![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
421 Cards in this Set
- Front
- Back
|
Nutrient agar |
Basic media for non-fastidious bacteria |
|
|
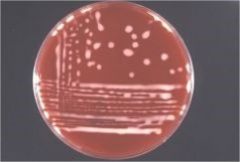
blood agar |
enriched media most pathogenic bacteria allows for recognition of hemolysis |
|
|
MacConkey agar |
selective medium gram (-) bacteria |
|
|
Eosin Methylene Blue (EMB) agar |
selective medium gram (-) bacteria |
|
|
Columbia Nalidixic Acid (CNA) |
selective medium gram (+) bacteria |
|
|
Chocolate agar |
for fastidious bacteria |
|
|
Brilliant green agar |
for salmonella |
|
|
Trypticose Soy Broth |
general purpose medium aerobic bacteria |
|
|
Buffered-peptone water |
non-selective medium to low number of pathogens in environment and feed |
|
|
Selenite broth |
selective enrichment medium Salmonella spp |
|
|
Hayflick liquid medium |
selective enrichment medium Mycopasma spp |
|
|
UVM medium |
selective medium Listeria spp |
|
|
Selective media |
-contains substances to either: +enhance growth of particular organisms +inhibit growth of unwanted organisms -dyes (eosin, methylene blue), pH, NaCl, antimicrobials, etc
|
|
|
GasPak system |
anaerobic bacteria -use reducing media containing compounds like sodium thioglycollate -plates placed in sealable containers utilizing chemicals to provide oxygen-free environment |
|
|
Streak-plate method |
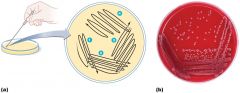
|
|
|
Pour-plate method |

|
|
|
Confirming presence of pathogenic bacteria (3 ways) |
-stained smears -cultural & biochemical characteristics -detection by immunological & molecular methods |
|
|
Gram stain |
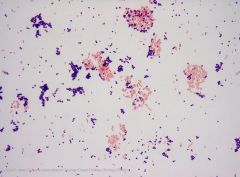
Widely used -crystal violet retained by gram (+) -crystal violet not retained by gram (-) |
|
|
Giemsa stain |
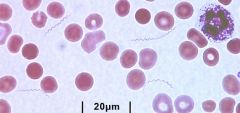
Dermatophilus congolensis Rickettsia Babesia Anaplasma Borrellia
|
|
|
Ziehl-Neelsen (acid-fast) stain |
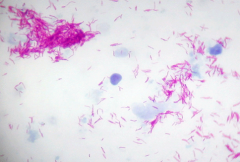
Mycobacterium spp Actinomycetes (red=positive)
|
|
|
Carbol fuchsin stain |
Campylobacter Brachyspira Fusobacterium (stain red) |
|
|
Basic criteria for presumptive ID |
-colonial morphology and color -presence/absence of hemolysis -appearance on gram staining/ability to grow on MacConkey -motility -reaction to biochemicals (catalase & oxidase test) |
|
|
Biochemical tests |
-sugar fermentation -triple sugar iron (TSI) -sulfide indole motility (SIM) -urease |
|
|
Particular tests |
-CAMP reaction -Coagulase -Hemagglutination -Nagler test |
|
|
ID'ing oxygen requirements |

|
|
|
Immunological techniques |
-fluorescent antibody tests (Leptospira, Clostridium) -ELISA tests (Clostridium difficile) -Agglutination tests (Salmonella typing, Taylorella) |
|
|
Phage typing |
-use of well-characterized lytic phages to ID specific bacteria -causes lysis of bacteria -special labs for Salmonella and Staphlyococcus |
|
|
Molecular techniques |
PCR tests -Mycrobacterium paratuberculosis -Mycoplasmsa bovis -Moraxella differentiation -Genotyping C. perfringens and C. difficile -Leptospira -Salmonella
DNA sequencing |
|
|
Bacteria & Archaea |
-prokaryotic -no nuclei -single chromosome (usually) -asexual reproduction -great majority don't cause disease -archaea often isolated from extreme environments |
|
|
Fungi |
-eukaryotic -have cell walls -molds and yeasts |
|
|
molds |
-multicellular -filamentous growth -sexual and asexual spores |
|
|
Yeast |
-unicellular -oval to round -reproduce by budding |
|
|
protozoa |
-single-celled eukaryotes -most capable of locomotion by pseudopodia, cilia, or flagella -most asexual |
|
|
algae |
-unicellular/multicellular photosynthetic organisms -make own food from CO2 and water using energy from sunlight |
|
|
Viruses |
-smaller than prokaryotes -not visible by light microscope -acellular -obligate intracellular |
|
|
prokaryotic cells |
-nucleoid not surrounded by nuclear membrane -usually single chromosome -no membrane-bound organelles -minute size -binary fission -no cytoskeleton -ie bacteria |
|
|
eukaryotic cells |
-nuclear material surrounded by nuclear membrane ->1 chromosome -membrane-bound organelles -fairly large -mitosis/meiosis -cytoskeleton -ie fungi, algae, plant, mammalian cells |
|
|
prokaryotic capsule/glycocalyx |
-gelatinous, sticky substance surrounding cell -composed of polysaccharides, polypeptides, or both +made inside cells and extruded onto cell's surface (K-antigen)
|
|
|
prokaryotic capsule/glycocalyx |
-protect bacteria from immune system cells and desiccation -virulence factor -numerous pathogenic bacteria (Bacillus antracis, Klebsiella pneumoiae) |
|
|
flagella |
-mostly gram (-) bacteria -bacterial movement -virulence factor |
|
|
flagella |
3 parts: -filament (flagellin protein) -hook -basal body (bacterium)
-differences in flagella proteins may allow classification of species into serovars |
|
|
fimbriae |
-for movement & adherence to each other & environment -up to 100's on the cell -shorter than flagella -important function in biofilms
|
|
|
Pili (conjugation pili) |
-transfer of DNA from one cell to another |
|
|
Bacterial cell walls |
-provide structure and shape -protect cell from osmotic forces -assist in attaching to other cells -resisting antimicrobial drugs -target for antibiotics -give bacteria characteristic shapes -mainly composed of peptidoglycan |
|
|
Gram staining procedure |
1. slide flooded with crystal violet, then rinsed in water. all cells purple 2. slide flooded in iodine, then rinsed in water. all cells purple 3. slide flooded in ethanol and acetone, then rinsed with water. Gram (+) remain purple, gram (-) colorless 4. slide flooded with safranin, then rinsed with water and blotted dry. Gram (-) pink. |
|
|
Bacterial cytoplasmic membranes |
-fluid mosaic model controls passage of substances into/out of phospholipid bilayer: +hydrophilic heads +hydrophobic hydrocarbon tails -membrane proteins for recognition, enzymes, receptors, carriers, and channels
|
|
|
Plasma membrane function |
-selectively permeable -naturally impermeable to most substances -proteins allow substances to cross membrane -maintain concentration & electrical gradient -site of electron transport for respiration |
|
|
Passage of substances from membrane |
-passive (smaller molecules) +diffusion +facilitated diffusion +osmosis -active processes +active transport +group translocation |
|
|
cytoplasm |
-water (mostly) + dissolved/suspended substances (ions, carbohydrates, proteins, enzymes, lipids, DNA, RNA, wastes) -chemical reactions occur -houses storage granules (lipids, starch, etc) |
|
|
ribosomes |
-sites of protein synthesis -prokaryotic ribosomes different than eukaryotic +50S + 30S -some antimicrobial drugs target protein synthesis |
|
|
nuclear material |
-single haploid circular chromosome -extensively folded with small amounts of protein & RNA -some 2 circular chromosomes, 1 linear chromosome, plasmid |
|
|
protein secretion systems |
-mechanisms to transport large molecules through complex membranes and cell walls -gram (-) bacteria (esp) have evolved secretion pathways |
|
|
effector proteins |
-proteins transported through secretion systems -includes enzymes (proteases, lipases, cytotoxic/apoptosic proteins) |
|
|
endospores |
-produced for durability and pathogenicity -high content of dipicolinic acid and calcium -resistant to drying, pasteurization, radiation -ie Bacillus anthracis, Clostridium tetani, Clostridium perfringens |
|
|
biofilms |
-bacterial populations adherent to each other &/or surfaces -enclosed in a biopolymer matrix -immobile form -complex relationships among numerous microorganisms
|
|
|
biofilms |
-develop extracellular matrix -allows attachment to substrate -drug penetration difficult -microorganisms more harmful as part of a biofilm |
|
|
formation of endospore |
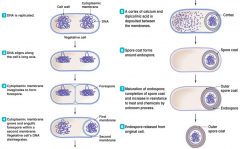
|
|
|
endospore germination |
-initiated when conditions are favorable -heat, warm weather, nutrients |
|
|
microbial growth |
increase in a population of microbes that results in either: -discrete colony-aggregation of cells arising from a single parent cell -biofilm-collection of microbes in the surface of a complex community |
|
|
typical microbial growth curve |
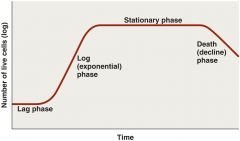
|
|
|
binary fission |

