![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
Infertility Definition
|
“the inability of couples to conceive a pregnancy after a year of unprotected intercourse, or the inability to carry a pregnancy to term”
Under 35 and trying to conceive for 12 months Over 35 and trying to conceive for 6 months |
|
|
Age Factor
|
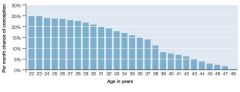
|
|
|
Preconception - History
|
Smoking
EtOH Other drugs Medications Family history genetic problems / ethnicity (consider targeted genetic tests – CF etc) |
|
|
Preconception - Examination
|
WOMEN:
BMI BP Breast Pelvic (at PAP) MAN: BMI Testicular examination at least once in adulthood |
|
|
Preconception Investigations - Women
|
PAP (+/- Chlamydia & gonorrhea PCR)
Serology Rubella Varicella HBV HCV HIV Syphillis FBC +/- thalassaemia screen Bl Gp & Ab screen TSH Vitamin D ffer CF carrier testing Offer CF carrier testing (target Caucasians) |
|
|
TSH – why ?
|
Overt thyroid disease
Subclinical hypothyroidism incidence at least 1 in 500, increases with age Subclinical hypothyroidism - why treat? Increased demand for thyroxine in the mother – may convert compensated hypothyroidism to overt hypothyroidism Evidence of reduced neurological outcomes in children of mothers with hypothyroidism (3 studies) several years after birth |
|
|
Preconception Investigations – Men
|
Consider
HIV HBV HCV +/- Chlamydia & gonorrhea PCR |
|
|
Preconception Advice - Women
|
Immunisations current including:
Rubella (serology) Varicella (serology) Influenza Pertussis (Pneumococcal); Smokers, Asplenia, - as long as last vaccination > 5yrs ago & not had 2 previous doses, mpaired immunity, Chronic illness BMI Don’t smoke Minimal / no EtOH Folic acid / vitamins (Vit D, iodine) |
|
|
Preconception Advice - Men
|
Don’t smoke
BMI Pertussis immunity current |
|
|
Preconception Advice - Couple
|
Fecundity
Predicting ovulation Fertile time SI frequency Other myths |
|
|
Predicting ovulation
|
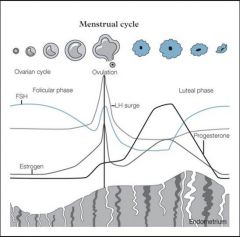
|
|
|
Fertile time
|
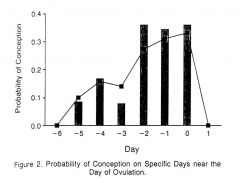
|
|
|
Predicting ovulation
|
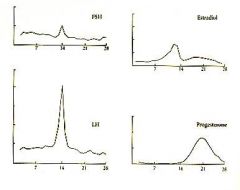
The BBT temperature rise follows ovulation and is useful only to confirm ovulation has taken place – and, over several cycles – to enable a prediction to be made of the likely day of ovulation for that woman in general.
To anticipate ovulation accurately you need all 3 hormones at each measurement. |
|
|
Predicting ovultion
|
1. estradiol dip: "mayeb baby)
2. LH surge: LH in urine (fortel) |
|
|
Degrees of fertility
|
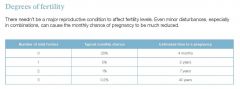
|
|
|
Infertility assessment – (GP)
|
Routine preconception as earlier
Women Previous pregnancies ? Ovulatory ? Risk previous tubal damage (STI, ectopics) ? Endometriosis – premenstrual spotting, secondary dysmenorrhoea, dyspareunia, family history Men History undescended testes, orchitis, trauma / torsion Both SI timing and frequency – ensure not contraceptive good sexula positions |
|
|
When to investigate infertility
|
Virtually always recommended Ix after 12 months infertility
85% conceive first 12 months 50% of the remaining do so in the next 12 months Thereafter pregnancy rates very low (10% per annum or less) |
|
|
What is Andrology?
