![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
12 Cards in this Set
- Front
- Back
|
Wells Score
|
cancer tx <6 months- 1 pt
calf swelling >3 cm >contra 10 cm below tibial tub- 1pt whole leg swell- 1pt Collateral superficial veins- 1 pt Ipsi solo pitting edema- 1 pt Localized pain along DV- 1pt Paralysis, paresis, or recent cast- 1pt bedridden > 3 days, or surg<4wks- 1pt Alternative diagnosis at least as likely -- Subtract 2 points |
|
|
Virchow's triad
|
reduced flow
vas endoth injury hypercoag |
|
|
Hidradenitis
|
chronic follicular occlusive disease, insideous onset pub to 40yo, 3:1 f/m, obese.
Affects axilla & grossly perineal area b/n vagina (vs. granuloma inguinale), relapsing. Deep round lesions (vs. furuncles) to abcesses, comedones, and fibrosis. Scarring & induration (vs. follicular pyodermas) no GI hx (vs. Chrons) |
|

|
Hidradenitis in the axilla
|
|

|
Hidradenitis
|
|
|
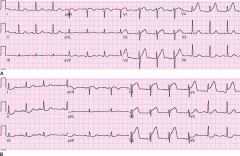
Tented T-waves, V3/4, early AMI
|
|
|
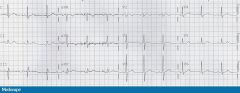
Acute pericarditis, stage I/II
|
|

|
Acute perciarditis, stage I
|
|
|
On physical examination, he appears well. The abdomen is mildly tender without guarding or rebound. Rectal examination is normal. Hemoglobin is 12 g/dL (120 g/L), the leukocyte count is 11,300/µL (11.3 × 109/L), and the erythrocyte sedimentation rate is 38 mm/h. Colonoscopy shows areas of inflammation throughout the colon associated with friability, granularity, and deep ulcerations. The inflamed areas are separated by relatively normal-appearing mucosa, including normal rectal mucosa. The ileum appears normal. Biopsy samples from the inflamed areas of the colon show moderately active chronic colitis without granulomas. Biopsy samples from the ileum are normal.
Which of the following is the most likely diagnosis? A) Crohn's disease B) Ulcerative colitis C) Microscopic colitis D) Yersinia enterocolitis E) Ischemic colitis |
A) Crohn's disease
areas of deep ulceration separated by areas of normal mucosa (skip lesions) and rectal sparing, his findings are more consistent with Crohn's disease than with ulcerative colitis. The absence of ileal inflammation and granulomas on biopsy does not rule out a diagnosis of Crohn's disease. In addition, the patient is a smoker, which increases the risk for Crohn's disease. Patients with ulcerative colitis have continuous inflammation, typically including the rectum, and usually do not have deep ulcers or skip lesions |
|
|
A 55-year-old man is evaluated for excessive daytime sleepiness and hypertension. His wife reports that he snores loudly, causing her to have to sleep in a separate bedroom. He also had a minor car accident when he fell asleep while driving.
On physical examination, the patient is an obese man (BMI 32) with a thick neck; the blood pressure is 145/90 mm Hg. Cardiopulmonary examination is otherwise normal. What is the most appropriate next step in the management of this patient? A) An attended laboratory polysomnography B) Nighttime continuous pulse oximetry C) Automated positive airway pressure (APAP) therapy D) Modafinil therapy |
A) An attended laboratory polysomnography
Polysomnography is indicated for the evaluation of a patient with clinical features suggestive of obstructive sleep apnea. Neither physical examination findings nor continuous nocturnal pulse oximetry is sensitive or specific enough to make the diagnosis. |
|
|
A 35-year-old man has a 2-day history of painful sores on his penis without fever, headache, dysuria, or photophobia. He has never had similar lesions. The patient reports a new sexual partner for the past 6 months but does not know if his partner has a history of any sexually transmitted diseases.
On physical examination, vital signs are normal. There is no rash or evidence of meningismus. Nontender right inguinal lymphadenopathy is noted. Examination of the genitals reveals three vesiculoulcerative lesions clustered on the right side of the penile shaft. The lesions have an erythematous base and a serpiginous border. Which of the following is the most likely diagnosis? A) Herpes zoster B) Herpes simplex virus infection C) Syphilis D) Group B streptococcal infection |
The presentation is most compatible with recurrent genital herpes simplex virus infection. The limited number of lesions and absence of systemic findings support this diagnosis. Herpes zoster lesions would be more extensive and would involve other areas in a dermatomal distribution. Lesions in patients with syphilis are not painful and do not have a serpiginous border. Group B streptococcal infection would involve the scrotum rather than the penis and only rarely causes lesions.
Key Point Genital herpes simplex virus in a male patient is generally characterized by a limited number of genital vesiculoulcerative lesions without systemic symptoms. |
|
|
A 25-year-old man is evaluated for a two-month history of low-grade fevers, cough, night sweats, fatigue, pleuritic chest pain, and weight loss. The patient emigrated from Mexico almost two years ago and now lives in Central California.
On physical examination, his temperature is 38° C (100.4° F), pulse rate is 96/min and regular, respiration rate is 22/min at rest, and oxygen saturation is 94% on room air. There is diminished breath sound and vocal fremitus over the right hemithorax. The left lung is clear. Peripheral blood leukocyte count is 9000/ μL (9 x 109/L), with 60% neutrophils and 35% lymphocytes. Liver function test results are normal. Chest radiograph shows a moderate right-sided pleural effusion with layering of 3 cm of free-flowing pleural fluid and no parenchymal infiltrates on right lateral decubitus chest radiograph. Thoracentesis yields 1.0 L of minimally turbid, yellow fluid with test results as follows: Laboratory Studies Pleural fluid cell count Leukocyte count 3000/μL (3 x 109/L) with 5% neutrophils, 85% lymphocytes, 1% mesothelial cells, and 1% macrophages Total protein 5.5 mg/dL (55 g/L) Lactate dehydrogenase 290 U/L Glucose 80 mg/dL (4.44 mmol/L) pH 7.36 Pleural fluid Gram, fungal, and acid-fast bacilli stains are negative. Tuberculin skin test is pending. Serologic tests for fungal organisms are negative. Cytologic evaluation for malignant cells is negative. Which of the following is the most likely diagnosis? A) Tuberculosis B) Pneumococcal parapneumonic effusion C) Pulmonary embolism D) Malignant pleural effusion E) Pleural effusion due to coccidiodomycosis |
The correct answer is A) Tuberculosis
Tuberculous pleural effusion is the most likely diagnosis. The PPD is positive in about 50% to 70% of patients with tuberculous pleuritis at the time of admission. A negative PPD skin test therefore does not rule out the diagnosis of tuberculous pleuritis. In patients who are not anergic, the PPD will usually become positive within 8 weeks of the development of symptoms of tuberculous pleuritis. Parapneumonic effusion is usually associated with a neutrophilic pleocytosis. The clinical history is more suggestive of tuberculous pleural effusion than pulmonary embolism, in which illness is generally more acute. Malignant pleural effusion would be more likely in the absence of fever and in an older individual. The presentation and pleural fluid characteristic of fungal pleural effusion is similar to tuberculous pleural effusion, and the patient's residence in Central California increases the suspicion for coccidioidal effusion. However, fungal serologic studies usually reveal elevated titers of anti-coccidioides antibodies. |

