![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
96 Cards in this Set
- Front
- Back
|
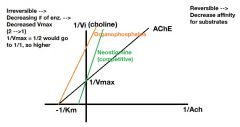
Put organophosphates and competitive inhibitors of AChE on a lineweaver-burk plot. |
|
|
|
What receptors antagonize each other in the heart?
|
beta1 and M2
|
|
|
What renin response would you see in a patient with a pheochromocytoma?
|
Decreased due to alpha1 stimulation. Alpha-receptors are less sensitive to activators than beta, but at higher doses they become predominant.
("It's like a safety valve. If you already have plenty alpha1 response to increase BP you don't need RAAS engaged") |
|
|
Beta2 receptors are mostly not innervated. What neurotransmitter(s) cannot reach this receptor?
|
NE. This is the receptor for E.
|
|
|
Beta2 receptors are coupled to what intracellular protein?
|
Gs, increasing cAMP.
|
|
|
What is the effect of epinephrine on the liver?
|
(1) Glycogenolysis
(2) Gluconeogenesis (3) Lipolysis |
|
|
Insulin secretion is slightly enhanced by ______________.
|
epinephrine
|
|
|
What is the result of alpha2 stimulation and beta2 stimulation in the pancreas?
|
Alpha2 - decreased
Beta2 - increased |
|
|
D1, just like beta2 will result in an increased intracellular __________.
|
cAMP
|
|
|
Why can dopamine bind to beta and alpha adrenergic receptors?
|
Remember dopamine has a similar molecular structure to norepinephrine, only differing by an hydroxyl group.
|
|
|
As you're titrating your patient with increasing dopamine dosages, what will happen?
|
You will go from D1 stimulation to beta1 stimulation to alpha1 stimulation.
|
|
|
What drug has a good clinical use in shock?
|
Dopamine. It dilates coronaries and renal vasculature (maintaining GFR), it increases cardiac output (beta1) and can help maintain BP (alpha1).
|
|
|
This is a D1 agonist used for severe HTN.
|
Fenoldopam
|
|
|
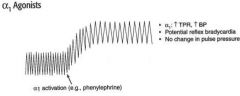
What BP tracing would you see with addition of phenylephrine?
|
|
|
|
Why should you think twice about administering phenylephrine systemically in a hypotensive patient?
|
It does increase BP, but increases the risk for ischemia and reflex bradycardia.
|
|
|
Mention two alpha1 agonists and their uses.
|
(1) Phenylephrine: Nasal decongestant and ophthalmologic use (mydriasis w/o cycloplegia)
(2) Methoxamine: Paroxysmal atrial tachycardia because of vagal reflex - Increased BP can cause a reflex bradycardia which slows down the heart. |
|
|
Alpha2 agonists are used clinically for what? How does it work?
|
Mild to moderate HTN. It stimulates prejunctional receptors in the CNS to decrease sympathetic outflow.
|
|
|
These two drugs are alpha 2 agonists.
|
Clonidine and methyldopa
|
|
|
How would a BP tracing look when administering beta agonists?
|

|
|
|
What is the drug that is a non-selective beta agonist?
|
Isoproterenol (iso = the same). Works equally on beta 1 and beta 2.
|
|
|
What is a clinical use of isoproterenol? What are side effects?
|
(1) Bronchospasms (asthmatic; beta 2)
(2) Heart block (beta 1) (3) Bradyarrhythmias (beta 1) Side effects will be those of tachycardia; angina, arrhythmia and flushing (beta 2) |
|
|
What is Dobutamine? What is it useful for?
|
beta-agonist. It is practically a beta 1 selective agonist, but with weak beta 2 agonistic properties.
Acute management of CHF. |
|
|
What drugs could be used in asthmatics?
|
Selective beta2 agonists:
(1) Salmeterol (2) Albuterol (3) Terbutaline |
|
|
This beta agonist is used to prevent premature labor.
|
Ritodrine, works on beta 2 (selective). It relaxes
|
|
|
Compare salmeterol with albuterol and terbutaline.
|
Salmeterol is slow acting, it is used for prophylaxis in asthmatics only.
