![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
143 Cards in this Set
- Front
- Back
|
What is the definition of a macule?
|
Small spot
Not palpable < 1 cm |
|
|
What is the definition of a patch?
|
Large spot
Not palpable > 1 cm Can arise de novo, or as a coalescence of macules |
|
|
What is the definition of a papule?
|
Small bump
Superficial Elevated < 1 cm |
|
|
What is the definition of a plaque?
|
Large bump
Superficial Elevated >1 cm Can arise de novo, or as a coalescence of papules |
|
|
What is the definition of a nodule?
|
Significant deep component
Small bump < 1 cm |
|
|
What is the definition of a tumor?
|
Significant deep component
Large bump > 1 cm |
|
|
What is the definition of a vesicle?
|
Small bubble
Fluid-filled Usually superficial < 0.5 cm |
|
|
What is the definition of a bulla?
|
Large bubble
Fluid-filled Can be superficial or deep >0.5 cm |
|
|
What is the definition of a pustule?
What are the sub-categories of pustules? |
Pus-containing bubble
Often categorized according to whether or not they are related to hair follicles ◊ Follicular - generally indicative of local infection ► Folliculitis - superficial, generally multiple ► Furuncle - deeper form of folliculitis ► Carbuncle (boil) - deeper, multiple follicles coalescing ◊ Non-follicular - may indicate systemic infection |
|
|
What is the definition of a cyst?
|
A sac containing fluid or semisolid material (cells or cell products).
|
|
|
What are the components of the morphological description of a skin lesion/condition?
|
• Type of lesion (primary or secondary)
• Color, shape, texture • Configuration (e.g. linear, annular, arcuate, zosteriform) • Distribution, location |
|

What kind of condition causes a targetoid skin lesion?
|
Erythema multiforme
- this condition is sometimes used synonymously with Steven Johnson syndrome, but they're probably not the same (uptodate). - can be caused by herpes virus, and Mycoplasma |
|
|
What special skin exam is used for dermatophyte and yeast infections?
|
KOH microscopic examination
|
|
|
What special skin exam is used for tinea capitis, erythrasma, and vitiligo?
|
Woods' light (UVA)
|
|
|
What special skin exam is used for herpes simplex, zoster, and varicella?
|
Tzanck smear
|
|
|
What special skin exam is used for syphilis?
|
Darkfield examination
|
|
|
What special test is used to identify scabies?
|
Oil microscopy.
|
|
|
What infection causes tinea capitis?
|
Dermatophyte infection of the scalp. The most common pathogen in BC is Microsporum canis.
Second most common is Trichophyton tonsurans. |
|
|
What is lichenification?
|
It is a secondary skin lesion.
Increase in skin lines/creases produced by chronic rubbing. |
|
|
What is maceration?
|
Raw, moist, wet tissue.
|
|
|
What is excoriation?
|
Loss of skin due to scratching or picking.
|
|
|
What is another name for blackhead/whitehead?
|
Comedone.
- blackhead means open follicle. - whitehead means closed follicle. |
|
|
What is the name of a scar that has extended beyond the wound's boundaries, and is chronic in nature?
|
Keloid.
|
|
|
What is a milium?
|
Small, superficial cyst, containing keratin (usually 1-2 mm in size).
|
|
|
Inherited disease where there is impaired ability to repair DNA damage such as that induced by UV light, and death from skin cancer is common.
|
Xeroderma pigmentosum.
|
|
|
What wavelengths are UVA, UVB and UVC?
|
UVA - 320-400 nm
UVB - 290-320 nm UVC - up to 290 nm |
|
|
The two types of melanin are...
|
Eumelanin, which is protective, and found in all races. Blacks have larger melanosomes, which has a greater protective effect.
Phaeomelanin, which is ineffective at blocking UV light. Found in red-headed individuals. |
|
|
What are the variants of basal cell carcinoma?
|
-Superficial spreading
-Nodular -Sclerosing -Pigmented |
|
|
What is the name of a precancerous lesion that turns into squamous carcinoma of the skin?
|
Actinic keratosis. A superficial pink, scaling patch.
|
|
|
Treatment for actinic keratosis.
|
- Liquid nitrogen cryotherapy.
