![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
34 Cards in this Set
- Front
- Back
|
3 types of haemophilia
|
● Hemophilia A which is an inherited, X-linked, recessive disorder resulting in a deficiency of functional plasma coagulation factor VIII.
● Hemophilia B which is an inherited, X-linked, recessive disorder resulting in a deficiency of functional plasma coagulation factor IX. ● von Willebrand disease, which is a dysfunction of, reduction of, or a complete lack of the protein von Willebrand factor. |
|
|
Severity grading is based on
|
factor levels (<2% severe, 2-5 moderate, 5-30 mild)
Determines time of diagnosis, degree of spontaneous bleeding (esp arthropathy), and whether bleeding only occurs with surgery/dental work. Mild disease may also occur in female “carriers” of hemophilia |
|
|
Which is incorrect
1. Haem A&B typically produces bleeding delayed after trauma as the initial platelet response is normal 2. INR/PT UNAFFECTED in all haemophilias, APPT is usually prolonged 3. Any evidence of bleeding including mild joint pain that may be haemarthrosis gets recombinant or plasma derived factor replacement 4. Petechiae and purpura are characteristic 5. DDAVP is part of treatment of all VWD (if previous response), and some haemophilia A; it is given in consultation with haematology |
4. NO ecchymoses are characterisitic. Petechiae/purpura = platelet problem
|
|
|
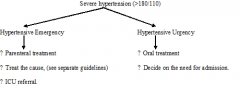
Definitions hypertensive urgency/emergency
|
Emergency hypertension AND signs of life threatening end organ damage
- hypertensive encephalopathy - MI - Aortic dissection - APO - acute on chronic renal failure - pre-eclampsia, eclampsia - SAH - acute sympathomimetic drug overdose Urgency >180/>110, needs treatment, but not immediately life threatening. Lower over 48 hours, oral agent Distinguish true hypertensive “urgency” from a secondary “physiological” hypertension that is due to pain, anxiety, urinary retention or hypoxia. This is most commonly seen in patients with impaired ability to communicate. Treatment is directed to the underlying cause. The blood pressure itself will not usually require specific treatment. |
|
|
Causes chronic hypertension
|
The Causes of Chronic Hypertension
These include: 1. Essential ● The vast majority of cases, (95%) and Secondary causes: 2. Endocrine ● Cushing’s disease. ● Primary aldosteronism, (Conn’s disease) ● Pheochromocytoma. 3. Vascular anomalies ● Coarctation of the aorta. ● Renal artery stenosis. 4. Pregnancy related, (eclampsia and pre-eclampsia) 5. Drug related. |
|
|
What is malignant hypertension?
|
Malignant hypertension is:
● Severe hypertension With ● Retinal hemorrhages, exudates, or papilledema. There may also be renal impairment, often referred to as malignant nephrosclerosis. untreated there is high morbidity and mortality at one year from diagnosis. |
|
|
Significance of hypokalaemia in severe hypertension
|
In the absence of an obvious cause, this may suggest secondary causes relating to hyperaldosteronism.
This itself may be either primary, (Conn’s syndrome) or secondary, (most commonly from renal artery stenosis) |
|
|
Inpatient investigations/SSU investigations for secondary cause in hypertensive urgency or malignant hypertension
|
Renin/ aldosterone ratio measurements:
● These are done to help differentiate a possible primary from a secondary hyperaldosteronism. ● It is best to order this test before commencing various medications (eg ACE inhibitors, beta blockers or diuretics which may make interpretation of the rennin/ aldosterone measurements difficult. Further investigations will then in most cases require admission and should include: Catecholamine excretion: ● This is done via a 24 hour urinary collection, (or preferably if available via a single metanephrine level) ● Failure to diagnose a phaeochromocytoma, can be catastrophic. Renal Ultrasound and Doppler Ultrasound: ● Looking for renal scarring and/ or renal artery stenosis. Note that when an ultrasound is requested, a hypertension study needs to be specifically requested, (not simply a "renal ultrasound"), which will include renal artery Doppler studies, that are required for the diagnosis of renal artery stenosis. |
|
|
Severe hypertension rx algorithm
|
|
|
|
Hypertensive urgency aim of rx
Agents to consider |
aim of treatment in these cases is to lower blood pressure slowly. This usually means over a period of at least 48 hours by means of an oral antihypertensive agent.
