![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
PEA prognosis is variable. What may suggests a good prognosis, and what a poor prognosis?
|
Better prognosis - sinus tachycardia or other 'perfusing rhythm', may have better outcome
Terrible prognosis - agonal or other non perfusing rhythm |
|
|
In all intubated patients arriving in the ED, what is a key first priority
|
Ensure the ETT is correctly located
|
|
|
When an error or clinical incident occurs in the department, what is the term which encompasses the process of explaining to the patient what has occurred?
|
Open disclosure.
|
|
|
Differentials for a wide mediastinum
|
Trauma - paramediastinal veins cause apical cap, haematoma secondary to bony injury (e.g. vertebrae, sternum)
Esophageal rupture - pneumomediastinum Preexisting pathology e.g. LAD, malignancy |
|
|
Options for investigating traumatic widened mediastinum
|
FAST
TTE CTA (MRI) |
|
|
Traumatic Aortic injury vs Aortic dissection findings on CT
|
Traumatic
- pleural cap and basal effusion, indirect indicators of aortic injury (suggest degree of force) - NB blood is NOT from aorta but paramediastinal veins Ao Dissection - widened mediastinum, no pleural effusion unless has ruptured and critically unwell |
|
|
SJS eye involvement - typical appearance?
|
Conjunctivitis with limbic sparing
|
|
|
How are EM, SJS and TEN differentiated
|
EM just skin
SJS has MUCOSAL involvement TEN has MUCOSAL involvement AND >30% skin involved |
|
|
DDx CVA
|
1. Space occupying lesions.
2. Extra-axial traumatic hemorrhage, (subdural or extradural). 3. Venous sinus thrombosis. 4. Metabolic disorders, including hyponatremia, hypoglycemia, hyperglycemia or Wernicke’s encephalopathy. 5. Todd’s paresis. 6. Demyelinating disease. 7. Hysterical. 8. Hemiparetic migraine |
|
|
BP goals in stroke patient
|
Ischaemic CVA - <210/120
Requiring thrombolysis <185/110 Haemorrhagic CVA - <180/110 ?? need to check GTN infusion can be used to control (also SNP, labetalol, hydralazine). In normally hypertensive patient continue usual regime |
|
|
Antiplatelet agents in CVA - who, what, how
|
If requiring thrombolysis - DON'T GIVE
If no thrombolysis - give aspirin, unless C/I or patient on aspirin prior to CVA then clopidogrel (or asasantin if 2nd scenario) |
|
|
Thrombolysis - when, what
|
<4.5/24 (ideally <90 minutes)
rt-PA - recombinant tissue plasminogen activator |
|
|
What are the neurointerventions available for stroke?
|
Neurointervention:
Neurointervention techniques refer to: ● Intra-arterial thrombolysis, (within 6 hours) in carefully selected patients. ● Percutaneous transluminal angioplasty and stenting. ● Mechanical clot removal (within 8 hours). These types of interventions are currently only available in a few large urban centers. They have yet to be fully evaluated. These interventions may have a role in cases of large proximal clots, (see appendix 2 below) - that do not respond well to thrombolysis therapy. |
|
|
Use of heparin
|
Heparin:
The routine use of early anti-coagulation in unselected patients following ischemic stroke is not routinely recommended. |
|
|
What is the role of neurosurgery?