- Topical 5-fluorouracil. |
|
|
Treatment of squamous cell carcinoma.
|
1. Surgical excision.
2. Radiation therapy. |
|
|
Treatment of basal cell carcinoma.
|
1. Electrodessication and curettage
2. Simple surgical excision 3. Micrographic surgery 4. Radiation therapy |
|
|
How large of a dose of UV light exposure is needed to significantly increase the risk of...
BCC? SCC? Malignant melanoma? |
BCC and malignant melanoma - low doses of UVB, childhood exposure is important to later life risk.
SCC - very large amount of UV light is needed. |
|
|
What is the normal progression of a benign nevus?
|
Junctional -> compound -> dermal nevus.
|
|
|
What is the most significant predictor of melanoma risk?
|
The number of nevi.
> 100 nevi suggests melanoma risk of 1 in 10. |
|
|
Autosomal dominant trait for tendency to develop many atypical nevi.
|
Dysplastic nevus syndrome.
|
|
|
Variants of melanoma
|
Superficial spreading melanoma
- evolves from atypical nevi. Nodular melanoma - arises without precursor lesion. Lentigo maligna melanoma - arises in expanding brown patch (lentigo maligna). |
|
|
Treatment for melanoma
|
1. Surgical excision with 1-3 cm margin.
2. Chemotherapy if there is systemic involvement. |
|
|
What agent is good for blocking UVA?
|
Parsol 1789.
|
|
|
What are the main components of the basement membrane zone of skin (between epidermis and dermis)?
|
- Type IV collagen
- Laminin |
|
|
What are the skin appendages?
|
• Hair
• Sebaceous glands • Sweat glands |
|
|
Layers of the epidermis
|
Stratum corneum
Stratum granulosum Stratum spinosum Stratum basale |
|
|
Innervation of eccrine sweat glands.
|
- Sympathetic cholinergic nerve fibres.
- Also respond to blood-borne adrenergic stimuli during exercise. |
|
|
What are the sub-types of psoriasis?
|
PIPEG
Psoriasis vulgaris (plaque psoriasis) Inverse psoriasis Pustular psoriasis Eryrthrodermic psoriasis Guttate psoriasis |
|
|
Cardinal morphological features of psoriasis vulgaris.
|
1. Plaque
2. Well-circumscribed margins 3. Silver scale 4. Salmon colour (bright, red) 5. Symmetric distribution |
|
|
Patient with pustular rash, fever, leukocytosis.
|
Generalized pustular psoriasis should be on the ddx.
Also known as von Zumbusch. |
|
|
Clinical features of lichen planus
|
- Papules 2-5 mm
- Polygonal - Purple - Planar - Pruritus - Wickham's striae - white lines on surface. - Buccal mucosal lacy white reticular lesions. |
|
|
What is the most common malignancy in all of North America?
|
Basal cell carcinoma.
|
|
|
What is easier to diagnose with small fragmented biopsies - BCC or SCC?
|
BCC can be diagnosed with small, fragmented biopsies.
SCC is hard because it could be confused with benign reactive hyperproliferation of the epidermis. |
|
|
Seborrheic keratosis
- benign or potentially malignant? - pathological features? |
Completely benign.
Pathologic features - epidermal cysts containing keratin. - melanin within tumor keratinocytes. - epidermal thickening. |
|
|
What is the mnemonic for diagnosing melanoma?
|
• Asymmetry
• Border irregular • Color □ Black (upwards spread of melanocyte tumor cells) □ Blue (melanin in the deep dermis) □ Red (dermal inflammation or vascular proliferation) □ White (fibrosis) • Diameter is 6 mm or greater. |
|
|
Which direction are melanocytes spreading in malignant melanoma - upwards into the stratum corneum, or downwards into the dermis?
|
Up into stratum corneum.
|
|
|
What are the 3 different growth patterns of hemangiomas?
|
• Large, rapidly growing tumours in infancy.
