped epiglottis Epiglottis falls backwards during inspiration |
|
|
What is the typical tx for laryngomalacia?
|
Usually obs and assurance that this will resolve by 12-16 months
Endoscopic epiglottoplasty for severe stridor or failure to thrive Trachotomy may be required |
|
|
What is the second most common cause of newborn stridor?
|
Laryngeal paralysis
|
|
|
List the causes of laryngeal paralysis in a newborn
|
1) Idiopathic
2) Birth trauma 3) Cardiomegaly 4) Arnold-Chiari malformation 5) Ligation of persistent ductus arteriosis (usually unilateral, but may be bilateral) |
|
|
What is the tx of a laryngeal hemangioma?
|
Natural history is expansion for several months followed by involution, so may just observe.
- Systemic steroids and racemic epinephrine for acute stridor - Systemic propranolol can result in dramatic involution - CO2 laser excision, external excision, or tracheotomy if obstruction does not respond to propranolol. |
|
|
What are laryngeal webs and atresia?
|
A congenital band over part (web) and all (atresia) of the glottis
|
|
|
What is the tx for laryngeal webs and atresia?
|
Tracheotomy for relief of airway obstruction
Web is best corrected when child is larger and anatomy is more distinct Successful division of web may not improve the voice |
|
|
What is the tx for congenital subglottic stenosis?
|
Tx - tracheotomy, cricoid split or laryngotracheal reconstruction
(may be congenital, or secondary to intubation) |
|
|
What is the cause of laryngeal clefts?
|
Rare anomaly caused by incomplete fusion of the laryngotracheal septum
|
|
|
What is the presentation of laryngeal clefts?
|
Cyanosis with feeding, stridor, recurrent pneumonia. Severity due to extent of cleft.
|
|
|
What is the tx of laryngeal clefts?
|
Some can be observed and will eventually improve, others require repair by endoscopic or open rapair
|
|
|
When should the first trach change be performed, and why not done it earlier?
|
Typically no earlier than day 5. Study of 46 institutions demonstrated mean first trach change at 5.3 days. New study recommends 7-14 days.
Not done earlier to prevent reentry into false passage, and there's really no need to change it earlier. |
|
|
List the immediate complications of tracheotomy
|
Bleeding
Pneumothorax Pneumomediastinum Subcutaneous emphysema Dislodged or obstructed tube False passage with tube outside trachea Postobstructive pulmonary edema Apnea due to loss of hypoxic drive Tube too short or inappropriate shape (esp in morbidly obese pts) |
|
|
List the delayed complications of tracheotomy
|
Granulation tissue
Stomal infection Subglottic or tracheal stenosis Tracheomalacia Tracheoesophageal fistula Displacement of tube Tracheoinnominate fistula Persisting tracheocutaneous fistula after decannulation |

