![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
103 Cards in this Set
- Front
- Back
|
what are the top 2 fastest growing older adult populations?
|
1. hispanic
2. asian |
|
|
top 2 causes of death for gero?
|
1. heart disease
2. cancer |
|
|
life expectancy for men and women at age 65?
|
men: 65+17
women: 65 +18.5 |
|
|
7 chronic diseases in older adults in order of prevalence?
|
Hypertension (67%)
Arthritis Heart disease Any cancer Diabetes Stroke; Asthma; Bronchitis or emphysema (9%) |
|
|
what percentage of older adults have a chronic illness?
what percentage have more than 1 chronic illness? |
80%
60% |
|
|
what percentage of older adults rate their health as very good or excellent?
what does this actually reflect? |
65-70%
this is not objective health, though. this actually reflects functionality rather than health. (subjective health) |
|
|
what 3 problems are OAs more vulnerable to?
|
socioeconomic, physical, and emotional problems.
|
|
|
what are IADLs?
|
instrumental ADLs (balancing a checkbook, e.g.)
|
|
|
5 major points of baltimore longitudinal study of aging
|
1. Poor health is not inevitable
Never assume abnormalities are due to aging 2. Symptoms are frequently due to multiple causes 3. Prevalence of most chronic disease increases with age 4. No single chronology of human aging exists Physiological age and chronological age may be disparate 5. Prevention of age related morbidity depends in large part on improving modifiable risk factors |
|
|
brenda's drinking recommendations for OA men and women
|
men - 2 per day, max 14
women - 1 per day, max 7 |
|
|
assessment fields for OA, in order of importance
|
1. Functional assessment (ADLs, IADLs, mobility and balance)
2. Mental and Social History (occupation and hobbies, occupation, etc.) |
|
|
most vulnerable organ in OA?
|
CNS
|
|
|
what percentage of falls are recurrent?
|
50%
|
|
|
what percentage of OA falls result in hospitalization?
|
25%
|
|
|
what's the most common reason for OA hospitalization?
|
hip fracture.
25% die within 6 months 25% lose significant functional capacity 25% have decreased mobility |
|
|
factors influencing falls
|
Change in environment
Lower extremity disability and muscle weakness Visual impairment Gait problems Foot problems Dementia and depression Drugs Balance |
|
|
3 goals in older adult polypharmacy
|
Decrease # of meds
Decrease dosage Assess adherence: Only about 35% adhere to medication regimens |
|
|
what is the SPICES tool?
|
mneumonic for geri problem evaluation
S – sleep disorders P – Problems with eating or feeding I – Incontinence C – Confusion E – Evidence of falls S – Skin breakdown |
|
|
mental status decreases in OAs
|
1. memory - recent goes before distant
2. problem-solving skills 3. executive function |
|
|
mental status fields that tend not to change in OAs
|
personality features
vocabulary skills |
|
|
skin changes in OAs
|
Decreased sebaceous
and sweat gland activity Epidermis thinner, paler, more transparent Loss of subcutaneous fat and elasticity Skin hangs more loosely Increased wrinkling Increased in pigmented areas, freckles, and hypopigmented patches |
|
|
6 types of normal lesions in OAs
|
Cherry angiomas
Cutaneous tags Cutaneous horns Lentigo (liver spots) Sebaceous hyperplasia (divot in middle) Seborrheic keratoses (scaly, brown) |
|
|
hair changes in OAs
|
Decreased head, body, axillary
and pubic hair Hair becomes thinner, sparse and drier Decreased follicle size of terminal hair Symmetrical balding in occiput and frontal areas especially in men Increased coarseness of aural, nasal, and eyebrow hair in men Increased coarse facial hair in women Decrease in melanocyte activity |
|
|
nail changes in OAs
|
Slowed nail growth
Nails become thicker, brittle, hard, and yellow especially toenails May develop longitudinal ridges and splitting |
|
|
musculoskeletal changes in OAs
|
Decreased bone density
Osteoarthritis in cervical spine, weight bearing joints and hands Stature decreases at 50+ Joint cartilage deteriorates Boney prominences more apparent Reduced muscle mass, tone and strength Decreased balance, agility and endurance Slower reaction time and speed of movement |
|
|
GI changes in OAs
|
Reduced GI peristalsis
Decreased secretion & production of digestive enzymes Bacterial flora become less biologically active Decreased mucous lining intestinal tract produces an increased susceptibility to chemical agents including carcinogens Decreased liver mass and blood flow Lose 1/3 of renal function between 20-90 Abdominal wall thinner and less firm Contour of abdomen is usually rounded |
|
|
respiratory changes in OAs
|
Barrel chest
Emphasized dorsal curvature of thoracic spine Decreased chest expansion Decreased exercise tolerance Drier mucous membranes |
|
|
Cardiac changes in OAs
|
Left ventricular wall thickens
Heart contractility decreases Valves calcify and fibrose Orthostatic hypotension Blood pressure increases Apical pulse may be more difficult to find |
|
|
most common sensory impairment in OAs?