□ Strawberry angioma = infantile capillary hemangioma. • Small , rapidly growing ulcerating tumours at any age. □ Pyogenic granuloma • Small, slowly growing tumours in adulthood. □ Senile angioma = cherry angioma = Campbell de Morgan spot. |
|
|
Major differences between tinea corporis and tinea versicolor
|
Tinea corporis
- caused by fungi that are not part of normal flora. - hyperkeratosis and parakeratosis -> prominent scales. - inflammatory. - few organisms seen on KOH prep. Tinea versicolor - caused by Malassezia furfur, a part of normal flora. - hyperkeratosis, no parakeratosis -> fine, subtle scales. - non-inflammatory. - numerous organisms seen on KOH prep. |
|
|
What skin appendages form the pilosebaceous unit?
|
1. Hair follicle.
2. Arrector pili muscle. 3. Sebaceous glands. 4. Apocrine glands. |
|
|
What method of secretion do sebaceous glands use?
|
Holocrine secretion.
|
|
|
What are the layers of the internal root sheath of a hair follicle?
|
Inner layer is Huxley's layer. Consists of stratum corneum and granulosum.
Outer layer is Henle's layer. Consists of stratum spinosum and basale. |
|
|
Main functions of melanin.
|
• Protection from UV radiation.
• Scavenges cytotoxic radicals. • Neurologic development. |
|
|
Embryological origin of keratinocyte.
|
Ectoderm.
|
|
|
Embryological origin of melanocyte.
|
Neural crest.
|
|
|
Embryological origin of Langerhans cells.
|
Dendritic monocyte-macrophage derived from bone marrow.
Mesoderm origin. |
|
|
Where are Merkel cells found in the body?
What is their function? |
• Palms and soles, and in mucous membranes of lips and oral cavity.
• May serve as sensory receptors, as they are associated with free nerve endings. |
|
|
What are the two different types of nerve endings' functions in the dermis of the skin?
|
• Encapsulated nerve endings
• Sense of touch. • Free nerve endings • Pain. • Temperature sensation. |
|
|
Which part of the body do sebaceous glands empty into surface of skin, rather than into hair follicles?
|
Lips, eyelids, nipples, glans penis.
|
|
|
What are the specialized glands of the external ear and eyelids called?
|
• Ceruminous glands - specialized apocrine glands of external ear.
• Moll's glands - specialized apocrine glands of eyelid. |
|
|
Loss of what kind of fibers in which layer of the skin causes wrinkles?
|
Loss of elastic fibers in the papillary dermis.
|
|
|
What type of collagen are anchoring fibrils in the basement membrane zone in the dermal-epidermal junction made of?
|
Type VII collagen.
|
|
|
Differences in function between Meissner corpuscles and Pacinian corpuscles
|
Meissner corpuscles
• Mechanoreceptors that mediate touch. Pacinian corpuscles • Deep pressure receptors. |
|
|
What kind of skin contains specialized nerve end organs like Pacinian and Meissner corpuscles - thin or thick skin?
|
Thick skin. Especially in palms and soles.
|
|
|
The single most common location for melanoma to occur in women is:
|
Legs
|
|
|
What does chronic sun exposure do to the Langerhans cells in the epidermis?
|
Langerhans cells decrease in number
|
|
|
What skin disease demonstrates spongiosis pathologically?
|
Eczema.
Spongiosis is increased spaces between the keratinocytes caused by intraepidermal intercellular edema |
|
|
Name the different forms of eczema.
|
• Atopic dermatitis - hereditary
• Irritant contact dermatitis - induced by contact with certain chemical irritants. • Allergic contact dermatitis - Induced by contact with allergens. • Asteatotic eczema - excessive drying of the skin. • Stasis dermatitis - venous insufficiency in the legs. |
|
|
What infection causes Scarlet fever?
|
Streptococcus.
|
|
|
What antibiotics are most commonly used to treat acne?
|
Tetracyclines
|
|
|
The most common cause(s) of allergic contact dermatitis in the general population is:
|
Nickel
|
|
|
Which tinea infection requires the longest and most aggressive course of treatment?
|
Tinea unguium generally requires a minimum of oral therapy and a 12 week course for treatment.
|
|
|
What virus causes herpes zoster?
|
Varicella zoster.
Another name for herpes zoster is shingles. |
|
|
What skin disease causes coarse keratohyaline granules and koilocytosis in keratinocytes?
|
Warts
Note that koilocytosis means perinuclear vacuolation. |
|

What is the cause of roseola infantum?
|
Aka sixth disease.
