![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
List four respiratory events, in degree of severity, that encompass sleep-disordered breathing (SDB).
|
- Snoring
- Upper airway resistance syndrome - Obstructive sleep apnea syndrome - Obesity-Hypoventilation syndrome |
|
|
What is the difference between snoring and upper airway resistance syndrome?
|
Snoring - nonapneic snoring is very common, and does not have to be associated with arousals or sleep fragmentation.
Upper airway resistance syndrome - events that do not qualify as apneas or hypopneas, but DO lead to arousals, sleep fragmentation, and excessive daytime sleepiness |
|
|
What classifies a respiratory event?
|
Apneic or hypopneic events last a minimum of 10 seconds and are associated with oxygen desaturations and brief arousals from sleep.
|
|
|
How many minimal scorable respiratory events per hour are needed on a polysomnogram to diagnose OSA?
What is the ranking? |
Normal - < 5 events per hour
Mild - 5-15 events Mod - 15-30 events Severe - >30 events |
|
|
Which stage of sleep do humans spend the most time in?
|
Stage 2
|
|
|
How many minutes does it take for a cycle of sleep to complete?
|
~ 90-120 minutes
|
|
|
Respiratory events (apneas or hyponeas) are LESS likely to occur in which stage of sleep?
|
Stage 3 (more likely to occur in stages 1, 2 & REM)
|
|
|
List the medical consequences of OSAS
|
- HTN
- Arrhythmias - MI - Strokes - Pulm HTN - CHF |
|
|
What is the pathophys of HTN in OSAS?
|
Most likely related to the increased sympatheic tone from hypoxemia and frequent arousals seen in OSAS.
During an apneic event there is decreased CO, increased SNS activation, and increased SVR. On resolution of the apneic episode, there is increased venous return to the right side of the heart leading to an increased CO against the increased vascular resistance. This causes an abrupt increased in BP. |
|
|
What is the pathophys of cardiovascular disease in OSAS?
|
Recurrent apneas can cause acute thrombotic events, secondary to an increased in platelet activation, and chronic atherosclerosis. A depletion of myocardial oxygen sypply during apneic events can lead to acute ischemia.
|
|
|
What is the pathophys of CHF in OSAS?
|
Can worsen CHF by increasing afterload (d/t increased SVR) on an already failing heart leading to reduced cardiac output. In addition, the released of catecholamines from the apneic events (d/t increased SNS) contributes to worsening cardiac function)
|
|
|
Which cardiac arrhythmias are most often seen in OSAS?
|
Bradytachyarrhythmias
Bradycardia starts at the cessation of respiration, followed by tachycardia at the resumption of respiration. |
|
|
What is the pathophys of strokes in OSAS?
|
During the apneic event there is a decrease in systemic pressure and increase in intracranial pressure leading to a decrease in cerebral perfusion. This decrease in cerebral perfusion increases the chance for an ischemic event.
In addition, an increase in atherosclerotic changes to the endothelium and increased risk of thrombotic events can also be seen from the fluctuations in cerebral blood flow, as seen in the cardiac vasculature. |
|
|
Name 2 questionnaires used to obtain a subjective assessment of excessive daytime sleepiness.
|
Epworth Sleepiness Scale (asks pt to rate the likelihood of dozing off in eight scenarios, on a scale of 0-3)
Functional Outcomes of Sleep Questionnaire |
|
|
What are the classes of dental occlusion?
|
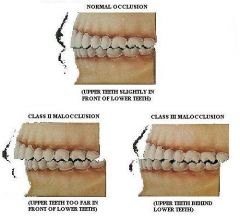
Class I - normal bite
Class II - overbite Class III - underbite |
|
|
What's the difference between Mallampati & Friedman classifications?
|
Mallampati has the pt open their mouth wide and protrude the tongue
Friedman has the pt open their mouth wide with the tongue in a neutral position |
|
|
What are the four levels of polysomnography?
|
Level 1 (standard PSG)
- Full attended in-laboratory polysomnography - >7 channels with sleep staging Level 2 - Full UNattended portable polysomnography - usually in pt's home - >7 channels with sleep staging Level 3 - Portable, UNattended sleep apnea monitors (AASM recommendation for HST) - 3 channels, no sleep staging (HR, air flow, oximetry) Level 4 - Limited unattended monitors - 1-2 channels, no sleep staging NOTE: Stages 3-4 DO NOT measure sleep time |
|
|
What are some behavioral modifications in OSAS?
