![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
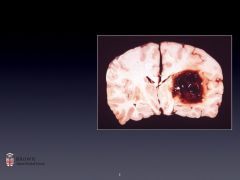
Most common stroke type?
2nd most? 3rd most? |
Ischemic
Intracerebral hemorrhage Subarachnoid hemorrhage |
|
|
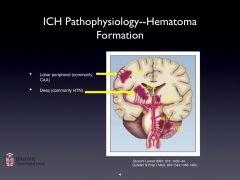
Where in the brain, generally, does intracerebral hemorrhage occur?
|
Deep structures (vessels there are vulnerable to HTN)
|
|
|
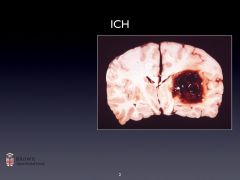
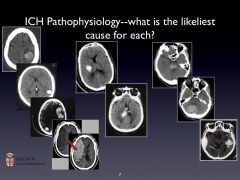
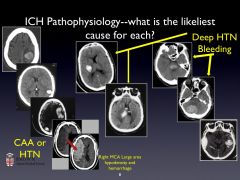
ICH pathophysiology:
6 |
-Rupture of a bv--> hematoma
-Later, hematoma expands -+ ICP -Tissue disruption/ischemia around hemorrhage -Inflammation -Edema/possible herniation |
|
|
Typical ICH locations:
What happens to the artery walls? |
-Small penetrating aa coming off ACA, MCA, PCA, Basilar.
-May be ruptured at multiple sites. -Artery walls have layers of platelet and fibrin aggregates with breakdown of the elastic lamina; smooth muscle atrophy; wall dissection; and cell degeneration. |
|
|
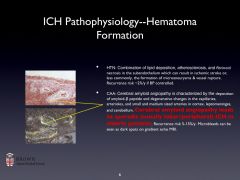
Describe how HTN contributes to ICH:
|
-Combination of lipid deposition, atherosclerosis, and fibrinoid necrosis in the subendothelium can result in ischemic stroke or, less commonly, the formation of microaneurysms & vessel rupture.
Recurrence risk ~2%/y if BP controlled. |
|
|
Cerebral Amyloid Angiopathy:
|
-Hereditary or sporadic.
-Characterized by the deposition of amyloid and degenerative changes in the capillaries, arterioles, and small and medium sized arteries in cortex, leptomeninges, and cerebellum. -Cerebral amyloid angiopathy leads to sporadic (usually lobar) ICH in the elderly. -Recurrence risk 5-15%/y. Microbleeds can be seen as dark spots on gradient echo MRI. There are also white matter hyperintensities. |
|
|
Treatment for CAA?
|
None.
|
|
|
Causes of ICH: 8
|
HTN
CAA Anticoagulants Vascular malformations/aneurysms Tumors Infarction with hemorrhagic transformation Venous sinus thrombosis Drug use |
|
|
Things you must ask about in ICH pts: 6
|
History of Trauma
Hematologic abnormality (coagulopathies) History of anticoagulant med taking Anti-platelet med usage Symptoms prior to the hemorrhage Non-hypertensive site of bleeding |
|
|
ICH presentation of typical ICH patient:
BP, history, etc. |
•Blood pressure > 150/90 in 80% patients
•History of HTN, poor medication compliance, and cardiomegaly are common •No prodromal transient symptoms •Onset while patient is active |
|
|
Signs and symptoms of ICH: 8
|
•Abrupt onset with gradual evolution over minutes to hours
•A one-time event with rare recurrence •Headache appears in only 50% •Neck stiffness •Vomiting (+ICP) •Focal seizures in approximately 10% •Focal symptoms a function of site/size of bleed •Symptoms and signs persist for months |
|
|
Imaging/lab options for ICH evaluation:
|
CT
-Fast (secs-mins), commonly available -Easy to read & very sensitive for acute blood (appears bright white); also may reveal hydrocephalus, edema, mass effect, and (potentially) tumor -Inexpensive MRI -Not so fast (mins-hrs), not so common, not so available -Very sensitive (acute blood); much more sensitive (chronic blood) -Gives a more detailed look for other causes of ICH -Expensive Labs: CBC, Chem, Coags |
|
|
Anticoagulant use and its implications for ICH:
|
-Most ICH occurs within therapeutic range of anticoagulation, but the risk of hematoma formation and expansion in ICH rises with the level of anticoagulation.
-Rapid reversal of Warfarin with FFP, vitamin K, and prothrombin complex concentrate (2,7,9,10) is recommended to resolve coagulopathy. |
|
|
Thrombolytic use and its implications for ICH:
Risk factors? |
-Makes hemorrhage more likely when used to dissolve a clot. TPA.
Risk factors: age >70, large stroke, early ischemic changes visible on CT, serum glu > 300 mg/dL |
|
|
Discuss the significance of vascular malformations in causing ICH:
|
-Accounts for 5% of ICH; more common in the young.
-Arteriovenous malformations (AVM) -Dural A-V fistulas (dAVF) -Cavernous malformations -Aneurysms (berry, saccular, or infective) |
|
|
Who should get an angiogram to try to detect vascular malformations?
|
-Probably only young, healthy people (some risk attached to them)
-Imaging (MRI) can serve the function of an angiogram to an extent and is non-invasive. |
|
|
Treatment for ICH:
supportive measures? 6 |
-No Definitive Treatment
-Supportive care: *Correct treatable causes of bleeding *Treat seizures (not prophylaxis) *Treat raised intracranial pressure *Blood pressure management; levels are under debate. *Surgery is controversial (Probably only helpful in avoiding catastrophic herniation or if ICH close to surface) *ICU/hospital care & prophylaxis: DVT, GI, euthermia/ euglycemia |
|
|
Prognosis for ICH:
how does it compare to ischemic stroke? Medical cost of ischemic stroke: |
Mortality