|
hearing impairment
|
|
|
visual changes in OAs
|
Decreased tearing
Change in ability to accommodate Increased sensitivity to glare Decreased sensitivity to contrast |
|
|
9 superficial lymph node sites to palpate in HEENT exam
|
1. Occipital - At the base of the skull
2. Postauricular - Behind the ear 3. Preauricular - In front of the ear 4. Parotid & Tonsillar - At the angle of the jaw 5. Submandibular - Under the jaw on the side 6. Submental - Under the jaw in the midline 7. Superficial Anterior Cervical – In the anterior triangle of the neck 8. Posterior cervical – In the posterior triangle along the anterior border of the trapezius 9. Supraclavicular - In the angle of the sternomastoid and the clavicle |
|
|
which node site enlargement usually signals cancer?
|
supraclavicular node enlargement, since the thoracic duct empties into this (thorax and abdomen).
|
|
|
lymphadenopathy mneumonic
|
MIAMI
Malignancy Infections Autoimmune disorders Miscellaneous and unusual conditions Iatrogenic causes |
|
|
upper/lower extremity node sites
|
axillary
epitrochlear popliteal inguinal |
|
|
what is the size of a "good node"?
|
1 cm or less
|
|
|
things to assess and document about palpable nodes
|
Location (bilateral or unilateral)
Size Consistency (soft, firm, hard, smooth, nodular) Quantity (discrete or matted) Mobile or fixed Tenderness Warmth, erythema Changes over time (requires multiple assessments) |
|
|
what is a rosenbaum and how far away do you hold it?
|
it's a small snellen chart. hold at 14 inches.
|
|
|
what is the range of a snellen chart?
|
largest line of characters (20/200)
smallest line of characters (20/10) |
|
|
instructions for using snellen chart
|
Allow the patient to use their glasses or contacts
Stand 10 or 20 feet in front of the eye chart Cover one eye at a time with a card Ask the patient to read progressively smaller lines of letters until they get some incorrect. Record the smallest print successfully read 100% Repeat with the other eye. |
|
|
how would you interpret 20/40 vision?
|
what the normal eye can read at 40 feet, this person's eye reads at 20 feet.
|
|
|
what snellen score usually warrants glasses?
|
20/40 or 20/50
|
|
|
what does PERRLA stand for?
|
– Pupils equal, regular, and react to light and accommodation
|
|
|
give the brief sequence of events for a HEE(NT) exam. (big picture, with materials)
|
sit pt. on end of exam table
examine from right side Head Inspection Neck Inspection Lymph Node assessment (head, neck, upper/lower extremities) Eyes: snellen, rosenbaum, cover, penlight. Ears: using otoscope |
|
|
Sequence for HEENT eye test
|
1. Test distant vision (Snellen chart, E chart)
2. Test near vision (Rosenbaum chart or Jaeger card) 3. Assess PERRLA 4. Assess corneal light reflex (5. Perform the cover/uncover test) 6. Test cardinal fields of gaze (holding chin) |
|
|
How do you assess PERRLA?
|
note shape (round is normal, oval is abnormal)
note relative size note reaction to light by constriction note consensual reaction (+ is normal) accomodation - give pt. a distance target, then ask them to look at near target, look for smoothness and symmetry. |
|
|
How do you assess corneal light reflex?
|
square up with pt., ask them to look directly in between my eyes.
shine light in between their eyes, checking for symmetry of reflection. CN III, IV, VI |
|
|
with what condition would the corneal light reflex be diminished?
|
cataracts
|
|
|
how do you perform the cover/uncover test?
|
cover one eye and you should observe NO MOVEMENT in the uncovered eye.
|
|
|
3 types of urinary diversions
|
1. ileal conduit - bowel resection to provide "tube" for ureters to empty into. leads out to a stoma. continuous flow.