|
From the Greek andros meaning ‘man’
Andrology is to men what gynaecology is to women |
|
|
investigation - Male
- semen |
Semen analysis: “SFA + IBT”
= Volume, concentration, motility, morphology and antisperm antibody screen Analysis, especially morphology very operator dependent Repeat if abnormal If repeating consider adding DNA fragmentation analysis if not previously done No need to repeat IBT (antibody screen) DNA fragmentation analysis SCIT SCSA |
|
|
Initial investigations - Female
|
Early follicular (day 2) FSH & oestradiol
Luteal (day 21) progesterone If irregular cycles / galactorrhoea Androgen screen (DHEAS, 17-OHP, FAI, testosterone) Prolactin Note am, fasting, not stressed, follicular if possible Above assumes preconception screen including TSH current Pelvic ultrasound Follicular phase Transvaginal Consider a HyCoSy |
|
|
form of fertility treatment
|
Intrauterine insemination (IUI)
Ovulation induction (OI) In vitro fertilisation (IVF) Intracytoplasmic sperm injection(ICSI) |
|
|
What is IVF?
|
In Vitro fertilisation – any fertilisation that occurs outside of the body
Originally devised to overcome blocked or absent fallopian tubes Now used to treat many factors: Irregular ovulation Low sperm count or motility Severe endometriosis Ovarian issues Unexplained infertility |
|
|
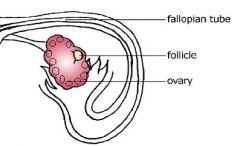
What's involved in fertility treatment?
|
Monitoring the menstrual cycle and ovulation
Blood tests for hormone levels – indicate the number and stage of egg development Vaginal ultrasound examinations to count and measure follicles on the ovary Depending on age, between 1-30 follicles will develop during a women's menstrual cycle In a natural cycle only 1 of these will develop to full maturity and be ovulated In fertility treatment the aim is to increase the number of follicles with mature eggs |
|
|
A typical patient experience with fertility treatment
|
Contact Genea nurses on first day of period
Start daily injections of FSH. Injections will last for 10-14 days During this stimulation period patients will attend clinic for 3-6 blood tests and ultrasounds to monitor follicle growth Start medication on about day 7 to suppress natural ovulation Once follicles reach 18-20 mm in diameter patient will take a trigger injection to mature the eggs |
|
|
Egg Retrieval
|

36 hours after the trigger injection patients attend day surgery for egg collection
|
|
|
Semen collection
|
On the day of egg pick up the male partner will collect his sample either at the clinic or at home
Also possible to collect and freeze sperm prior to egg collection |
|
|
Insemination
|
Insemination performed either by:
IVF – Sperm added to eggs in a dish ICSI – Sperm injected into egg directly by embryologist |
|
|
Embryo culture and development
|

|
|
|
Ultrasound guided embryo transfer
|
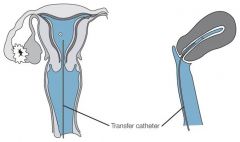
Usually on day 5 (or 6), less frequently on day 3
Committed to single embryos transfer to prevent multiple births Simple, relatively painless procedure performed in day surgery without any medication. Similar to pap smear. |
|
|
Embryo storage
|
Excess embryos are vitrified (frozen) for storage until required
Allows patients to have another embryo transfer without undergoing stimulation |
|
|
After embryo transfer – the “2 week wait”
|
Can be a difficult period for patients as they await their results – Genea counsellors offer support.