Caused by human herpes virus 6. After a child's fever abates, a maculopapular rash, starting on neck and trunk and spreading to face and extremities. |
|
|
What is the principal chemical difference between the protein of the nail plate and the stratum corneum?
|
Nail plate has increased sulfur content. It is cross-linking between sulfur moieties which increases the hardness of cutaneous proteins of the nail plate.
|
|
|
Which virus has been linked to Kaposi's sarcoma?
|
Human herpes virus 8.
|
|
|
What is the MOA of retinoic acid for treatment of acne?
|
Topical retinoic acids:
• Promotes desquamation of keratinized layers. Systemic Isotretinoin • Reduces sebaceous gland size and reduces sebum production; regulates cell proliferation and differentiation |
|
|
What are the variant forms of acne?
|
Childhood acne
- neonatal - infantile - early onset acne vulgaris Follicular occlusion triad - acne conglobata - hidradenitis suppurativa - dissecting cellulitis of the scalp Acne fulminans Acne excoriee |
|
|
Which skin disease are mediated by Th1 model, and which one(s) are mediated by the Th2 model?
|
Th1 - psoriasis
Th2 - atopic dermatitis |
|
|
Ddx for vesicular and vesiculobullous eruptions.
|
• Herpes Simplex I and II
• Varicella • Herpes Zoster • Impetigo • Bullous insect bite reaction • Primary skin bullous disorder. E.g. pemphigus, pemphigoid. |
|
|
Ddx for follicular eruptions.
|
• Pityrosporum folliculitis
• Pseudomonas folliculitis • Staphylococcus folliculitis • Acne |
|
|
Ddx for annular and scaling eruptions.
|
• Tinea corporis
• Tinea versicolor • Secondary syphilis • Psoriasis • Nummular eczema • Pityriasis rosea |
|
|
Ddx for papular eruptions.
|
• Verruca
• Molluscum contagiosum • Insect bites |
|
|
Ddx for eczematous and pruritic eruptions.
|
• Scabies
• Pediculosis corporis (louse infestation) • Insect bites • Eczema |
|
|
Ddx for scalp eruptions.
|
• Tinea capitis
• Pediculosis capitis (head lice) • Psoriasis • Seborrheic dermatitis |
|
|
Ddx for intertrigo.
|
• Tinea cruris (jock itch)
• Candida • Erythrasma • Inverse psoriasis |
|
|
Pathogenesis of seborrheic dermatitis.
|
• Involves sebum production and Pityrosporum fungus.
• Located at sites of increased sebaceous gland density and activity. • Pityrosporum - Lipophilic yeast that thrives on lipids in sebum. • Scaling and inflammation seen clinically is due to host response to Pityrosporum. |
|
|
Pathogenesis of pityriasis rosea
|
• May be due to human herpes virus 7.
• Eruption typically evolves over 6-8 weeks • Development of herald patch, a solitary 2-6 cm scaly plaque. • This is the first patch, but is a sign of more to come. • Eruption of multiple 1-2 cm oval annular papules with fine "collarette" scaling along rim of individual lesions. • T-shirt and shorts distribution. • Pruritus is variable. |
|
|
Etiology and clinical appearance of molluscum contagiosum.
|
Etiology: Pox virus transmitted via skin to skin contact.
Skin coloured, umbilicated papules. |
|
|
What is a seborrheic keratosis?
|

Idiopathic, benign tumour of the skin that increases with age.
Cysts that contain keratin. Keratinocytes take up more melanin, giving brown color. |
|
|
Which layer of the epidermis contains keratohyalin granules?
Which layer is linked by desmosomes? |
Stratum granulosum contains the keratohyalin granules.
Stratum spinosum is linked by desmosomes. |
|
|
How many days does it take for a keratinocyte to go from the stratum basale layer to the corneum layer?
|
25-30 days
|
|
|
Why exactly do dark skinned races have dark skin?
|
It is NOT an increase in number of melanocytes. It is an increased production of melanin, which is then transferred to keratinocytes.
|
|
|
What is the name of the granules contained in Langerhans cells? What is their purpose?
|
Birbeck granules. Degrades antigen.
|
|
|
What is a glomus body?
|
Arteriovenous shunt located in the reticular dermis within the deep dermal capillary plexus. When the skin is exposed to cold, the shunt will open up and allow arteriolar blood to shunt into venules, bypassing the superficial dermal capillary plexus.
|
|
|
Hair follicles are divided into 3 segments. What are these 3 segments?