Albuterol and terbutaline can be given in IV form to have an immediate effect in severe asthmatic attacks. |
|
|
What is a common complaint of anti-asthma drugs?
|
Beta2 agonists works just like epinephrine. It causes vasodilation that may cause reflex tachycardia.
|
|
|
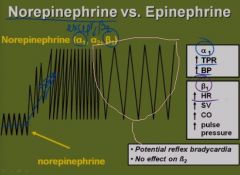
What adrenergic receptors do NE work on? E?
|
Everything except beta2 (not innervated). Epinephrine works on everything.
|
|
|
How would NE appear on a tracing?
|
|
|
|
NE CAN NEVER ___________________________.
|
LOWER BLOOD PRESSURE (no beta 2)
|
|
|
How would E appear on a tracing? (increasing doses)
|
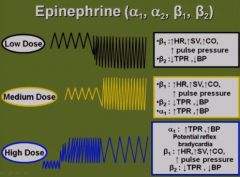
Low doses: Primarily beta activity
Medium doses: Alpha1 is poking its nose in the pharmacology. It looks like a beta 1 agonist. High dose: Alpha 1 predominates. BP increased. May see reflex bradycardia. |
|
|
What drug would look like medium dose epinephrine on a tracing?
|
Dobutamine (beta 1).
|
|
Is this E or NE?
|
We don't know. If we were told, however, that the drug bronchodilates, it would be E.
|
|
|
How do NE and E at high doses differ?
|
NE: Alpha1, Beta1
E: Alpha1, Beta1, Beta2 Leaving out alpha2 |
|
|
You have given too much epinephrine in a patient in shock. His BP is high and HR is progressively lower. What can be done?
|
Alpha 1 blocker (this is epinephrine reversal)
|
|
|
In too high doses E, we can reverse it by alpha-1 blockade by unmasking its beta-2 activity. How can we do the same with NE?
|
We can't. NE can never reach beta 2 receptors (has not beta2 activity).
|
|
|
What are uses of NE and E?
|
(1) Cardiac arrest (beta1)
(2) Adjunct to local anesthetic (prevent absorption) (3) Hypotension (alpha1, beta1) (4) Anaphylaxis (only E) (5) Asthma (only E) |
|
|
What are releasers?
|
Drugs that displace NE from its mobile pool in the nerve terminal.
|
|
|
Where are MAO-A enzymes found in the body?
|
Anywhere (A for Anywhere)
|
|
|
MAO-A inhibitors will prevent the metabolism of what exogenous compound? What happens?
|
Tyramine from wine and cheese. Tyramine causes a massive release of NE from the mobile pool. Extreme alpha1 (BP), beta 1 (tachycardias). This is called a HTN crisis, it will kill the patient.
|
|
|
A patient is on a MAO-A inhibitor. What must they avoid?
|
(1) Tyramine
(2) Ephedrine (3) Amphetamines They are releasers. |
|
|
A consequence of chronic cocaine use?
|
Dilated cardiomyopathy, potential for dying from MI or strokes.
|
|
|
What should you worry about when you give tricyclics?
|
Cardiotoxicity (it's a limiting side effect of these drugs)
|
|
|
Alpha receptor antagonism may cause ____________ and __________.
|
reflex tachycardia; salt and water retention
|
|
|
What else should you add to an alpha antagonist in the drug regimen in the treatment of hypertension?
|
Beta blocker (reflex tachycardia) and diuretic (RAAS may increase
|
|
|
Major uses of alpha antagonists?
|
(1) Hypertension
(2) Pheochromocytomas |
|
|
What is the drug of choice in a patient with pheochromocytoma? Explain your choice.