Suitable short acting oral agents include: ● Nifedipine 5-10 mg ● Captopril 6.25-25 mg ● Methyl-dopa 250-500 mg Do not give nifedipine (or captopril) sublingually as this may precipitate sudden and excessive hypotension. Suitable longer acting oral agents include: ● Irbesartin 75-300 mg ● Perindopril 1-4 mg Amlodipine 2.5-10 mg ● Atenolol 25-50 mg |
|
|
Hypertensive urgency - decision to admit?
|
Admission Criteria for Hypertensive Urgencies:
As a general rule the higher the blood pressure above 180/110 the more advisable will be admission. Factors to consider include: ● Patient comorbidities ● The absolute level of blood pressure ● The need for investigation, particularly with first presentations, or in patients who have not been adequately investigated. ● Patient social/ reliability factors A short Stay Unit Admission This is useful for patients with severe (>180/110) or malignant hypertension to ensure: ● Investigation ● Initiation of treatment and monitoring of response. ● Stabilization of blood pressure ● Initial patient education |
|
|
What is tumour lysis syndrome
Quartet of biochem abnormalities Settings in which it occurs |
It occurs as a result of the rapid lysis of tumour cells, which leads to the release of toxic amounts of tumour intracellular contents into the circulation.
● Hyperuricemia ● Hyperphosphatemia ● Hyperkalemia ● Hypocalcemia, (secondary to elevated phosphate). 1 Spontaneously: ● In tumours with high proliferative rates. 2 Following initiation of chemotherapy or radiotherapy. |
|
|
Life threatening complications
|
● Acute renal failure, which may be due to a number of factors including:
Uric acid nephropathy. Nephrocalcinosis, (calcium phosphate deposition). Dehydration ● Arrhythmias Due to hyperkalemia in particular. ● Seizures |
|
|
High risk scenarios for TLS
|
TLS is most commonly seen after therapy for aggressive hematologic malignancies, (such as high-grade lymphomas and acute leukemias), and commonly within 48 hours of the first cycle of therapy.
Less commonly TLS may be seen after the treatment of solid tissue tumours. It may also rarely occur spontaneously prior to therapy. Important risk factors relate to: ● Tumour type ● Renal impairment ● Dehydration |
|
|
Regarding TLS management
1. utility of uric acid level 2. management of calcium, phosphate, uric acid |
Can be a surrogate marker for tumour bulk and rapid cell turnover.