|
Follicular infundibulum
□ From opening of hair follicle to opening of sebaceous duct Follicular isthmus □ From opening of sebaceous duct to insertion of arrector pili muscle Inferior segment □ Extends to the base of the follicle |
|
|
What is the method of secretion for
- eccrine sweat glands? - sebaceous glands? |
Eccrine sweat glands - merocrine
Sebaceous glands - holocrine The difference: * Apocrine glands - a portion of the plasma membrane buds off the cell, containing the secretion,an example is fat droplet secretion by mammary gland. * Holocrine glands - the entire cell disintegrates to secrete its substance,an example is sebaceous glands for skin and nose. * Merocrine glands - cells secrete their substances by exocytosis an example is pancreatic acinar cells. |
|
|
What are the three segments of the eccrine gland's excretory duct?
|
1. Convoluted duct
2. Straight dermal component 3. Acrosyringium |
|
|
What does an SPF of 30 in a sunscreen mean?
|
It takes 30x the amount of time to get erythema when you have the sunscreen on.
|
|
|
Name the three growth phases of the hair follicle. How many scalp hairs are in each phase at any time?
|
Anagen - 90% of your hairs on your head
- Active growth phase - 1000 days on scalp - 28 days on eyebrows Catagen - 1% - Apoptosis - Lasts 2 weeks Telogen - 9% - Resting phase - Lasts 100 days - Hairs can be easily tugged out during this phase |
|
|
On a hair pull test, how many hairs is hair loss?
|
6+ hairs is considered hair loss.
|
|
|
Which drugs can cause telogen effluvium?
|
Metoprolol
Antithyroid drugs Valproate |
|
|
List the non-scarring hair loss and the scarring hair loss diseases.
For the non-scarring hair loss, also say which ones come out at the root, and which ones are breakages. |
Non-scarring
-Androgenetic alopecia (root) -Alopecia areata (root) -Anagen effluvium (root) -Telogen effluvium (root) -Tinea capitis (breakage) -Trichotillomania (breakage) Scarring hair loss -Lichen planopilaris -Discoid lupus erythematosus hair loss |
|
|
What is the rate of growth of nails (per week)?
What grows faster - toenails or fingernails? |
0.5-1.2 mm / week.
Fingernails grow faster. |
|
|
What is the angle between the nail plate and adjacent skin called?
|
Lovibond's angle
|
|
|
What organism is the most common cause of onychomycosis?
|
Trichophyton rubrum
|
|

|
Beau's grooves - a horizontal depressed line on nail plate that occurs after severe illness such as MI, high fever, malnutrition.
|
|
|
What causes "white banding of the nails"?
What causes "brown banding of the nails"? |
White:
- Occurs in hypoalbuminemia, which accompanies chronic hepatic or renal failure. Brown: - If vertical - nevus or melanoma - If horizontal - Addison's or chemotherapy |
|
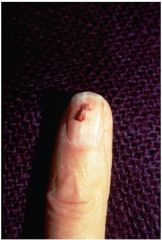
What is this caused by?
|
This is a splinter hemorrhage, caused by bacterial endocarditis, trichinosis, and sometimes just in normal people.
|
|
|
What is the group of hereditary skin disorders that causes fish-like scaling of the skin, due to abnormal epidermal cell differentiation?
|
Ichthyosiform dermatoses
|
|
|
What are the protein contents of keratohyalin granules?
|
Keratin
Profilaggrin, which gets cleaved to form filaggrin, a protein which aids in assembly of final keratin |
|
|
Pathogenesis of bullous pemphigoid
vs Pathogenesis of pemphigoid vulgaris |
Bullous pemphigoid - antibodies to hemidesmosome proteins, which help anchor epidermis to the basement membrane. Bullae are tough, with few erosions. Death is unusual.
Pemphigoid vulgaris - antibodies to proteins that hold keratinocytes together. Blister/split occurs between stratum basale and stratum spinosum. Bullae are fragile, can rupture, and result in death. |
|
|
What is the cause of immediate tanning, and delayed tanning?
|
Immediate tanning - UVA, oxidizes and redistributes melanosomes.