(1) Phentolamine (2) Phenoxybenzamine |
Phenoxybenxamine. It is an irreversible inhibitor and works noncompetitively. Phentolamine is a competitive inhibitor. This is a bad choice due to the extreme doses we would need to out-compete epinephrine.
|
|
|
How would you fit phenoxybenzamine and phentolamine in a graph with % TPR as a function of log dose of NE?
|
|
|
|
When would you give a beta blocker to a patient with a pheochromocytoma?
|
After phenoxybenzamine. If you do it before, you allow all the E to bind only to alpha1.
|
|
|
List these selective alpha 1 blockers.
|
(1) Prazosin
(2) Doxazosin (3) Terazosin (4) Tamsulosin |
|
|
Alpha 1 selective blockers are used for what?
|
(1) HTN
(2) Benign prostatic hyperplasia |
|
|
We use alpha 1 blockers in benign prostatic hyperplasia to allow for better voiding of the bladder. What can we do to actually decrease the size of the prostate?
|
Finasteride (5 alpha reductase inhibitor)
|
|
|
List alpha 2 blockers you know.
|
(1) Yohimbine
(2) Mirtazapine |
|
|
What drug could you give a woman with anorexia and depression?
|
Mirtazapine. Causes weight gain as well as treating depression by increasing NE in the brain.
|
|
|
Beta1 blockade results in what?
|
(1) Decreased HR, Decreased SV, Decreased CO
(2) Decreased Renin (3) Decreased aqueous humor production |
|
|
What are clinical uses of beta1 antagonists?
|
Heart: SVTs, Angina, MI
Kidney: HTN, CHF |
|
|
What is the rationale for use of beta blockers in HTN?
|
BP = TPR x CO
Renin secretion is decreased, decreasing angiotensin II and reducing TPR. Cardiac output is also decreased. |
|
|
A beta blocker in overdose will cause?
|
AV block. Could potentially stop the heart.
|
|
|
How can you reverse a beta blocker overdose?
|
Glucagon. It has positive inotropic and chronotropic effects on the heart that are G-protein linked to adenylyl cyclase.
|
|
|
Don't use this drug in these groups of patients unless you really have to. Explain why.
|
Beta blockers in asthmatics. Beta 2 blockade may precipitate bronchospasms.
Beta blockers may precipitate vasospasms in patients with vasospastic dx such as Raynauds or Prinzmetals angina. |
|
|
In prinzmetals angina you should not use? What could you use?
|
Don't use beta blockers. Use Calcium channel blockers or nitrates.
|
|
|
What can beta blockade result in other than bronchospasms in asthmatics and vasospasms in patients with vasospastic disorders?
|
Metabolic effects upon fasting. We need E's effect on beta 2. It can decreased glycogenolysis, decrease gluconeogenesis. Result is hypoglycemia.
|
|
|
What group of patients will be most affected by the metabolic side effects of beta 2 blockade?
|
Diabetics.
|
|
|
In what three groups of patients would you want to avoid using beta blockers?
|
(1) Asthmatics
(2) Vasospastic dx (3) Diabetics |
|
|
What do we really mean (in vivo) when saying that a drug is, for example, beta 1 selective?
|
Beta 1 > Beta 2
It's a matter of dose. |
|
|
Memory help: How can we easily remember what beta blockers are beta1-selective drugs?
|
If they start with letters A through M. From letters P and onwards you have beta non selective.
|
|
|
What does it mean that a drug have ISA?
|
Intrinsic Sympathomimetic Activity, it means that the drug has partial agonist activity (partial agonists have duality; by themselves they behave as agonists, in the presence of full agonists they behave as blockers)
|
|
|
These two beta blockers that have ISA?
|
(1) Acebutolol
(2) Pindolol |
|
|
What does it mean that certain beta blockers have a "ceiling" on their effect?
|
It means that they might be less effective, but they are also far less toxic.
|
|
|
List some properties of beta blockers with ISA.