|
|
|
generation time |
time required for bacterial cell to grow and divide -dependent on chemical and physical conditions |
|
|
obligate aerobes |
oxygen is essential |
|
|
obligate anaerobes |
oxygen is deadly -toxic forms of O2 are highly reactive and excellent oxidizing agents -resulting oxidation causes irreparable damage to cells |
|
|
ID oxygen requirements |

|
|
|
nitrogen requirements |
-anabolism often ceases due to insufficient nitrogen -acquired from organic & inorganic nutrients -cells recycle nitrogen from amino acids and nucleotides -nitrogen fixation by certain bacteria essential to life on earth |
|
|
chemical requirements |
-phosphorus-membrane/cell wall, DNA, RNA, ATP -sulfur-disulfide bonds of proteins -trace elements required in small amounts (se) -growth factors-some amino acids, purines, pyrimidines, NADH, heme |
|
|
effect of temperature on growth |
-too low, membranes become rigid and fragile -too high, membranes become too fluid
pathogenic bacteria usually can't grow outside specific temperature range |
|
|
psychrophiles |
-5C to 20C |
|
|
mesophiles |
most of the pathogenic bacteria
15C to 45C |
|
|
thermophiles |
42C to 80C |
|
|
hyperthermophiles |
polymerases for PCR reactions
67C to 105C |
|
|
pH requirement |
organisms sensitive to changes in acidity -H+ and OH- interfere with H-bonding
|
|
|
Neutrophiles |
grow best in narrow range around neutral (7) pH
most pathogens grow best around neutral pH |
|
|
Acidophiles |
grow best in acidic (<7) pH -yeast (Candida) and Clostridium difficile |
|
|
physical effects of water |
-osmotic pressure -hydrostatic pressure
-microbes require water to dissolve enzymes, nutrients -most cells die in absence of water -some have cell walls the retain water (Mycobacterium spp) -Endospores & cysts-most metabolic activities stop |
|
|
culturing microorganisms |
-cultivating microorganisms -inoculum introduced into medium |
|
|
obtaining pure cultures |
-cells arising from a single progenitor -aseptic technique prevents contamination of sterile substances/objects -streak plates -pour plates |
|
|
colony forming unit |
-progenitor of cells |
|
|
characteristics of bacterial colonies |
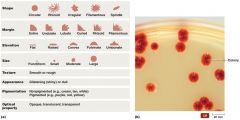
|
|
|
culture media |
some microorganisms don't require specific nutrients (E. coli), but some do (Haemophilus somni) -liquid & solid media
|
|
|
agar |
complex polysaccharide -most microbes can't digest agar -powdered agar dissolves at 100C -solidifices at 40C |
|
|
solid media |
-blood agar -MacConkey -Hekton -CNA -urease slant -citrate slant |
|
|
defined media |
know concentration of each ingredient in media |
|
|
complex media |
contains variety of nutrients released by partial digestion of yeast, soy, beef, or casein -exact chemical composition unknown -blood often added to provide NADH and heme |
|
|
selective media |
contains substance either to encourage growth of particular organisms or inhibit growth of unwanted organisms -some dyes (eosin, methylene blue), pH, NaCl, antimicrobials used |
|
|
differential media |
used to differentiate microorganisms -visible changes in medium or differences in appearance of colonies -many media selective & differential |
|
|
transport media |
used for carrying clinical specimens -feces, saliva, sputum, blood -Amie's transport medium + charcoal |
|
|
special culture techniques |
-low-O2 culture-microaerophiles -enrichment culture-enhancing growth of less abundant microbes in specimen -cold enrichment-cold tolerant microbes (Listeria, Vibrio cholerae) -animal-no growth in liquid media (M. laprae-armadillos; Treponema pallidum-rabbit) -cell culture-viruses, rickettsias |
|
|
direct method (measuring microbial reproduction) |
-serial dilution & viable plate counts -membrane filtration -most probable number -microscopic counts -electronic counters |
|
|
serial dilution & viable plate count |