|
Neurosurgery:
Large acute infarcts can lead to significant cerebral edema resulting in rapid clinical deterioration and death. In selected cases, urgent hemicraniectomy may be considered. Criteria include: 1 ● Age 18-60 years ● Surgery is undertaken with 48 hours of symptom onset. ● Large middle cerebral artery infarction (or large life-threatening space occupying cerebral edema in general), sometimes referred to as “malignant infarction” Corticosteroids are not recommended for cerebral edema due to infarction. Mannitol and hyperventilation may have some benefit in rapidly deteriorating patients due to raised intracranial pressure. |
|
|
Regarding basilar artery thrombosis, which is incorrect
1. Mortality and significant morbidity are very high without timely recanalization with thrombolytic agents or embolectomy. 2. the therapeutic window for thrombolytic therapy is prolonged to around 12 hours 3. fluctuating initial symptoms of alterations in conscious state in combination with brainstem signs are uncommon 4. the patient may present with a “locked in” type picture, where the patient is unconscious and quadraparetic. 5. is one of the few indications to use CONTRAST with a CTB for suspected stroke 6. urokinase is preferable to rtPA 7. heparin is not indicated 8. mechanical clot retrieval/embolectomy may be employed |
3. common, and occur over a period of hours to even days
|
|
|
Describe the clinical presentation of basilar artery thrombosis
|
● Transient loss of consciousness
● Nausea and vomiting ● Diplopia ● Dysarthria ● Bilateral visual disturbance ● Vertigo, particularly in association with hearing loss. ● Quadraparesis/ sensory loss ♥ Although lesser variations of this are possible in lesser degrees of ischaemia, such as that confined to a vertebral artery. In the fully developed syndrome: 1. Unconscious 2. Quadraparesis (a so-called “locked in” type picture, with variable degrees of awareness). 3. Dysconjugate eye movements, third, sixth cranial nerve abnormalities. 4. Pupillary abnormalities. 5. Bilateral upgoing plantar responses. |
|
|
Regarding TIA which is incorrect
1. the diagnosis is made if at 24 hours there has been complete resolution 2. the recognition of earlier episodes is important 3. symptoms present at 1/24 are likely to persist past 24 hours and be considered a stroke 4. risk stratification is important |
Most TIA's show resolution within 10/60
|
|
|
The ABCD2 score - components
|
Age > 60 (1)
BP >140/and or >90 (1) Clinical features - hemiparesis (2), isolated speech deficit (1) Duration 10-60 (1), >60 (2) Diabetes (1) > 4 (e.g. 5 and above) is considered high risk >4% for CVA within 48 hours and mandates admission. 0-3 is ~1% |
|
|
Regarding investigation of TIA which is incorrect
1. all patients should have a carotid Doppler 2. Doppler should be done <24 hours IF ABCD2 >4, amaurosis fugax, recurrent or crescendo sx 3. In low risk groups Doppler should be done within 48-72 hours 4. MRI is important if diagnostic uncertainty, or carotid artery dissection suspected; provided prognostic information (e.g. if abnormal or occlusions shown, higher risk of subsequent stroke) 5. Echo is done where suspicious of cardiac source OR no other source identified |
1. NO only those with anterior circulation signs
|
|
|
What is the role of heparin in TIA?
|
Only two specific circumstances
1. crescendo TIA with known high grade carotid artery stenosis, amenable to endarterectomy 2. high risk cardiac embolic source e.g. known LV/left atrial clot, severe cardiomyopathy or some AF |
|
|
What considerations make a TIA patient high risk?
|
● Those with an ABCD 2 score of > 4.
● Those with amaurosis fugax. ● Those with crescendo symptoms, ie 2 or more recent events. ● Those with a high index of suspicion for a cardiac embolic source. ● Symptomatic patients with high grade carotid stenosis. ● Those patients with associated severe uncontrolled hypertension. ● Patients who have TIA in the setting of ACS. ● Those with an acute infarct detected on CT, (even though symptoms have resolved). Should have Ix done prior to leaving hospital. Ideally go to stroke unit or short stay (minimum). Medical treatment initiated. Management plan. Education re stroke/TIA and RF. Observation period. Once d/c should be referred to specialist within 48 hours |
|
|
Who should TIAs (esp recurrent) with high grade stenosis be referred to?