2. continent urostomy (Kock pouch). bowel resection that allows for a urine reservoir that is emptied by catheterizing the stoma. 3. Mitrofanoff procedure. appendix is used to connect the bladder to the surface of skin and is used to form a stoma. allows self-care. |
|
|
what pop is mucus in the urine a normal finding for?
|
those with urinary diversions, as the resected bowel continues to produce mucus.
|
|
|
what should you check upon removing a catheter?
|
check the post-void residual using a bladder scanner.
|
|
|
risk factors for urinary retention
|
Vaginal prolapse
Prostatitis Abdominal surgery Hypotonic detrusor muscle Anticholinergic medications Pain medications |
|
|
what causes urinary stasis?
|
bladder stones
UTI |
|
|
what is the hallmark of urinary retention?
|
voiding small amounts frequently (5-10 ml)
|
|
|
where should you point the bladder scanner?
|
at the coccyx
|
|
|
considerations for bladder scan accuracy
|
Morbid obesity
Inadequate ultrasound gel Improper aim of scanhead Moving the probe during the scan Presence of an indwelling urethral catheter Does enable the detection of a blocked catheter Scar tissue**, incisions, sutures, and staples can affect ultrasound transmission and reflection Program for gender |
|
|
what population uses straight catheters?
|
autonomous neurogenic bladder (spinal cord lesion).
|
|
|
most common catheter size?
|
16 Fr
|
|
|
what do you document with a catheter instillation?
|
Size and type
Amount in balloon U/O (initial) C&S obtained? Tolerance of procedure Start I&O |
|
|
talk through bladder irrigation procedure
|
clamp the catheter!
Irrigate through port Solution: Use room temp solution Use an 18G needle Instill 30-60mL slowly |
|
|
what would you document when irrigating a bladder?
|
Amount & type of irrigant
Characteristics of drainage Ease of irrigation Pt tolerance + make sure to subtract irrigant volume from U/O |
|
|
2 important things to remember about changing colostomy bags
|
A. push the skin away, don't pull the bag.
B. pat skin dry after cleaning |
|
|
colostomy or ileostomy ring: how large do you cut it?
|
no more than 1/8" larger than the stoma.
|
|
|
where do you plug in a piggyback?
how is the rate controlled? |
above the clamp on the primary line.
(proximal port) clamp on the main line controls the rate. |
|
|
talk through IV push procedure.
|
saline flush
clamp primary line (so med doesn't travel up) scrub port screw on luer check blood return instill slowly, noting pt. reaction. saline flush at same rate as med push. |
|
|
describe a mini-infusion pump
|
also called a syringe pump. often used in pedi.
can go in distal port of primary line or in saline lock. |
|
|
talk through the use of a volume-control infusion
|
Fill burrette (volume controlled infusions)
Air vent is open Add med & label Gently rotate Attach to distal port on primary line Adjust flow rate on burrette tubing |
|
|
things to know about blood transfusions
|
2 nurses do ID checks
equipment: Y-set, NORMAL SALINE, blood, Blood must be infused within 4 hours of leaving the blood bank. stay with pt. for first 5-10 min in case there's a rxn |
|
|
signs of hemolytic reaction during blood transfusion
|
chills
tachycardia decrease bp fever tachypnea H/A chest pain apprehension |
|
|
what would you do in response to any reaction (be it hemolytic, allergic, or febrile) during a blood transfusion?
|
stop infusion and switch to normal saline at KVO rate.
|
|
|
drip rate calculation:
drops/min = |
Drops/min = total volume to be infused X drop factor / Time in minutes
|
|
|
units for drop factor?
|
gtts/ml
|
|
|
3 reasons for use of an NG tube
|
Enteral nutrition
Lavage (irrigating stomach) Decompression |
|
|
reasons for using decompression
|
1. Rest GI tract
-Severe vomiting and diarrhea 2. Monitor GI bleeding 3. Clear GI tract -Promote healing and allow peristalsis to resume |
|
|
2 NPO thirst remedies
|
oral hygiene (lemon toothettes)
a few ice chips |
|
|
2 types of NG tubes to know
|
1. Single lumen (Levine tube), can be used for intermittent suction. CANNOT be used for continuous suction.
2. Double lumen (Salem sump), CAN be used for continuous suction. Offsets the pull of the suction. |
|
|
talk through the NG tube placement procedure
|
Pre-assessment
Measuring…nose-tip of ear – xiphoid Position patient >45 degrees, hyperextend head slightly Advancing tube (only on swallow); chin tuck here. Secure tube |
|
|
what do we document after NG tube placement?
|
Type and size of tube
Nare used Stomach contents characteristics pH Patient response Teaching that was done |
|
|
what kind of tube requires a CXR?
|
nasoenteric tube
|
|
|
what are the pHs of the stomach, lungs, and intestines?
|
pH of stomach contents less than 5.5.
pH of lungs >6.0 Intestines >7.0 |
|
|
what must you do before medicating through an NG tube?
|
irrigate to assure patency.
|
|
|
what should you do with new nausea in a pt. with an NG tube?
|
check suction, irrigate NG tube to make sure its not blocked.
|
|
|
NG irrigation procedure
|
Use isotonic solution
1. Instill irrigant gently 2. Inject air into vent (pigtail - the blue one) Subtract irrigant from NG output |
|
|
where should the suction container be?
|
below the level of the stomach
|
|
|
where should the pigtail vent (blue vent) be?
|
the pigtail vent should be above the level of the stomach.
|
|
|
procedure for removing NG tube
|
Check physician’s order for removal of nasogastric tube.