Endometrial support provided through doses of hCG or progesterone pessaries Blood pregnancy test performed 10 to 12 days after embryo transfer/16 days after egg collection day |
|
|
Chance of pregnancy
|
The chance of pregnancy will depend on:
Woman's age Reason for infertility Quality of the embryo transferred |
|
|
Antimullerian Hormone
|
Can perform anywhere in menstrual cycle
Can perform when on oral contraception Different assays in different laboratories – less of a problem now (mainly Gen II) Some intra-individual variation : best to repeat if big decisions are about to be made on it Shall I order it? Will it change behaviour or management Careful counseling especially in single women What would you do if it’s normal What would you do if it’s abnormal |
|
|
AMH- what do we know
|
Consistently the best predictor of oocyte reserve
Good predictor of response to IVF in terms of number of eggs Helpful for IVF dosing Predicts susceptibility of ovarian follicles to damage with chemotherapy |
|
|
AMH defining Normal
|
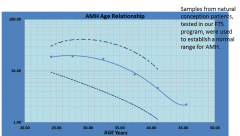
|
|
|
Low AMH for age
|
Earlier menopause likely
Narrowed window of opportunity for pregnancy Risk of poor response to IVF Narrowed window of opportunity for IVF to work Not necessarily less fertile or less likely to fall pregnant naturally (if not yet trying) Pathological concerns especially if markedly abnormal for age Genetic conditions? Endometriosis? Excludes PCOS |
|
|
High AMH for age
|
Associated with PCOS
Not (yet) a diagnostic criterion At risk of ovarian hyperstimulation High AMH in women over 40 IVF more likely to be successful AMH therefore may be useful to INCLUDE patients in to IVF but can it be used to EXCLUDE??? |
|
|
AMH – what we don’t know
|
Does a low AMH predict a low pregnancy rate with IVF (< 40 yrs)?
Does a low AMH predict miscarriage? Does AMH reflect egg QUALITY? |
|
|
AMH – useful indications (our opinion!)
|
Unexplained subfertility
Triage into keep trying vs moving to ART Older women considering IVF/oocyte freezing Suspected PCOS that doesn’t quite fit the diagnosis All women about to undergo IVF stimulation to get dosing right Counseling patients about to undergo chemotherapy Follow up of patients that have previously had chemotherapy |
|
|
Karyotype
|
? all infertile couples ?
or Targeted Men: severe oligozoospermia Women: POF, poor ovarian reserve Couples: recurrent miscarriage, recurrent IVF failure |
|
|
Fecundability
|
Fecundability - probability of
achieving pregnancy in one menstrual cycle (0.25 in the first 3 months and 0.15 during next 9 months) |
|
|
Prevalence of infertility
|
> 1 in 6 couples
> Female factors 37%, male factors in 8%, both in 35%, 5% unexplained > 15% conceive during investigations |
|
|
Anti-Mullerian hormone (AMH)
|
• Originally described in human fetal sexual
differentiation • Produced by granulosa cells of primary follicles / small follicles (not visible on ultrasound) • A reflection of total oocyte pool • Cycle independent • Does not necessarily relate to egg quality |
|
|
Causes of anovulation
|
• Polycystic ovary syndrome (PCOS)
• Hypothalamic disturbance (functional) • Hyperprolactinaemia • Primary ovarian failure • Other endocrine disease • Other - organic pituitary / hypothalamic |
|
|
Polycystic ovary
|
- 20% of the female population
- in combination with clinical/biochemical changes = polycystic ovary syndrome |
|
|
Effect of obesity on fertility
|
• Anovulation
• 50% more likely if BMI >25 • 300% more likely if BMI>30 • Increased hip-waist ratio alone also affects fertility in ovulating women • Adverse effect of insulin |
|
|
Tubal disease / anatomy
|
• Pelvic inflammatory disease (PID)
• STD • other • Previous surgery • Congenital anomalies |
|
|
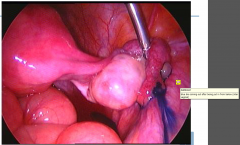
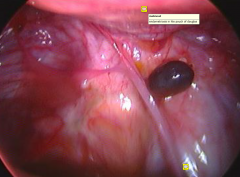
Laproscopy Normal
|

|
|
|