|
Vascular surgeon, urgently
|
|
|
Regarding vertigo which is correct
1. peripheral causes are benign 2. cerebellar infarction always presents with vertigo and localising signs 3. decision for imaging is based on neuro exam (HINTS) and CVS risk profile 4. the slow phase of nystagmus is towards the unaffected side (away from the lesion) 5. nystagmus direction is named by the direction of the slow phase |
1. peripheral causes may include bacterial labrynthitis or acoustic neuroma
2. 10% isolated 3. CORRECT 4. slow phase TOWARDS lesion 5. named direction is QUICK phase |
|
|
Vertigo - peripheral
How does the presence or absence of deafness/tinnitus divide causes? |
Deafness/tinnitus
- labrynthitis - ototoxic drugs - acoustic neuroma - Meniere's disease - internal auditory small artery disease No D/T - vestibular neuronitis - BPPV |
|
|
Causes of central vertigo
|
Vascular:
Posterior fossa, i.e. brain stem or cerebellar lesions ♥ Ischemia, (e.g. cerebellar or lateral medullary syndrome or variations thereof) ♥ Hemorrhagic lesions ♥ Migraine variants. Less commonly: ● Central space occupying lesions ● Demyelination lesions. ● CNS infection (encephalitis, abscess or meningitis) |
|
|
Which of the following suggest central cause?
1. gait or truncal ataxia 2. vertical nystagmus 3. diplopia, dysarthria, dysphagia 4. a head impulse test which is abnormal (e.g. presence of catch up saccades - eyes do not continue to fix on nose) 5. unidirectional nystagmus (beats to the same side no matter where patient looks, Cf directional - nystagmus changes with gaze direction) 6. vertically disconjugate gaze |
1, 2, 3, 6
4. NO, this suggests peripheral causes; a NORMAL HI tests suggests central 5. NO suggests peripheral; central cause changes with direction |
|
|
Management considerations in vertigo
|
● Control of the patient’s symptoms
● Deciding on the need for imaging, and what type of imaging ● Treatment of the underlying cause of the vertigo, (where possible). ● The disposition of the patient |
|
|
Regarding digoxin, which is incorrect?
1. NaK ATPase pump inhibition leads to a decrease in intracellular calcium 2. lethal toxicity potential at 10mg adults, 4mg children 3. K levels >5.5. serum levels >15nmol/L may indicated lethal dig toxicity 4. death from CVS complications occurs 8-12 hours |
1. INCREASE, and hence increased automaticity
|
|
|
Cardiac manifestations of Dig toxicity
|
Enhanced automaticity:
● Ventricular ectopic contractions, (less commonly atrial) ● Atrial tachycardias, often with A-V blocks ● VT ● VF Bradyarrhythmias: ● Conduction delays / blocks ● Pre-existing AF that has become very slow, (note, AF and atrial flutter are not typically caused by digoxin toxicity. It is the ventricular rate that is affected) |
|
|
When should dig levels be done?
|
Immediately, 4 hours post ingestion, then 2 hourly after this
|
|
|
Three things to avoid or use with extreme caution in Dig toxicity
|
1. adrenaline for bradyarrhythmias - may aggravate cardiac toxicity
2. Cardioversion for tachyarrhythmia - poor efficacy, and may cause VF - if unavoidable lowest effective amount of energy 3. Ca for hyperkalaemia - theoretically may enhance dig toxicity, but in practice may simply be ineffective (intracellular Ca is already raised) The definitive treatment of ALL of these is Fab fragments |
|
|
Chronic dig toxicity which is incorrect
1. occurs with relatively normal dig levels 2. likelihood progressively increases with presentations of bradycardia, automaticity or GI symptoms 3. commonly occurs with intercurrent illness, renal failure 4. xanthopsia and chromatopsia may occur 5. a common mistake is to withhold Fab fragments due to underestimation of lethality/concerns about cost |
1. therapeutic range 0.6-1.3nmol/L, toxic 1.9-3.2ng/ml!!