|
|
|
membrane filtration |
-used when population density is low
pic |
|
|
cell counter |
-no incubation required
pic |
|
|
indirect methods (measuring population size) |
-metabolic activity -turbidity -dry weight -genetic methods |
|
|
metabolic activity |
measure nutrient utilization, waste production, pH |
|
|
turbitidy |
MacFarland for antimicrobial susceptibility, spectrophotometer
|
|
|
dry weight |
filtered, dried, weighed |
|
|
genetic methods |
isolate total DNA of microorganism -perform real-time PCR -UV spectrophotometry of DNA -used to estimate number of microbes |
|
|
refrigeration preserving cultures |
stores for short periods of time |
|
|
deep-freezing preserving cultures |
stores for years |
|
|
lyophilization preserving cultures |
stores for decades |
|
|
role of HEPA filters |
prevents human contamination from specimen
pic |
|
|
tissue & organ specimens |
-suitable portions placed in individual polyethylene bags/suitable leakproof container -portions of intestine (tied off) should be packaged separately |
|
|
swab specimens |
-abscesses -nasal passages -pharynx -tonsil -eye -ear -skin -vagina/cervix
prevent drying by using suitable transport medium |
|
|
fecal specimen |
-preferably obtained directly from rectum in manner that avoids contamination -avoid submission of fresh droppings -place in leak-proof container and ship immediately |
|
|
milk specimen |
collected aseptically using sterile screw-capped/stoppered vials (not bags) -should be refrigerated immediately following collection -deliver to lab under refrigerated conditions |
|
|
urine specimen |
collected aseptically -refrigerated immediately -avoid free-catch samples -minimum 5mL urine |
|
|
antrax, plaque, tularemia, foreign diseases special considerations |
clearly label all boxes & bags to avoid exposure to lab personnel |
|
|
antrax special considerations |
cotton swabs soaked in extruded blood/blood taking from superficial ear vein -swine-swabs taken from exudates & cut surfaces of hemorrhagic lymph nodes |
|
|
blackleg, malignant edema special considerations |
submission of fresh affected tissues -clostridium rapidly invades tissues after death -2 impression smears on glass slides |
|
|
clostridial enterotoxemia special considerations |
several ounces of fresh intestinal contents or tied-off section of affected intestine |
|
|
Johne's disease special considerations |
fecal specimen from live animals |
|
|
Campylobacteriosis special considerations |
-semen, preputial washing, fetal stomach contents, cervical mucus obtained aseptically -refrigerated & delivered to lab within 5-6 hours of collections -OR frozen as soon as collected with dry ice and shipped in insulated container with adequate amount of dry ice |
|
|
Brucellosis special considerations |
placenta, stomach content of aborted fetus, mammary lymph nodes, milk samples preferred -shipped under refrigerated conditions |
|
|
Listeriosis special considerations |
submit brain stem sample and indicate Listeria is suspected |
|
|
fungal isolations |
take up to 3 week before reported out -collect samples aseptically before antifungal therapy |
|
|
fungal specimens |
-superficial mycoses-hair & skin scrapings from edge of active lesions +submit in small paper envelope +saprophytic fungi will proliferate rapidly and overgrow ringworm fungi in sealed container -deep-seated mycoses-tissues & organs as for bacteriology |
|
|
drug |
chemical that affects physiology in any manner |
|
|
antimicrobial agent |
-drug that treat infections -kill or inhibit growth of susceptible microorganisms |
|
|
Paul Erlich |
-"magic bullets" -arsenic compounds that killed Treponema pallidum (causative agent of syphillus)
|
|
|
Gerhard Domgak |
-Prontosil red for Streptococi infections -Converted to sulfanilamide in body by liver |
|
|
Alexander Fleming |
-Penicillin released from Penicillium sp. |
|
|
Selman Wkasma |
-Antimicrobial agents produced naturally by organisms -Other antibiotics-streptomycin |
|
|
Selective toxicity |
more toxic to pathogen than host -based on differences of biochemical, structural, or metabolic pathways between bacteria and eukaryotes |
|
|
Bactericidal |
drugs that kill bacteria |
|
|
bacteriostatic |
drugs that inhibit bacterial pathogenity |
|
|
Ratio of drugs available |
Antibacterial>antifungal>antiviral |
|
|
Inhibition of cell wall synthesis |
-prevent cross-linkage of NAM subunits in peptidoglycan layer -prevent bacteria from increasing amount of peptidoglycan |
|
|
Beta-lactams |
-functional groups are beta-lactam rings -bind to enzymes that cross-link NAM subunits
-Penicillins Cephalosporins |
|
|
Beta-lactams: affect existing peptidoglycan layer? |
-NO! -bacteria have weakened cell walls and eventually lyse due to increased osmotic pressure inside cell |
|
|
Vancomycin & cycloserine mechanism |
-interfere with particular bridges that link NAM subunits -many gram (+) |
|
|
Bacitracin mechanism |
-blocks secretion of NAG and NAM from cytoplasm |
|
|
Isoniazid and ethambutol mechanism |
-disrupt mycolic acid formation in mycobacterial species |
|
|
Semi-synthetic beta-lactam derivative benefits |
-more stable in acidic environments (stomach) -more readily absorbed -less susceptible to deactivation -more active against more types of bacteria |
|
|
monobactams vs synthetics/semisynthetics (amoxicillin, ampicillin) |
monobactams-effective ONLY against aerobic gram (-)
synthetics-more effective on gram (+) |
|
|
Inhibition of protein synthesis |
-prokaryotic ribosomes 70S (30S & 50S) -eukaryotic ribosomes 80S (40S & 60S) +mitochondria contain 70S-drugs can be more toxic with more adverse effects -drugs selectively target translation |
|
|
different mechanisms of inhibiting protein synthesis |