Hypocalcemia: ● Correction should be avoided where possible when there is concurrent high phosphate because of the risk of precipitation of insoluble calcium phosphate. ● Only symptomatic hypocalcaemia need be corrected. ● Give IV calcium gluconate: 10% 10 to 20 mL (= 1 to 2 gms) IV over 10 to 20 minutes Hyperphosphatemia: ● Phosphate binders (e.g.: aluminum hydroxide) for mildly elevated levels. ● May require dialysis Hyperuricemia - haematologists to assist with dosing below agents Allopurinol: ● This can be given orally or IV. Rasburicase: ● This is recombinant urate oxidase that converts uric acid to allantoin, an inactive and soluble metabolite of uric acid that is easily excreted in the urine. It is used in order to prevent uric acid nephropathy Dialysis: ● There should be early consideration of dialysis when creatinine, potassium, or phosphorous levels rise significantly. |
|
|
Acute cholecystitis which is correct
1. the absence of physical findings or abnormal blood tests can exclude cholecystitis as early as four hours after onset persistent epigastric/RUQ pain 2. Gas forming organisms, such as clostridia species are responsible for emphysematous cholecystitis 3. patients typically writhe in discomfort as per biliary colic 4. XR will show no findings 5. the treatment of emphysematous cholecystitis is urgent AB's |
1. no - can't exclude; prolonged biliary pain >4 hours likely to have some degree of cholecystitis and index of suspicion remains high even if normal exam/Ix
2. correct 3. no, still because of peritonism 4. There may be indirect indicators of cholecystitis, including: ♥ Sentinel bowel loops. ♥ Basal lung atelectasis. ♥ Gall stones, (the majority will be radiolucent, however) ● In cases of emphysematous cholecystitis radiological signs may be detectable on the plain x-ray film, (see below) 5. no - SURGERY urgently |
|
|
Complications of cholecystitis
|
1. Associated pancreatitis,:
● Especially with calculus cholecystitis. 2. Ascending cholangitis: ● Associated with impacted gallstones 3. Generalized septicaemia. 4. Gangrene and perforation: ● More common in cases of acalculus and emphysematous cholecystitis with subsequent peritonitis. 5. Fistula formation into bowel. 6. Adjacent lung atelectasis. |
|
|
Ultrasound findings of acute cholecystitis
|
Ultrasonic signs of cholecystitis include:
● Thickened gallbladder wall, (greater than 3 mm) ● Positive ultrasonic Murphy’s sign, (tenderness on direct probe pressure). ● The presence of pericholecystic fluid, (from perforation or exudate). ● Air in the gall bladder wall suggests emphysematous (or gangrenous) cholecystitis. |
|
|
Regarding hypokalaemia
Describe ECG changes |
1. Development of U waves (earliest sign).
2. Depression of ST segment and flattening of T wave, with increasing prominence of U wave, (i.e as T wave flattens, the U wave increases and vice versa as hypokalemia resolves). 3. Increased QT segment (with potential for torsade). 4. Elevation of P wave. 5. Mild prolongation of the PR interval 6. Arrhythmias, as listed below. |
|
|
In severe symptomatic or life threatening cases maximum rate IV administration...
|
20-40mmol/hr may be given
● Baseline potassium level has been documented. ● Normal renal function. ● Adequate urine output. ● ECG monitoring. Can push/bolus if cardiac arrest and suspected cause is K |
|
|
Two main causes hypercalcaemia
|
malignancy or primary hyperparathyroidism, all other causes are rare.
|
|
|
Complications of hypercalcaemia - which is incorrect
1. confusion, drowsiness, coma 2. hyperreflexia 3. pancreatitis and peptic ulceration 4. increased digoxin sensitivity 5. VF/cardiac arrest 6. nephrogenic DI |
2 HYPOreflexia
|
|
|
Level at which acute hypercalcaemia is usually symptomatic
Renal function should always be checked. Which other blood test is particularly helpful? |
>3.5 mmol/L - this is considered severe
PTH |
|
|
ECG features hypercalcaemia
|
Lesser degrees of hypercalcemia cause two well recognized, but subtle and non-specific changes:
● Prolongation of the P-R interval ● Shortening of the QT interval, (primarily via shortening of the ST segment). It is really only at very high levels, that marked ECG changes begin to occur, and these are often not recognized because of their rarity. These may include: ● A concave upward ST elevation or “pseudo-infract” pattern, (coronary angiography is normal and troponin levels are not elevated). 3 ● Large pseudo - Osborne (or J) waves: ♥ These are normally seen in hypothermia, as an extra upward deflection between the R and the T wave that may be fused with the downstroke of the QRS complex. 4 ● Arrhythmias: ♥ Ventricular irritability with VEs. 5 ♥ Cardiac arrest in VF. 6 |
|
|
Hypercalcaemia therapy
|
IVF
Saline diuresis up to 4 - 6L per 24 hours. ● Corrects dehydration ● Increases calcium loss by increased filtration. ● Increased sodium load will help inhibit the proximal tubular reabsorption of calcium. Bisphosphonates Use pamidromate 30 to 90 mg IV, over 2 to 4 hours (not recommended in severe renal impairment - discuss with ICU) Calcitonin IM or IV may have a role if life threatening Glucocorticoids if excess Vit D implicated Dialysis if life threatening, failure of conservative measures or oliguric renal failure INVESTIGATE AND TREAT THE CAUSE |
|
|
3 venomous jellyfish in Australia
|
● Chironex fleckeri (the Box Jellyfish).