|
Reduce alcohol use
Weight loss Change in sleeping position |
|
|
Effective CPAP compliance is considered to be at least __ hours of usage, five nights a week.
|
4 hours
|
|
|
What is an Auto-PAP machine?
|
Automatic positive airway pressure is a unit that adjusts and delivers variable CPAP pressures with each respiratory cycle based on changes detected in airflow pressures, resistance or snoring intensity. May be a substitute for a CPAP titration study.
|
|
|
How can you help a patient overcome the claustrophobic feeling associated with wearing a CPAP mask?
|
most sleep laboratories offer CPAP desensitization clinics
|
|
|
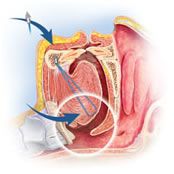
How do oral appliances typically work?
|

Work by bringing the mandible and base of tongue forward and stabilize the mandible to prevent it from falling open during sleep.
|
|
|
What is the name of a nasal device that is FDA approved for OSAS?
How does it work? |

Provent
Uses a valve design that attaches over the nares with an adhesive. On INspiration - valve opens, allowing the user to breath freely On EXpiration - valve closes, increasing pressure in the airway (expiratory positive airway pressure) which maintains patency of the upper airway until the start of the next inhalation |
|
|
List the various palatopharyngeal procedures aimed at OSAS
|
UPPP
Transpalatal advancement pharyngoplasty Expansion sphincterplasty Uvulopalatal flap Laser-assisted uvulopalatoplasty (LAUP) Cautery-assisted palatal stiffening (CAPSO) Radiofrequency ablation of soft palate Palatal implants Injection snoreplasty |
|
|
What is the success rate of UPPP in eliminating OSAS?
|
40-50%
|
|
|
Describe transpalatal advancement pharyngoplasty technique for OSAS
|
Involved removing a portion of the posterior edge of the hard palate and advancing the soft palate anteriorly.
This results in enlargement of the posterior oropharyngeal airway w/o resection of soft tissue. |
|
|
Describe the uvulopalatal flap procedure for OSAS
What are the advantages vs UPPP? |
Variation of the UPPP; rather than resecting palatal & uvular tissue, this advancement flap involves sutuing the uvula and distal soft palatal tissue upward onto the soft palate, after demucosalization of opposing surfaces.
Advantages of this procedure are that it is reversible in the immediate post-operative period should the pt develop VPI symptoms; less post-op pain Contraindicated in pts with excessively long or thick palates or uvulas |
|
|
What is the primary use of the laser-assisted uvulopalatoplasty?
|
Snoring (reported 80-85% success rate)
It's use in upper airway resistance syndrome (UARS) and OSAS is more controversial |
|
|
Describe the laser-assisted uvulopalatoplasty procedure?
|
Usually done in the office setting under local anesthesia
Using a CO2 laser, two vertical cuts are made in the soft palate on either side of the uvula, and the lower two-thirds to three-fourths of the uvula is amputated and the cut edge of the uvula is "fish mouthed" with the laser to allow further retraction during healing. As these cuts heal, scar retraction and stiffening of the palate are achieved. |
|
|
Describe cautery-assisted palatal stiffening (CAPSO) procedure for OSAS
|
Office-based procedure that uses a standard electrocautery unit to remove the mucosa off the midline of the soft palate, inducing scar tissue that results in a stiffer palate.
|
|
|
Describe the radiofrequency ablation of soft palate procedure for OSAS
|
Office-based procedure performed with local anesthesia. uses low-temp energy delivered into the tissue of the soft palate via a needle. The resulting submucosal coagulation necrosis causes scarring and contraction of the tissue resulting in a shorter and stiffer soft palate.
3-4 sites are ablated. |
|
|
Describe the palatal implant procedure for OSAS
|

The Pillar System , used for snoring and mild OSAS, utilizes polyethylene terephthalate implants that measure 18mmx2mm.
Three implants are injected submucosally into the soft palate using a commercially available handpiece. The implant and assocaited scarring result in stiffening of the palate. |
|
|
Describe the injection snoreplasty procedure for OSAS
|
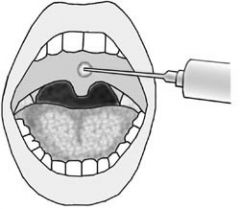
Simple and inexpensive office-based procedure for snoring.