|
|
|
Aminoglycosides |
-used topically-not absorbed well orally -little activity against anaerobes
-amikacin, kanamycin, neomycin, tobramycin, spectionomycin |
|
|
tetracyclines |
-block docking site of mRNA
-large spectrum -shouldn't be used in pregnant animals
-textracycline, doxycycline, minocycline |
|
|
chloramphenicols |
-binds and blocks binding site of amino acids
-chloramphenicol, florfenicol |
|
|
macrolides |
-bind to 50S subunit, blocking proper mRNA movement through ribosome, stopping synthesis
-enytromycin, axithromycin, claritromysin, tylosin -mainly affect gram (+) cocci and intracellular pathogens |
|
|
disruption of cytoplasmic membrane |
-form channel through cytoplasmic membrane and damage integrity |
|
|
polymyxin |
-disrupts cytoplasmic membranes of gram (-) -toxic to kidneys |
|
|
amphotericin b |
-attaches to ergosterol in fungal membranes -bacteria lack sterols, so not susceptible |
|
|
inhibition of nucleic acid synthesis |
-block DNA replication or mRNA transcription
-often affect eukaryotic & prokaryotic cells
-limited clinical use-except quinolones and fluoroquinalones |
|
|
quinolones and fluroquinolones |
-act against prokaryotic DNA gyrase and topoisomerase IV |
|
|
rifampin |
-inhibit RNA polymerase during transcription |
|
|
reverse transcriptase inhibitors |
-acts against enzyme of retroviruses -don't harm mammalians because they lack reverse transcriptase |
|
|
inhibition of metabolic pathways |
-effective when metabolic processes of pathogen & host differ |
|
|
sulfonamides |
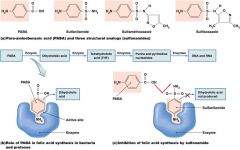
-structural analogs
|
|
|
heavy metals |
-inactivate enzymes |
|
|
clinical considerations |
-ideal antimicrobial agent -spectrum of action -efficacy -routes of administration -safety & side effects |
|
|
ideal antimicrobial agent |
-readily available -inexpensive -chemically stable -easily administered -nontoxic & nonallergenic -selectively toxic against wide range of pathogens |
|
|
spectrum of action |
-number of different pathogens a drug acts against
-narrow-spectrum effective against few organisms
-best to perform antimicrobial susceptibility test before starting treatment |
|
|
broad-spectrum |
-effective against many organisms -may allow for secondary or superinfections to develop -killing of normal flora reduces microbial antagonism |
|
|
efficacy |
ascertained by -diffusion susceptibility test -minimum inhibitory concentration (MIC) test -minimum bactericidal concentration test |
|
|
minimum inhibitory concentration teset |
-lowest concentration of antimicrobial that prevents visible growth of microorganisms in a broth dilution susceptibility test |
|
|
Susceptible |
an infection due to the isolate may be treated in body sites with the recommended dosage |
|
|
resistant |
isolates are not inhibited by the usual achievable concentration of a drug and not reliable in treatment |
|
|
intermediate |
infection due to isolate may be treated in body sites where high dosage of the drug can be used |
|
|
no interpretation |
no interpretative criteria established yet |
|
|
routes of administration |
-topical-external infections -oral-no needles -IM-via needle into muscle -IV-via needle into bloodstream
must know how antimicrobial agent will be distributed to infected tissues |
|
|
toxicity |
-cause of many adverse reactions poorly understood
-may be toxic to kidneys, liver, or nerves
-pregnant animals need extra consideration |
|
|
allergies |
-rare, but may be life-threatening -anaphylactic shock |
|
|
disruption of normal microbiota |
-may result in secondary infections -overgrowth of normal flora causes superinfections -greatest concern in hospitalized animals |
|
|
resistance to drugs |
-some pathogens naturally resistant
acquired in 2 ways: -new mutations of chromosomal genes -acquisition of R-plasmids via transformation, transduction, and conjugation |
|
|
mechanisms of resistance |
-produce enzyme that destroys or deactivate drug -slow or prevent entry of drug into cell -alter target of drug so it bind less effectively -alter their metabolic chemistry -pump drug out of cell before it can act -biofilms retard drug diffusion and slow metabolic rate -Mycobacterium tuberculosis produces MfpA protein, binds DNA gyrase depriving fluoroquinolones |
|
|
multiple resistance |
-pathogen can acquire resistance to more than 1 drug -common when R-plasmids are exchanged -develop in animal hospitals +constant use of drugs eliminates sensitive cells -superbugs |
|
|
cross resistance |
resistance to structurally similar drugs at the same time |
|
|
limiting antibacterial resistance |
-effective surveillance systems for collection of data at local & national level -treatment based on susceptibility test results -strict adherence to drug withdrawal periods in food-producing animals -maintain high concentration of drug in patient for sufficient time -use only when necessary -use in combination |
|
|
synergism |
two agents enhancing the individual effects of drugs |
|
|
Trueperella (Arcanobacterium) pyogenes pathogenicity |
opportunistic causing suppurative lesions -hemolytic toxin pyolysin causes pus formation -neurominidases, extracellular matrix proteins, and fibria -proteases |
|
|
Trueperella (Arcanobacterium) pyogenes species |
cattle, pigs, sheep |
|
|
Trueperella (Arcanobacterium) pyogenes affected area |
any organ system -bovine pneumonia -hepatitis -osteomyelitis -peritonitis -cerebral abscesses -lymphadenitis -mastitis |
|
|
Trueperella (Arcanobacterium) pyogenes appearance on culture |
-small hemolytic colonies in BAP -typical pleomorphic cell morphology in gram stain |
|
|
Trueperella (Arcanobacterium) pyogenes treatment |
-based on antimicrobial susceptibility test -resistance to macrolides and tetracyclines
-feedlot cattle receive sub-therapeutic doses of tylosin (macrolide) as prophylaxis against liver abscessation
-no vaccine |
|
|
Actinomyces bovis disease |
bovine actinomycosis-lumpy jaw -assumed to invade following trauma
|
|
|
Actinomyces bovis affected area |
-mandible -maxilla less common causes chronic osteomyletis
-min involvement with regional lymph nodes -swelling painful -fistulous tracts |
|
|
Actinomyces bovis diagnosis |
-advanced cases-distinctive clinical signs -radiography -bacterial culture |
|
|
Actinomyces bovis culture appearance |
-filamentous branching -non acid-fast (purple) |
|
|
Actinomyces bovis treatment |
-small lesions: surgery -adv cases: surgery unrewarding
prolonged therapy with penicillins
sodium iodine-IV multiple times |
|
|
Actinomyces viscosis disease |
canine actinomycosis -A. canis and A. hordeovulnaris also isolated in similar conditions |
|
|
Actinomyces viscosis affected area |
extensive fibrovascular proliferation on the peritoneal and pleural surfaces -with sanguinopurulent exudate
|
|