Delayed tanning - UVB damages DNA, which increases melanocytes, melanosomes, and dendricity. |
|
|
What causes a skin lesion that is described as a "dewdrop on a rose petal"? It may start off as papules, which later become vesicles. Has Christmas tree distribution.
|
Varicella
|
|
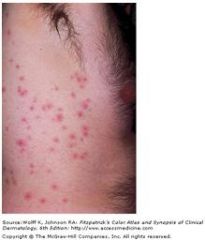
These lesions occurred after using a hot tub 3 days ago. What causes it?
|
Pseudomonas folliculitis
|
|

What disease is this?
|
Tinea corporis (ringworm)
- Trichophyton rubrum, or Microsporum canis |
|

What disease is this?
|
Tinea versicolor
- Malassezia furfur |
|
|
What is condyloma lata?
|
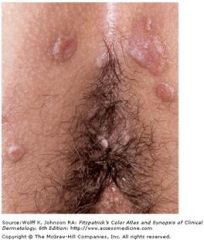
When secondary syphilis appears in moist areas, such as mouth and anogenital area.
They are soft, flat-topped, reddish pale papules. |
|
|
What are the variants of tinea capitis?
|
Ectothrix - infection outside hair shaft (Microsporum canis)
Endothrix - infection within hair shaft (Trichophyton tonsurans) Kerion - variation of endothrix, with inflammatory plaques |
|
|
What causes pediculosis corporis? What sort or secondary infections are possible?
|
Louse infection.
Can transmit trench fever and epidemic typhus. |
|
|
What are the organisms that cause tinea cruris?
|
Trichophyton rubrum
Trichophyton mentagrophytes |
|
|
What is the most common infecting organism that causes tinea unguium?
|
Trichophyton rubrum
|
|
|
What causes guttate psoriasis?
|
Group A Streptococcus
|
|
|
It psoriasis, how many days does it take for the keratinocyte to transit from basal layer to surface?
|
3-4 days, as opposed to the normal 28 days
|
|
|
What conditions often occur together in a patient with atopic dermatitis?
|
Conjunctivitis (allergic)
Hayfever Asthma |
|
|
What is the difference in pathogenesis between seborrheic keratosis and seborrheic dermatitis?
|
Seborrheic keratosis - benign tumours of keratinocytes and melanocytes.
Seborrheic dermatitis - sebum production attracts Pityrosporum infection. |
|
|
What is parakeratosis?
|
Remnants of nuclei in the stratum corneum
|
|
|
What is Auspitz's sign?
|
It is when you peel off a scale of psoriasis, it starts to bleed because the vessels are close to the surface.
|
|
|
Differences between acne and rosacea.
|
Acne
-comedones -adolescents -pathogenesis is keratin blocking follicular opening, ↑sebum, and Proprionibacterium acnes Rosacea -erythema, telangiectasia -mostly middle aged women -pathogenesis unknown, but vascular in origin |
|
|
What is rhinophyma?
|
Late stage of rosacea, causing sebaceous hyperplasia and fibrosis on nose.
|
|
|
List the subtypes of rosacea.
|
1. Erythematotelangiectatic rosacea
2. Papulopustular rosacea 3. Phymatous rosacea 4. Ocular rosacea |
|
|
What are the three pillars of management for psoriasis?
|
Cream - steroids, retinoid, salicylic acid
Phototherapy - UVB or PUVA Systemic therapy - methotrexate, oral retinoid, cyclosporine, biologics |
|
|
What is squamous cell carcinoma in situ of the skin called?
|
Bowen's disease.
Can be caused by drugs, among other things. |
|
|
What is it called when you have hairs with nodules that break easily at those points? Microscopically, it looks like 2 brooms coming together.
|
Trichorrhexis nodosa.
Caused by lack of copper. |
|
|
What is the main treatment of choice for rosacea?
|
Systemic antibiotics - minocycline
|
|
|
What is the margin needed for an excision biopsy of melanoma?
How about for surgical excision with intent to cure? |
0.5 cm, need 1:3 width:length ratio to prevent dog-ears when suturing. Deepness to subcutaneous layer.
Intent to cure: - If depth > 2 mm → 2 cm around, and down to fascia - If depth 1-2 mm → 2 cm if you can, but have option to do between 1-2 cm - If depth < 1 mm → 1 cm around |
|
|
What is used for T staging of melanoma?
|
Breslow staging. Measured from stratum granulosum down.
< 1 mm, 5 year survival 95-100% 1-2 mm, 5 year survival 80-96% 2.1-4 mm, 5 year survival 60-75% > 4 mm, 5 year survival 50% |