2. INCORRECT - bradycardia less likely than GI symptoms, less likely than automaticity The onset is insidious over days to weeks and features may include those listed above under acute intoxication together with visual disturbances such as reduced acuity, yellow halos (xanthopsia) and altered color perception (chromatopsia). |
|
|
Digibind/Fab fragment administration
1. how quickly does it work? 2. should be given at the onset of life-threatening toxicity? 3. What are the endpoints of therapy? 4. How much does 1 amp bind? |
Response within 20/60
No - may be given beforehand where risk assessment may be made e.g. >10mg adult >4 child, >15nmol/L level Restoration of normal cardiac rhythm and conduction. Resolution of nausea and vomiting 1 amp bind 0.5mg of digoxin |
|
|
Horner's syndrome - where could the lesion be?
|
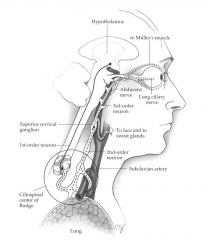
● Hypothalamus
● Sympathetic nucleus of the brainstem ● Cervical and upper thoracic cord. ● Anterior spinal first thoracic root ● Sympathetic chain and stellate ganglion ● Carotid sympathetic plexus. 1.Brainstem: ●Vascular, especially as part of lateral medullary syndrome. ●Tumour ●Syringobulbia 2.Neck: ●tumour, thyroid, lymph nodes. ●Trauma / surgery ●Vascular lesions, carotid aneurysms or dissections ●Syringomyelia (may cause a bilateral Horner’s) 3.Chest: ●Pancoast tumour, (ie apical lung tumours) ●Look for a T1 lesion 4.Intracranial (but outside the brainstem) ●Carotid aneurysms ●Cavernous sinus disease |
|
|
What does 'everything gets smaller' mean in terms of Horner's syndrome?
|
Miosis
Ptosis Enophthalmos (likely appearance rather than genuine enophthalmos) Less sweating (anhydrosis) - this only occurs if lesion occurs before the sympathetics re-enter the cranium (where it is intracranial but outside the brainstem). If no anhidrosis = partial |
|
|
Regarding Horner's which is incorrect
1. combination of Horner’s syndrome and neck pain and or mass may be the first indication of a carotid artery dissection 2. MRI may be the best test if a brainstem lesion is suspected 3. Doppler is the definitive test for carotid lesions 4. A CT may need to be done of head neck and chest |
3, No, MRA or CTA
|
|
|
Regarding hanging which is incorrect
1. in those who survive to hospital c-spine fracture is common 2. non cardiogenic pulmonary oedema is a main pathology 3. if falling greater than body height death by high cervical fracture (usually Hangman's, bilateral pedicle fracture C2) is virtually assured 4. Where Hangman's fractures occur, brainstem transection, respiratory and cardiac arrest and bilateral common carotid artery dissection are common 5 non judicial hangings typically lead to vascular congestion, cerebral oedema and hypoxic encephalopathy |
1 UNCOMMON
2 yes as well as hypoxic ischaemic encephalopathy |
|
|
Non judicial (commonly incomplete or atypical hangings) have what progression of pathology?
|
There is initial venous obstruction, leading to raised intracranial pressure and reduced cerebral blood flow leading to stagnant hypoxia.
Loss of consciousness occurs. Loss of neck musculature tone follows this. Arterial obstruction then follows, leading to anoxic brain injury. |
|
|
Complications of hanging
|
1. Airway injury:
● Laryngeal and hyoid bone fractures, (these are more commonly seen with manual or ligature type strangulations). 2. Neurological: ● Cerebral anoxia and edema with raised intracranial pressure, due to initial venous congestion followed by carotid/ vertebral arterial occlusion 3. Pulmonary: ● Aspiration, delayed pneumonia ● ARDS or non-cardiogenic pulmonary edema. ♥ This is thought to be a type of neurogenic mediated pulmonary edema. 4. Cervical spine fracture: ● Fatal injury in judicial hangings, most commonly by a Hangman’s fracture with associated brainstem transection. ● Much less commonly seen in non-judicial hangings 5. Vascular injury: ● Carotid artery injury is relatively common ● Vertebral artery injury may occur but is less common. |
|
|
What airway issues may be encountered in hanging patients and how could they be managed?
|
Laryngeal injury making intubation difficult
Semielective fibreoptic intubation Delayed oedema/obstruction Observe |
|
|
Bilateral pedicle fractures of C2 - different mechanisms
|
1. hangman's extension/distraction
2. extension/axial compression e.g. diving into pool and hitting bottom, falls from horse |