|
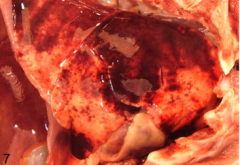
Actinomyces viscosis gross apperance |
|
|
Actinomyces viscosis diagnosis |
bacterial culture |
|
|
Actinomyces viscosis treatment |
penicillins |
|
|
Nocardia sp characteristics |
-gram (+) -aerobic -inhabitant of soils rich in organic matter -opportunistic infections
|
|
|
Nocardia sp smear characteristics |
-smears: long, slender, branching filaments +partial acid-fast +gram staining (+)
|
|
|
Nocardia sp pathogenesis |
-assc with immunosuppression or heavy challenge -usual mode of infection: inhalation +may occur by skin wounds and teat canal -supreoxide disnutase, catalase, and thick peptidoglycan confer resistance
|
|
|
Nocardia sp culture characteristics |
-culture: produce aerial filaments +may have spores +white, powdery, odorless, firmly adherent to agar
-grow in Sabouraud agar
|
|
|
Nocardia sp sequencing |
-16S rRNA DNA sequencing |
|
|
Nocardia asteroides common name |
Canine nocardiosiis |
|
|
Nocardia asteroides affected systems |
-pulmonary -cutaneous -CNS |
|
|
Nocardia asteroides pulmonary |
-develop from inhalation -not typically seen -mostly in dry, warm climates |
|
|
Nocardia asteroides cutaneous |
-result from intro of bacteria into wounds -may produce mycetoma |
|
|
Nocardia asteroides CNS |
-result from spread of bacteria in blood -meningitis in humans-inhfalation to blood |
|
|
Nocardia asteroides tx + control |
-tx less effective than for canine actinomycosis +intrinsically resistant -susceptibility using broth microdilution -amikacin, imipenem-cilastatin, TMX usually effective -prevention-avoiding exposure to bacteria in soil |
|
|
Bovine nocaridal mastitis characteristics |
-chronic bovine mastitis -usually sporadic cases -diffuse or multifocal fibrosis -white clots intermittently in milk -systemic reactions may be induced during early lactation |
|
|
Bovine nocaridal mastitis tx |
-difficult to treat -dry-cow therapy with neomycin could be effective |
|
|
Bovine nocardiosis common name + distribution |
bovine farcy -limited to tropical areas -Mycobacterium spp also isolated |
|
|
Bovine nocardiosis systems affected |
chronic infection of superficial lymphatic vessels and lymph nodes +thickened and cord-like -nodules on the medial aspects of legs and on neck |
|
|
Actinobaculum suis common name/disease |
porcine cystitis and pyelonephritis |
|
|
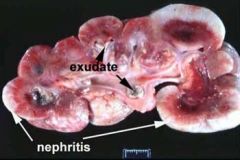
Actinobaculum suis pathogenecity |
-causes cystitis and pyelonephritis in breeding pigs (mostly female) -ascending infection
|
|
|
Actinobaculum suis predisposing conditions |
-mating -trauma to urogenital tract -presence of other organisms -water restriction |
|
|
Actinobaculum suis presentation |
-sudden death with or without clinical signs -hematuria, azotemia -mild fever -painful urination -arching of back |
|
|
Actinobaculum suis diagnosis |
-gram stain (+) -culture -PCR -immunofluoresence |
|
|
Actinobaculum suis tx |
penicillin ampicillin |
|
|
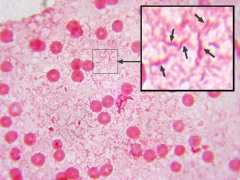
Dermatophilus congolensis smear characteristics |
-gram (+) -filamentous -branching -produces motile coccal zoospores |
|
|
Dermatophilus congolensis predisposing factors + pathogenesis |
-maybe present in skin of healthy animals -trauma and persistent wet conditions -when activated, zoospores produce germ tubes and invade epidermis
-cyclical pattern or invasion/regeneration of epidermis, serous exudation and microabscess formation lead to raised scab-like crusts |
|
|
Dermatophilus congolensis virulance factors |
-phospholipases -proteolytic enzymes -ceramidase |
|
|
Dermatophilus congolensis dx |
-clinical picture -scab material & skin in formalin -smears from undersurface of scabs for Giemsa -cultured on BAP +small, yellowish, hemolytic colonies -no growth in Sabouraud agar -16S DNA sequencing |
|
|
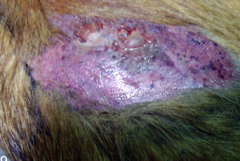
Dermatophilus congolensis clinical picture |
-dorsal areas of animals +prolonged rainfall +warm environment -early lesions appear as papules -serous exudate and inflammation produces adherent scabs |
|
|
Dermatophilus congolensis tx |
-localized lesions can resolve spontaneously -systemic long-acting oxytetracycline or penicillin/streptomycine -topical tx ineffective |
|
|
Nocardioform placentitis causative agents |
Crossiella equi Amycolatopsis spp |
|
|
Nocardioform placentitis pathogenesis |
gram (+) filamentous branching bacteria -causes brown mucoid placentitis -sporadic |
|
|
Nocardioform placentitis clinical signs |
-premature udder development/lactation -vulvar discharge
<1/2 mares exhibit signs |
|
|
Nocardioform placentitis dx |
-ultrasound exam |
|
|
Nocardioform placentitis outcomes |
-abortion -premature foal -term, but compromised foal -normal foal
mare clears infection rapidly, rebreeds normally, not at increased risk of subsequent abortion |
|