|
(1) Act as partial agonists
(2) Less bradycardia (beta1) - Partial agonist activity (3) Slight vasodilation or bronchodilation (beta2) (4) Minimal change in plasma lipids (beta2) |
|
|
What beta blocker has ISA and is non-selective?
|
Pindolol
|
|
|
Blood lipids often increase with beta blockers. Why?
|
Lipolysis is impaired particularly in the liver.
|
|
|
These beta blockers have no issues with hyperlipidemia.
|
(1) Acebutolol
(2) Pindolol |
|
|
Atenolol is ________-soluble and does not produce _________.
|
water; sedation
|
|
|
What beta blockers produce sedation?
|
Acebutolol (+)
Metoprolol (+) Pindolol (+) Timolol (++) Propranolol (+++) |
|
|
Patient has hx of angina. They are treating insomnia with benzodiazepines. Which beta blocker will be safer to use?
|
Atenolol (no CNS depressant effect)
|
|
|
General uses of beta-blockers?
|
(1) Angina
(2) HTN (3) Post-MI |
|
|
Some beta-blockers are classified as antiarrhythmics. What class are they?
|
II
|
|
|
What beta blockers are approved as antiarrhytmics?
|
(1) Propranolol
(2) Acebutolol (3) Esmolol ("APE") |
|
|
These beta-blockers are used in glaucoma.
|
(1) Timolol
(2) Betaxolol |
|
|
Propranolol has some special uses since it penetrates the CNS. What is it?
|
(1) Migraine
(2) Thyrotoxicosis (3) Performance anxiety (4) Essential tremor |
|
|
Propranolol is the only beta blocker that inhibits __________.
|
deiodinase
|
|
|
What is special about Labetalol and Carvedilol?
|
They have combined alpha-1 and beta-blocking activity. Used in CHF.
|
|
|
How can we easily remember that Labetalol and Carvedilol have combined alpha and beta action?
|
They don't end in olol, but rather lol.
|
|
|
This beta blocker is also a class III antiarrhythmic.
|
Sotalol
|
|
|
What is special about sotalol?
|
It's a potassium channel blocker AND beta blocker. It has a use as antiarrhythmic (class III)
|
|
|
Glaucoma comes in two flavors, what are they?
|
(1) Open-angle glaucoma
(2) Closed-angle glaucoma |
|
|
What angle are we talking about in glaucoma?
|
The angle between the iris and the cornea
|
|
|
What is the problem in glaucoma and what happens?
|
Increased intraocular pressure which compromises the vascular supply to the retina. With hypoxic damage (fragile neural tissue) we can get blindness.
|
|
|
Describe open-angle glaucoma.
|
Chronic condition with IOP due to decreased reabsorption of aqueous humor, leading to progressive (painless) visual loss and, if left untreated, blindness.
|
|
|
Drug treatment of open-angle glaucoma?
|
Drug treatment: Beta blockers to decrease the formation of fluid by ciliary epithelial cells and muscarinic activators to improve drainage through the canal of Schlemm. Muscarinic agonists to improve outflow. AChE inhibitors improve outflow.
|
|
|
Describe closed-angle glaucoma.
|
Acute (painful) or chronic (genetic) condition with increased IOP due to blockade of the canal of Schlemm. When it's acute it's a matter of hours for us to decrease intraocular pressure using powerful diuretics, otherwise blindness will be the result.
|
|
|
What is latanoprost?
|
Prostaglandin analogue that will open the canals of schlemm.
|
|
|
Side effect of Latanoprost for glaucoma?
|
Darkening of the iris
|
|
|
Treatment of acute glaucoma attack?
|
Diuretics. Mannitol and short term treatment with carbonic anhydrase inhibitors.
|
|
|
_____________ (Miosis/Mydriasis) is a good idea in glaucoma.
|
Miosis
|
|
|
These drugs are contraindicated in treatment of glaucoma.
|
(1) Alpha1 agonists
(2) Muscarinic blockers Causes mydriasis. Can precipitate an acute attack in people with glaucoma and result in blindness. |