● Physalia Physalis (the Portuguese Mar of War, blue bottle) ● Carukia Barnesi (the Irukandji) |
|
|
Which is incorrect?
1. children are a higher risk of significant envenomation due to their smaller body sizes 2. the species most likely to be fatal is the box jellyfish 3. the Portugese Man of War may rarely cause death possibly due to stimulation of massive catecholamine release 4. specific antihypertensive therapy may be required for irukandji syndrome |
3. IRUKANJI causes catecholamine release
|
|
|
Regarding Box Jellyfish T/F
1. death may occur within 20-30 minutes 2. a major sting is more than 50% involvement of a limb 3. wheals greater than 1m are likely to be lethal 4. wheals may later blister and undergo necrosis 5. delayed hypersensitivity reactions (pruritic erythema 1-2 weeks later) are rare 6. Pressure immobilisation bandage should be used 7. Vinegar should be used 8. Tentacle remnants can be picked off without harm to rescuer |
3. FALSE - >6m in adults (just over 1m in a child has caused death)
5. FALSE - very common 6. FALSE |
|
|
In CVS collapse due to box jellyfish envenomation, which two therapies should be used?
|
1. Antivenom 6amp for arrest otherwise 3 for CVS effects (collapse, hypotension, arrhythmia)
2. MgSO4!! up to 10mmol IV over 5-15 minutes |
|
|
Regarding Portugese Man of War T/F
1. frequently fatal with extensive stings 2. found in Northern Australia 3. a long trailing tentacle of up to 10m is responsible for most stings 4. dermal reaction is cross hatching welts 5. systemic symptoms are uncommon - occasionally GIT upset, myalgias, resp distress 6. continuous hot water treatment 45 degrees for 20 minutes may deactivate venom 7. vinegar should be used |
1. FALSE - not been shown to be fatal
2. FALSE - all coastal regions Australia 4, FALSE (cross hatching = box) - linear erythematous welts and papules 7. FALSE UNLESS Box jellyfish is in the differential |
|
|
Regarding Irukandji
1. antivenom exists 2. Northern waters of Australia only 3. small jellyfish, bell only 2.5cm, severe pain 4. elevations in serum troponin may occur due to cardiac toxicity 5. pulmonary oedema occurs due to direct pulmonary toxicity 6. skin signs may be minimal; erythematous papular rash may occur 7. development of “irukandji syndrome”, can occur within 30-120 minutes of being stung |
1. FALSE
5. FALSE secondary to cardiac toxicity |
|
|
Irukandji syndrome
|
● Nausea and vomiting.
● Severe muscular pains ● Adrenergic response, (hypertension, tachycardia, sweating, anxiety or dysphoria). This state may induce secondary complication such as: ♥ ICH Rarely more severe cardiac toxicity may occur: ♥ Myocardial depression ♥ ECG changes, (T wave inversion and ST segment depression have been described). ♥ Pulmonary edema Symptoms generally resolve over 1-3 days. |
|
|
Irukandji sting/syndrome treatment
|
Vinegar
Analgesia - large doses opioids Tetanus immunoprophylaxis (for all jellyfish) Antihypertensive if refractory hypertension to analgesia e.g GTN infusion MgSO4 - no benefit in one RCT, may have a role |
|
|
Trifasicular block
|
x
|