|
Trueperella (Arcanobacterium) pyogenes |
|

|
Actinomyces bovis |
|

|
Nocardia asteroides canine nocardiosis |
|

|
Dermatophilus congolensis |
|

|
Nocardioform placentitis Crossiella equi Amycolatopsis spp |
|
|
Diseases associated with Staphylococcal sp
|
infections of dogs and cats, S. intermedius(S. pseudointermedius)
staphylococcal mastitis, S. aureus exudative epidermitis–S. hyicus Omphalitis– S. aureus Botryomycosis– S. aureus Tick Pyemia– S. aureus Methicillin resistant Staphylococcal infections |
|
|
Causative agent of Staphylococcal infections in dogs and cats
|
S. intermedius(S. pseudointermedius)
|
|
|
Staphylococal infections of cats and dogs are
|
opportunistic pathogens
|
|
|
staphylococcal diseases of cats and dogs cause
|
suppurative conditions: dermatitis, pyoderma, otitis externa, endometritis, cystitis, osteomyelitis and wound infections
|
|
|
symptoms of staphylococcal diseases of cats and dogs
|
fever, pain, loss of appetite, itching, pus filled lesions such as pyoderma
|
|
|
who is more susceptible to staphylococcal diseases of cats and dogs and why
|
younger and older dogs due to weak immune system
|
|
|
staphylococcal diseases of cats and dogs; cystitis cases signs and symptoms
|
often urination, urinalysis may indicate increased protein and hemoglobin
|
|
|
staphylococcal diseases of cats and dogs; diagnosis
|
clinical signs
gram staining of clinical specimen culture and/or biopsy |
|
|
When obtaining specimen for bacteriological culters one must
|
–avoid superficial contamination
–special swab protected by a sterile otoscope for otic specimens –skin shaved and disinfected for blood specimens –urine collected by cystocentesis, catherter or midstream(clean catch) –swabs should be kept in transport media, kept cold and submitted to lab ASAP |
|
|
staphylococcal diseases of cats and dogs: Tx
|
–stop itching and scratching for skin diseases
–topical therapy may be ineffective in uncomplicated superficial infections(combinations of silver sulfadiazine, mupiracin, fusidic act etc) –susceptible to antimicrobials including beta lactams though some multi resistance strains(MRS) detected –for urinary infections drugs excreted by urine should be chosen for up to 2 weeks |
|
|
Staphylococcal mastitis
|
common form of mastitis worldwide caused by S. aureus
–can be subclinical, chronic, and acute –necrosis due to alpha toxins |
|
|
transmission of Staphylococcal mastitis
|
contaminated hands and milking equipment
|
|
|
what could cause systemic reaction and be lethal in staphylococcal mastitis
|
peracute and gangrenous forms
|
|
|
symptom of gangrenous form of staphylococcal mastits
|
effected quarter is cold, dark and eventually sloughs
|
|
|
Staphylococcal mastitis Tx
|
–Cephalosporins, cloxacillin, erythromycin, penicillin
–if susceptible penicillin can be combined with novobiocin, pirliycin, tylosine or tilmicosin |
|
|
Staphylococcal mastitis Tx concerns
|
–Antimicrobials administered by parenteral or intrammamary routes
–difficult to treat with success rate up to 60% –intrammamary route advised: parenteral could be used during acute mastitis –culture and susceptibility should be done |
|
|
Desirable characteristic of antimicrobials to treat mastitis
|
–low MIC for pathogen
–high distribution and availability in mammary tissue –low serum protein binding activity –long half life |
|
|
control plan for mastitis
|
–properly maintain of milking equipment
–hygienic milking practices –post–milking teat disinfection –antibiotic therapy for clinical cases and for dry cows –culling of persistently infected cows |
|
|
Exudative epidermitis
|
caused by S. hyicus in suckling and weaned pigs
|
|
|
characteristics of exudative epidermitis
|
widespread sebaceous secretion and exudation on skin surface and highly contagious
|
|
|
symptoms of exudative epidermitis
|
anorexic, depressed, febrile and non prutic dermatitis with greasy exudate
|
|
|
Mobidity/mortality of exudative epidermitis
|
20–100%/can reach 90% in litters
|
|
|
S. hyicus can be isolated from
|
healthy pigs' vaginal mucosa and skin
|
|
|
Exudatie epidermitis transmission
|
via minor abrasions on the skin
|
|
|
exudative epidermitis predisposing factors/major virulence factor
|
weaning/ exfoliative toxin
|
|
|
exudative epidermitis diagnosis
|
clinical: high mortality rate in oung pigs with exudative, non prutic skin lesions
laboratory: isolation and identification of S. hycus by culture |
|
|
Tx of exudative epidermitis
|
early systemic antibiotic combined with topical antiseptics and/or antibiotics
|
|
|
control of exudative epidermitis
|
–strict isolation of infected pigs
–cleaning and disinfecting of contaminated buildings –sows should be washed prior to farrowing with antiseptic soap |
|
|
S. aureus infections in poultry
|
omphalitis– infection of yolk sac can be seen in young chicks
–skin injuries may cause localized abscesses like on the foot(bubblefoot) –may also cause invasive infections in bones, joints, tendon sheaths, and sternal bursa |
|
|
omphalitis causes
|
decreased weight gain and egg production and mortality
|
|
|
S. aureus infections in poultry diagnosis
|
E. coli and Pasteurela multocida may cause similar lesions in poultry so identification by culture
|
|
|
S. aureus infections in poultry Tx
|
AST must be performed due to common drug resistance
|
|
|
S. aureus infections in poultry prevention
|
–proper management to reduce injury and immunosuppression
–elimination of wood splinters, protruding wires of cages and fighting –good litter management and hatchery management |
|
|
Botryomycosis
|
–a chronic, suppurative condition often caused by S. aureus
–can occur within a few week of castration of horses due to infection of spermatic cord(schirrhous cord) –can also happen in mammary tissues of sows, composed of fibrous tissue and pus |
|
|
Tick pyemia
|
characterized by either septicemia and rapid death or by localized abscesses in many organs
|
|
|
predisposing factor for tick pyemia
|
Anaplasma phagocytophilum transmitted by ticks
|
|
|
confirmatory test for tick pyemia
|
microscopic identification of S. aureus in pus and isolation
|
|
|
tick pyemia Tx
|
–limited value
–prophylactic Tx of lambs can be initiated at age week 1 |
|
|
most MRS strains are
|
coagulase positive
|
|
|
MRS Tx
|
– limited options
–antimicrobial susceptibility must be performed –vancomycin often the only drug of choice as well as oxazolidiones like Linezolid but never be used as a single agent to Tx MRSA infections |
|
|
Diseases/important species of Streptococcus spp
|
–Strangles–S equi subsp equi
–Purpura hemorrhagca –S. zooepidemicus and S.equisimilis –S. canis –Bovine streptococcal mastitis –S. suis –enterococcus spp |
|
|
Strangles
|
–a febrile disease, with abscessation of lymph nodes, commonly in young horses that's highly contagious disease of horses
reportable disease |
|
|
transmission of strangles
|
via purulent exudates or discharging absesses
–sales, shows, race–tracks increase the risk |
|
|
Strangles:Clinical signs
|
–incubation period 3–6 days
–high fever, depression, and anorexia followed by oculonasal discharge which becomes purulent –lymph nodes are swollen and painful characteristically submandibular lymph nodes are effected and eventually rupture discharging purulent highly infectious material –guttural pouch empyema common –most horses become immune with reinfection occurring in some horses |
|
|
Strangles Morbidity/mortality
|
–up to 100%/less than 5%
–death due to complications |
|
|
Strangles– diagnosis
|
–clinical signs and history of recent exposure to suspect animal
–must be differentiated from S. zooepidemicus and S. equisimilis for causing similar problems –culture and PCR(tests are very sensitive to detect) –colonies are beta hemolytic slightly mucoid sugar fermentation tests help to differentiate |
|
|
Strangles Tx
|
–Penicillin to in contact animals
–antimicrobial therapy is controversial for infected horses and limited if abscesses have formed –carriers may be treated with local antibiotic treatment of guttural pouch –ruptured abscesses should be flushed with 3–5%povidine–iodine solutions –anti–inflammatory drugs for pain and fever |
|
|
Strangles– Control
|
–isolation of suspected and infected horses |
|

|
Purpura hemorrhagica |
|

|
Strangles
|
|
|
Purpura hemorrhagica
|
immune mediated disease that may occur due to strangles |
|
|
Tx of purpura hemorrhagica
|
–dampening the immune response and removing the inciting cause |
|

|
Ascending placentitis associated with S. zooepidemicus and S. equisimilis being number 1 reason in horses
|
|
|
S. zooepidemicus and S. equisimilis
|
–mucosal commensals, opportunistic pathogens |
|
|
strangles like syndromes in horses reported in
|
S. zooepidemicus and S. equisimilis cases
|
|
|
Differentiation of S. zooepidemicus and S. equisimilis
|
–beta hemolytic colonies
– sugar fermentation tests and PCR –must be differentiated from S. equi |
|
|
Tx of S. zooepidemicus and S. equisimilis
|
–in early phase susceptible to beta lactams
–in early detection of placentitis tx could be effective –no vaccines available |
|
|
S. canis
|
|
|
S. canis
|
|
|
S. canis
|
–opportunistic pathogen causing neonatal septicemia, suppurative conditions(otitis externa, pneumonia, pleuritis, dermatitis, myositis, nephritis) and toxic shock syndrome in carnivores |
|
|
S. canis infections diagnosis
|
–gram staining of exudate may reveal streptococci in chain |
|
|
Tx of S. canis
|
–usually susceptible to beta–lactams but Tx may not always be successful
–draining and flushing the abscesses hasten recovery –dose could be higher than normally recommended because organisms could be harbored in the tonsillar crypts and pus –cats with diskospondylitis may require up to 6 months of antimicrobial, usually starting with a parenteral injection then subsequent oral meds |
|
|
Bovine streptococcal mastitis
|
three kinds
S. agalactiae S. dysgalatiae S. uberis |
|
|
S. agalactiae
|
bovine streptococcal mastitis which colonizes milk ducts and produces intermittent acute infections
|
|
|
S. dysgalatiae
|
bovine streptococcal mastitis which is found in the buccal cavity, genitalia and skin and causes acute mastitis
|
|
|
S. uberis
|
bovine streptococcal mastitis which is a normal inhabitant of skin tonsils and vaginal mucosa, a major causative agent of mastitis usually without systemic signs.
|
|
|
Bovine streptococcal mastitis diagnosis
|
–clinical sins–inflammation of mammary tissue and clots in milk
–milk samples should be sent to lab for culture |
|
|
differentiation of mastitis causing streptococci
|
by CAMP test and sugar fermentation tests
PCR also available |
|
|
Tx of bovine streptococcal mastitis
|
susceptible antimicrobials following culture–tx success is high especially for S. agalactiae
for environmental streptococci dry season therapy |
|
|
bovine streptococcal mastitis control
|
–milking hygiene
– biosecurity to limit reintroduction –avoid cross–suckling in calves –avoid any nutritional deficency –minimize teat sealants prepartum –cows that are refractory to tx should be culled |
|
|
S. suis is recognized as
|
significant losses to pig industry
|
|
|
S. suis Lancefiled group D
|
–at least 35 serotypes with varying virulence
–serotype 2 is the most prevalent serotype |
|
|
S. suis is associated with
|
–meningitis, arthritis, septicemia and bronchopneumonia of all ages
–sporadically can cause endocarditis, neonatal deaths and abortions –respiratory cases are in conjunction with Mycoplasma spp and Pasteurella spp |
|
|
S. suis pathogenesis
|
–capsule and an opacity factor are both essential pathogenic factors
–strains positive for suilysin, extracellular factor(EF), and muramidase released protein(MRP) are mose virulent –adhesions such as fibronectin–binding protein are other factors –hyaluronidase may facilitate local spread |
|
|
S. suis Tx
|
–most strains susceptible to beta–lactams
–prophylactic long–acting penicillins can be given by injection to sows 1 week before farrowing and piglets during first 2 weeks of life |
|
|
S. suis control
|
–bacteria tend to be endemic in a herd and eradication is not feasible
–improved husbandry needed –vaccine are available but may not be effected mostly due to serotype differences |
|
|
Enterococcus species
|
can cause opportunistic infections such as UTI and otitis in dogs, mastitis in cattle with E. faecalis most frequently isolated
|
|
|
Enterococcus species identification
|
–forms short chains and pairs and lacks a capsule
–previously classified with group D streptococci and reclassified as a separate genus |
|
|
enterococcus species are found in
|
the human colon though rarely pathogenic at this site and can cause disease if introduced into other parts of body
|
|
|
Tx of enterococcus species
|
intrinsically resistant to many antimicrobials so difficult to treat making it a possible major health concern in humans
|
|
|
Enterococcus spp differ from streptocci by |
–not sensitive to bile salts so will grow on MacConkey Agar |
|
|
prevention of enterococcus spp |
–difficult in health care setting |
|