Involves injecting a sclerosing agent into the midline of the soft palate, using a needle and syringe. Agents used include alcohol or sodium tetradecyl sulfate. |
|
|
List the hypopharyngeal procedures used for OSAS
|
Radiofrequency ablation of tongue base
Genioglossus advancement Hyoid suspension Tongue suspension Transoral midline glossectomy Mandibular advancement Maxillomandibular advancement |
|
|
Describe the radiofrequency ablation of tongue base used for OSAS
|
Radiofrequency ablation used to reduce tissue volume at the base of the tongue.
Four lesions are created at or anterior to the circumvallate papilla; multiple treatment sessions may be required. Potential complications may include abscess, ulceration, alteration of taste, or tongue paralysis if performed too close to the hypoglossal nerve. |
|
|
Describe the genioglossus advancement procedure used for OSAS
|
Results in a more anteriorly positioned tongue with increased tension. This helps keep the hypopharyngeal airway patent during sleep when there is muscle atonia.
Initially described as a horizontal inferior sagittal osteotomy, it was later modified to a rectangular geniotubercle osteotomy which advances only the geniotubercle in the anterior mandible where the genioglossus muscle attaches. Potential complications invlude dental root injury, mandible fracture, and hematoma of the tongue and floor of mouth. |
|
|
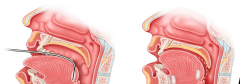
Describe the hyoid suspension procedure used for OSAS
|
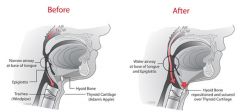
Hyoid bone is inferiorly positioned in pts with OSAS
Forward movement of the hyoid complex helps to open up the hypopharyngeal airway. Two techniques: Sutured to the Mandible - transecting the inferior hyoid muscles allows anterior and superior advancement where it can be sutured to the mandible Sutured to the Thyroid cartilage - transecting the superior hyoid muscles, it can be advanced and sutured to the thyroid cartilage |
|
|
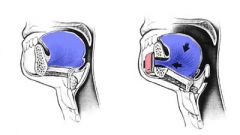
Describe the tongue suspension procedure used for OSAS
|
Using a commercially available system (Repose), a bone screw with an attached prolene suture is inserted into the mandible through the floor of the mouth. The suture is then passed submucosally from the floor of the mouth through the tongue and out the base. The suture is passed to the opposite side of the tongue, and then to the anterior floor of the mouth where it's secured to a screw seated in the mandible. Suture remained submucosal through entire course. Helps prevent backward collapse of the tongue during sleep.
|
|
|
Describe the transoral midline glossectomy procedure used for OSAS
|
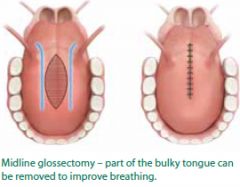
Resecting tissue from the base of the tongue in the midline may be done transorally using a CO2 laser, electrocautery, plasma knife, or traditional techniques (have seen this performed with the Devinci).
End result is volume reduction at the base of the tongue. Potential complications: bleeding from the lingual artery, hypoglossal nerve injury, hematoma, abscess, dysphagia and taste disturbance. |
|
|
Describe the mandibular advancement procedure used for OSAS
|

For pt's with retrognathia, mandibular advancement improves not only cosmetic appearance but helps to open the hypopharyngeal airway.
Performing bilateral sagittal osteotomies at the ramus allows the mandible to be advanced anteriorly and secured with plates. Similar to genioglossal tubercle advancement, this pulls the tongue anteriorly opening up the hypopharyngeal airway. |
|
|
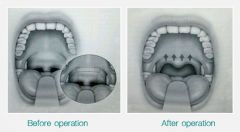
Describe the maxillomandibular advancement procedure used for OSAS
|
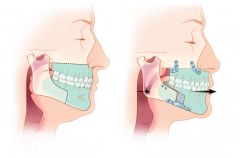
THE most effective surgical procedure for OSAS! (most successful is still trach)
Enlarges the pharyngeal and hypopharyngeal airway by expanding the skeletal framework. The maxilla and mandible are advanced by making osteotomies (LeFort 1 and bilateral sagittal mandibular osteotomies), and then fixed in the advanced location with plates. Usually reserved for pts who have documented BOT obstruction and have failed other upper airway procedures. |
|
|
In pt's undergoing a UPPP for mild to moderate OSA, a mandibular plane to hyoid of what distance has been associated with higher success?
|
Less than 21cm
|
|
|
Surgical success of OSA is often defined as at least a ___% reduction in AHI.
|
50%
|
|
|
What is the respiratory disturbance index (RDI)?
|
a similar measure to AHI, which refers to the number of times per hour that blood O2 saturation falls >3%
|