6-month, 30%-50% 1-year, 50% Functional recovery *much worse than ischemic stroke Medical Cost < 20% of ICH patients are independent at 6 months vs 60% of ischemic stroke patients $125,000 lifetime cost per person (1990) |
|
|
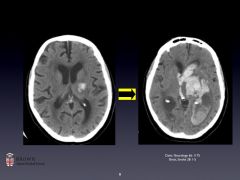
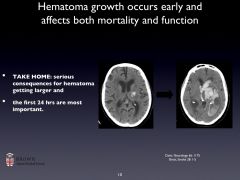
What does prognosis of ICH depend on?
other factors at play? |
-Prognosis depends on Size and Site of ICH
-Size (hematoma volume): 35-50% overall mortality ~75% mortality from massive ICH -Site: worse prognosis for midline, infratentorial (higher risk for brainstem compression) -Other factors: age, presence of IVH, edema (probably as a marker for shift), exam on presentation -Early withdrawal of care (careful of self-fulfilling prophecy: pts do poorly after we offer poor prognoses despite incomplete prognosis data): current reccomendations are to hold off DNR for 24h. |
|
|
ICH scores for predicting mortality take what into account? 5
|
-Glasgow coma scale score
-ICH volume -Presence of IVH -Infratentorial origin -Age of pt |
|
|
Data on Subarachnoid Hemorrhage:
prevalance mortality what causes them M/F genetic involvement? risk factors |
-1-7% of all strokes (dep on location), 26,000/y; unruptured aneurysms seen in 2% of routine autopsies
-Mortality approx 45% -Vast majority of non-traumatic SAH are aneurysmal, then other vascular causes such as AVM, also trauma. -More common in women -There's a genetic component. -Smoking is a risk factor. |
|
|
Mortality date on SAH:
|
25-35% 0-30d mortality
~40-45% overall mortality Despite its relatively low incidence, SAH impact is comparable to that of ischemic stroke |
|
|
Has SAH prevalance decreased with smoking cessation and HTN control over the years?
|
No. hasn't helped.
|
|
|
Typical pt comment upon presenting with a SAH?
|
"Worst headache of my life."
-Sudden onset, high intensity -May have had a previous, lower intensity headache due to "sentinel bleeds" (leakage from the aneurysm) |
|
|
Physical findings in SAH pts:
|
-diminished LOC
-Papilledema or retinal hemorrhage -IIId palsy -VIth palsy |
|
|
Predictors of prognosis for SAH:
|
-Hunt/Hess scale links neurological status to outcome.
-LOC is the best predictor! |
|
|
Is surgery a good call to fix a subarachnoid aneurysm?
|
Endovascular coiling is better.
|
|
|
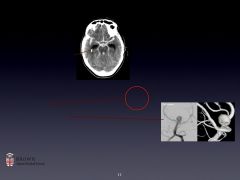
What testing do you do to identify subarachnoid hemorrhage?
|
-CT works really well- subtle brightness paraventricularly
-LP will tell you--presence of RBCs, high opening pressure, xanthochromia -Angiogram (or MRA, CT) |
|
|
The immediate steps in the evaluation of SAH include:
|
-Airway, breathing, and circulation, routine monitoring, labs
-Blood pressure control (usually <140 mm Hg systolic) -Evaluation of hydrocephalus and the need for management with extraventricular drainage (EVD); -Rapid evaluation of the intracranial vasculature and early surgery or endovascular coiling as indicated. -Seizure prophylaxis until the source of the hemorrhage has been identified/controlled; -Bedrest and stool softeners. -Nimodipine, a calcium channel blocker, was originally considered as prophylaxis against vasospasm; though it had no effect on vasospasm, it did have a measurable, as-yet-unspecified neuroprotective effect which improved 6-month outcomes markedly. |
|
|
Describe hydrocephalus in SAH:
|
-Blood in the CSF can cause either a non-communicating or a communicating hydrocephalus.
-Common symptoms: initial confusion and decreased level of alertness, upgaze paresis, somnolence, coma -Patients in whom hydrocephalus is suspected are rapidly re-imaged and, if necessary, given external drainage (EVD) -Resolution of hydrocephalus and clearance of blood from the CSF may take days; if EVD weaning is not possible, a shunt may be placed. |
|
|
Describe vasospasm in SAH:
how do you monitor it and treat it? |
-Leads to 2˚ ischemic injury and strokes (as high as 40%)
-Peaks between days 3-13 after rupture; Pts monitored with serial neuro exams and transcranial doppler evaluation of blood flow velocity through major intracerebral vessels (surrogate marker for vessel diameter) -Occurs more often if thick clots seen on CT -Can be treated by hemodynamic augmentation -Classically HHH therapy (hypertension, hypervolemia, hemodilution) -Now more typically hypertension and euvolemia -Can also be treated with Intra-arterial therapies Vasodilators (commonly calcium channel blockers) Angioplasty |
|
|
What are two common complications of SAH?
|
hydrocephalus
vasospasm |
|
|
Why do complications occur with SAH?
|
Immediately after subarachnoid hemorrhage, a progressive decrease in cerebral blood flow occurs.
This may result from a sudden massive increase in intracranial pressure or from a transient acute vasospasm. The net result is a decrease in cerebral perfusion pressure and, depending on its degree and duration, results in various levels of impaired consciousness or even death. |
|
|
|
|

|
|
|

|
|
|
|
|
|
|
|
|
|

|