|
Enterococcus
|
|
|
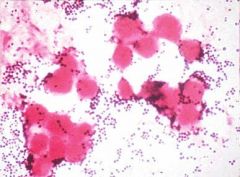
gram stain of purulent exudate of staphylococcal infections of dogs and cats |
|

|
bubblefoot from omphalitis |
|

|
omphalitis |
|

|
Staphylococcal infections in dogs and cats |
|

|
Staphylococcal infections in dogs and cats |
|

|
Staphylococcal mastitis |
|
|
Corynebacterium spp morphology
|
–small, pleomorphic, gram +
–in stained smears appear Chinese letter characters –relatively slow growth in lab media |
|
|
Differentiating factors of corynebacterium spp
|
–most are catalase +, oxidase –,
–non spore forming –pathogenic bacteria are non motile –cause pyogenic infections |
|

|
chinese letter characters of corynebacterium spp
|
|
|
corynebacteriu spp pathogenesis and pathogenicity |
–opportunistic pathogens |
|
|
C. presudotuberculosis can surviv and replicate in |
phagocytes
|
|
|
virulence in C. presudotuberculosis is linked to
|
–cell wall lipid and an exotoxin(phospholipase D(PLD)) and Corynebacteial secreted protease 40(CP40)
|
|
|
what may enhance survival and multiplication of corynebacterium spp
|
PLD
|
|
|
CP40 induces |
strong immune response which may provide protection
|
|
|
What do C. pseudotuberculosis and C. ulcerans produce |
diphtheria–toxin which the presence of in milk may have public implications
|
|
|
C.renale group are
|
–urinary tract pathogens and produce urease
–also posses fimbriae for attachment to urogenital mucosa |
|
|
Diagnositc procedures of Corynebacterium spp
|
–animals species affected and clinical signs may suggest a specific infection
–suitable specimens for the lab: pus, exudate, affected tissue, midstream urine –direct examination of gram stained smears may reveal corynebacteria –culture media: blood agar, McConkey and CNA incubated up to 5 days at 37C |
|
|
Corynebacterium spp identifying diagnostic procedures |
–colonial characteristics
– presence of hemolysis –absence of growth in McConkey, presences of growth in BAP and CNA –typical corynebacterium polymorphism on gram stain –biochemical tests |
|
|
Caseous lymphadenitis is |
a chronic suppurative condition of sheep, goat, and rarely cattle caused by C. pseudotuberculosis with organisms surviving in the environment for several months
|
|
|
Caseous lymphadenitis transmission route
|
–skin wounds, arthropod bites, or dips |
|
|
caseous lymphadenitis clinical signs
|
–abscessation and enlargement of superficial and internal lymph nodes
–goats usually develop superficial, subcutaneous abscesses usually in the head and neck –ill–thrift and pneumonia may be present –visceral form may not be detected antemortem |
|

|
caseous lymphadenitis |
|
|
incubation period of caseous lymphadenitis |
around 3 months
|
|
|
Caseous lymphadenitis diagnosis
|
–clinical (or postmortem) findings |
|
|
Caseous lymphadenitis: Tx |
susceptible to many antimicrobials but therapy is usually ineffective due to intracellular survival ability of bacteria and inability of drugs to penetrate into abscesses |
|
|
caseous lymphadenitis: control |
–import animals from countries/states/flocks free of caseous lymphadenitis |
|
|
ulcerative lymphangitis is/caused by |
– slow and chronic either lymphangitis of lower limbs or abscessation of pectoral region(also called pigeon fever) |
|
|
ulcerative lymphangitis is transmited by |
skin wounds, arthropod bites or contact of infected animals
|
|

|
ulcerative lymphangitis |
|

|
ulcerative lymphangitis
|
|
|
ulcerative lymphangitis clinical signs
|
–lymphatic vessels swollen and firm with nodules forming along their length |
|
|
ulcerative lymphangitis diagnosis |
based on isolation and identification in the lab
|
|
|
Tx and control of ulcerative lymphangitis |
–systemic antimicrobials may be combined with topical Tx |
|
|
Bovine pyelonephritis causative agent |
C. renale– which may be isolated from healthy cattle vulva, vagina and prepuce |
|
|
Bovine pyelonephritis acquired by
|
stress of parturition and short urethra in cow may predispose to infection |
|
|
Bovine pyelonephritis |
|
|
Bovine pyelonephritis: clinical signs
|
–fever, anorexia and decreased milk production |
|
|
Bovine pyelonephritis: Tx
|
–antimicrobial tx based on susceptibility test, should start early for at least 3 weeks |
|
|
Ulcerative balanoposthitis
|
–caused by C. renale |
|
|
C. renale may cause mucosal irritation and ulceration by
|
hydrolyizing urea into ammonia |
|
|
predisposing factor of Ulverative balanoposthitis
|
high urea level in the urine due to high protein intake
|
|