Explain procedure to patient and assist to semi-Fowler’s position. Gather equipment. Perform hand hygiene. Don clean disposable gloves. Place towel or disposable pad across patient’s chest. Give tissues to patient. Discontinue suction and separate tube from suction. Unpin tube from patient’s gown and carefully remove adhesive tape from patient’s nose. Attach syringe and flush with 10 mL normal saline solution or clean with 30 to 50 cc of air. (optional). Instruct patient to take a deep breath and hold it. Clamp tube with fingers by doubling tube on itself. Quickly and carefully remove tube while patient holds breath. Place tube in disposable plastic bag. Remove gloves and place in bag. Offer mouth care to patient and facial tissues to blow nose. Measure nasogastric drainage. Remove all equipment and dispose according to agency policy. Perform hand hygiene. Record removal of tube, patient’s response, and measure of drainage. Continue to monitor patient for 2 to 4 hours after tube removal for gastric distention, nausea, or vomiting. |
|
|
what is Xanthelasma?
|
cholesterol deposits under the eyes. sign of atherosclerosis.
|
|
|
how do we evaluate the carotid arteries?
|
auscultate for bruits
palpate for strength |
|
|
how do you evaluate for JVD?
|
jugular vein distension
sit them up to 45 degree angle, shine light from behind inspect for distension or pulsation. evidence for compromised right side of heart. |
|
|
what do you inspect the precordium for?
|
thrills (cat purring)
lifts (will lift your hand w/ heartbeat) pulsations |
|
|
what's the significance of erb's point?
|
it's the point at which the lub-dub is of equal intensity
|
|
|
auscultation and positioning sequence
|
A. Pt leaning slightly forward in expiration: Listen with the diaphragm at all 5 landmarks
B. Pt supine: Listen with the diaphragm at all 5 areas C. Pt rolled to a left lateral position: Listen with the bell at all 5 areas |
|
|
stenosis vs. insufficiency. which is more associated with opening problems?
|
stenosis is more associated with opening.
insufficiency is associated with closing problems (think floppy) |
|
|
murmur grading scale
|
Grade I - Barely audible with a stethoscope in a quiet room
Grade II - Quiet but clearly audible with a stethoscope Grade III - Moderately loud (like S1 or S2) Grade IV - Loud, associated with a thrill Grade V - Very loud, thrill easily palpable Grade VI - Extremely loud, audible with the stethoscope not in contact with the chest, thrill palpable and visible you need a scope for the first 4 grades.by grade 5, you can palpate a thrill |
|
|
4 elements of peripheral vascular assessment
|
1. Inspect arms and legs
-Color -Hair distribution -Texture & moisture -Edema -Venous patterns -Lesions 2. Palpate for temperature 3. Palpate pulses -Symmetry -Strength -Rate -Patency 4. Test capillary refill |
|
|
what's the difference between peripheral arterial disease and peripheral venous disease?
|
peripheral arterial disease is occlusion and sclerosis of arteries.
venous disease is the varicosity of veins, which impedes flow. |
|
|
signs and symptoms of venous disease?
|
hair present on extremities, edema, warm to touch, strong pulses, pruritis, aching and cramping pain.
|
|
|
signs and symptoms of arterial disease
|
hair absent on extremities, cool to touch, weak pulses, no edema, cap refill greater than 3 sec, sharp stabbing pain. *claudication*
|
|
|
where is S1 loudest?
|
mitral area. (5th ICS)
|
|
|
where is S2 loudest?
|
aortic area. (2nd ICS)
|
|
|
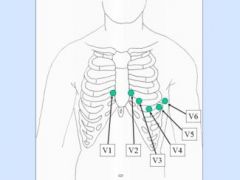
placement for 12 lead EKG
|
V1: 4th ICS RSB
V2: 4th ICS LSB V3: Between V2 and V4 V4: 5th ICS Left MCL V5: 5th ICS Left AAL V6: 5th ICS Left MAL 4 limb leads |
|
|
EKG lead placement
|
|
|
|
3 lead ECG mneumonic
|
white on right.
smoke over fire. |