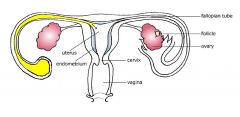
testing patency of the reproductive tract
|
|
|
|
Hydrosalpinx
|
can get back in and can upset the implantation phase (so better off to remove)
|
|
|
Hydrosalpinx Laproscopy
|
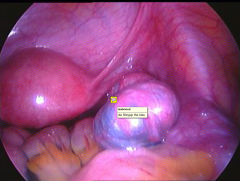
|
|
|
Adhesions
|
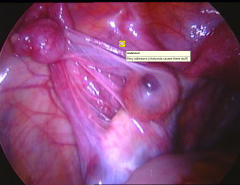
|
|
|
Submucous fibroids, Endometrial polyps
|

can affect fertility acting like an IUD
- can be surgically removed allowing the female a chance |
|
|
Endometriosis and infertility
|
• Prostaglandin production
• oocyte function • sperm transport • Autoimmune response • macrophage phagocytosis of sperm • autoimmune response to endometrium/ovarian tissue • Luteinised unruptured follicle syndrome (LUF) • Altered eutopic endometrium |
|
|
Non-active Endometerosis
|

|
|
|
Active endometerosis
|
can affect the quality of the egg
|
|
|
Azoospermia
|
1. Obstructive
• congenital = BCAVD • infection • vasectomy 2. Non - obstructive • genetic • maldescent • chemotherapy / radiotherapy • mumps |
|
|
Reduced sperm parameters
|
• Genetic
• Local genital causes • Medical disease • Medications • Noxious agents • ?Environmental |
|
|
Male obesity and fertility
|
• Sperm count reduced 50%
• 50% reduction in chance of conception • Increased sperm DNA fragmentation • Erectile dysfunction x 2 |
|
|
Male obesity - mechanism
|
• Reduced total and free testosterone
• Increased Estrone and E2 • Reduced FSH and LH • Reduced spermatogenesis and testosterone production • Increased testicular temperature |
|
|
Male age and fertility
|
• Independent effect (far less than the effect of female
age) • Lower potency / lower ejaculation frequency • Higher rates of infertility • Higher rates of aneuploidy – Down’s • Increase in relative risk for autism – spectrum disorders |
|
|
Known karyotype errors associated with male factor
infertility |
• 47 XXY – Klinefelter’s syndrome
• Klinefelter – related mosaicism • Balanced translocation between autosomes • XX male – transposition of SRY gene to an autosome |
|
|
Human Y chromosome
|
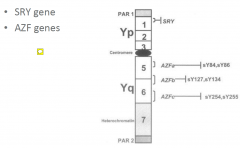
Y has no paterner to swap or recombine with...
thus the Y chromosome is gorwing shorter with bits flying off Areas of the Y chromosome that are cut off and they have low sperm counts and thus the kids will have the same problem (have to tell the couple this) |
|
|
Y chromosome microdeletions
|
• Can be detected in a proportion of men with sperm
concentrations below 2 million / ml • Can involve AZF A, B or C regions • Have been detected in male offspring from successful ICSI treatments |
|
|
Semen analysis
problems |
• Problems with collection / delivery
• Lab variability • Variation in reference standards |
|
|
Semen analysis - parameters
|
• Volume 1.5 ml
• Density 15 million / ml • Overall motility 40% • Progressive motility 32% • Normal morphology 4% |
|
|
Sperm chromatin structural assay (SCSA)
|
• Analyzes degree of DNA damage to sperm, often
secondary to reactive oxygen species in seminal fluid • Consider in cases of – Recurrent miscarriage – Otherwise unexplained infertility – Smokers / infrequent intercourse – Poor embryo development in IVF • Antioxidants / frequent ejaculations |
|
|
Important work up in male factor infertility
|
> Examination
> Hormone profile including FSH, LH, testosterone, prolactin, thyroid function > Scrotal ultrasound > Karyotype if concentration < 10 mill / ml > Y chromosome microdeletions if concentration < 2 mill / ml > Cystic fibrosis screening if obstructive azoospermia |
|
|
Antisperm Ab
|
- measure infemale serum
- measure in males too; can be higher after infection, post-vasectomy... (due to back pressure and breakdown of the blood testies barrier) - female; serum and cervix - Consider: postcoital test |
|
|
Klinefelter’s Syndrome
|
> 1 in 650 men
> Testes 1-4 ml in 99% of cases > Up to 75% never diagnosed |