|
ulcerative balanoposthitis |
|
|
rhodococcus equi morphology
|
–gram positive rods or cocci |
|
|
Rhodococcus equi |
|
|
Rhodococcus equi– suppurative bronchopneumonia epidemiology
|
–one of the most common causes of pneumonia in folas |
|
|
Rhodococcus equi– suppurative bronchopneumonia pathogenesis
|
–ability to survive and multiply in macrophage |
|
|
Rhodococcus equi– suppurative bronchopneumonia clinical signs
|
–usually less than 4 weeks old foals |
|

|
Rhodococcus equi– suppurative bronchopneumonia |
|
|
Rhodococcus equi– suppurative bronchopneumonia: diagnosis
|
–differentiating lower respiratory trac infections problematic |
|
|
Rhodococcus equi– suppurative bronchopneumonia: Tx |
–combination of oral rifampin and a macrolide for up to 10 weeks |
|
|
Rhodococcus equi– suppurative bronchopneumonia: control |
–vaccines not available |
|
|
Symbiosis |
"live together" |
|
|
mutualism |
benefits mammal benefits bacteria |
|
|
commensalism |
benefits bacteria neither harms/benefits mammal |
|
|
parasitism |
benefits bacteria harms mammal |
|
|
resident microbiata |
"normal flora" "indigenous microbiota" not normally causing disease -resident -transiet |
|
|
resident microbiota |
-part of the normal microbiota throughout life -mostly commensal |
|
|
transient microbiota |
-remain in body for short period -found in same regions as resident -cannot persist in body -competition from other microorganisms -elimination by body's defense cells |
|
|
acquisition of normal microbiota |
-development in womb free of microorganisms -microbiota begin to develop during birthing process -much resident microbiota established during first months of life -communities tend to be host-specific or organ-specific -normal microflora primes the immune system |
|
|
Opportunistic pathogens |
-normal microbiota that cause disease under certain circumstances -introduction into unusual site -immune suppression -changes in relative abundance may allow opportunity for member to thrive and cause disease |
|
|
reservoirs of infectious disease |
-most pathogens cannot survive for long period outside of their host -sites where pathogens are maintained as a source of infection -3 types +infected animals +carriers +nonliving reservoir |
|
|
infected animal |
transmit disease by excretions -aerosol -direct -feed -venereal |
|
|
carriers |
-infected individual who are asymptomatic but infective to others -some eventually develop illness, others never get sick -healthy carriers may have defensive systems that protect them |
|
|
nonliving reservoirs |
-soil -food -water contaminated often by feces or urine |
|
|
zoonoses |
-diseases naturally spread from animal host to humans |
|
|
acquisition of zoonoses |
-direct contact with animal/waste -eating animals -bloodsucking arthropods
humans usually dead-end host
|
|
|
contamination |
the mere presence of microbes in/on the body |
|
|
infection |
when organism evades body's external defenses, multiplies, and becomes established in the body |
|
|
portals of entry |
-sites where pathogens enter body -skin -ear -mucous membranes -placenta -parenteral route |
|
|
portals of exit |
-where we obtain specimens -ear -blood -skin -urine -feces -semen/vaginal excretions -eye tears -nose secretions -saliva -milk
|
|
|
pathogen |
infectious biological agent causing disease to its host -must find appropriate niche -must compete with normal microflora -must evade/overcome host defese |
|
|
pathogenisis |
-express proteins, adhesins, and other virulence factors to cause disease |
|
|
virulence genes |
many encoded within mobile genetic elements -plasmid -bacteria phage -composon
some encoded in bacterial chromosome |
|
|
antibiotic resistance genes |
carried in plasmids -makes other bacteria resistant to AB |
|
|
adhesion in infection |
-process by which microorganisms attach themselves to other cells -required to successfully establish colonies in host
|
|
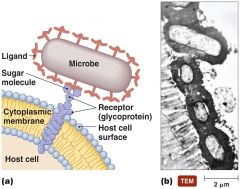
|
adhesion of pathogens to host cells |
|
|
adhesion factors |
-specialized structures -attachment proteins |
|
|
role of adhesion |
-attachment proteins help in adhesion -changing/blocking ligand or its receptor can prevent infection -inability to make attachment proteins/adhesins renders microorganisms avirulent -some bacterial pathogens attach to each other to form a biofilm |
|
|
attachment proteins |
-found on viruses and many bacteria -viral/bacterial ligands bind host cell receptors |
|
|
virulence factors |
-adhesion factors -biofilms -extracellular enzymes -toxins -antiphagocytic factors |
|
|
pathogenicity |
ability of microorganism to cause disease |
|
|
virulence |
degree of pathogenicity |
|
|
virulence factors extracellular enzymes |
-secreted by pathogen -dissolve structural chemicals in body -help pathogen maintain infection, invade, and avoid body defenses |
|
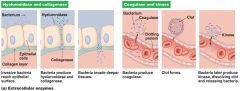
|
extracellular enzymes |
|
|
toxins |
|
|
virulence factors toxins |
chemicals that harm tissues or trigger host immune responses that cause damage -endotoxins -exotoxins |
|
|
toxemia |
toxins in bloodstream that are carried beyond site of infection |
|
|
virulence factors antiphagocytic factors |
prevent phagocytosis by the host's phagocytic cells -bacterial capsule +composed of chemicals not recognized as foreign +slippery-difficult to engulf -antiphagocytic chemicals +prevent fusion of lysosome and phagocytic vesicles +leukocidins directly destroy phagocytic WBCs |
|
|
infection |
the invasion of the host by a pathogen |
|
|
disease |
results if the invading pathogen alters normal bodily functions -aka morbidity |
|
|
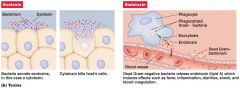
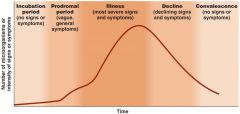
stages of infectious disease |
|
|
symptom |
subjective characteristics of disease felt only by patient |
|
|
sign |
objective manifestations of disease observed/measured by others |
|
|
syndrome |
symptoms & signs that characterize disease/abnormal condition |
|
|
asymptomatic/subclinical |
lack symptoms, but may still have signs of infection |
|
|
acute diseases |
relatively sudden onset of symptoms that are usually severe |
|
|
chronic disease |
disease that persists for a long time. A chronic disease is one lasting 3 months or more |
|
|
subacute |
poorly defined state between acute and chronic |
|
|
latent disease |
remaining in an inactive or hidden phase |
|
|
communicable disease |
illness caused by an infectious agent or its toxins that occurs through the direct or indirect transmission of the infectious agent or its products from an infected individual or via an animal, vector or the inanimate environment to a susceptible animal or human host |
|
|
contageous disease |
An infectious disease that is spread through contact with infected individuals |
|
|
principal challenge of host response |
detection of pathogen & mounting a rapid defensive response |
|
|
innate immunity |
-external physical barriers -internal protective cells |
|
|
external physical barriers |
-skin -mucous membranes |
|
|
internal protective cells |
-macrophages -neutrophils -anti-microbial peptides -interferons, complement inactivating pathogens |
|
|
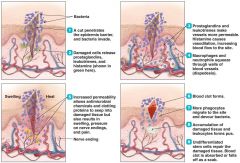
inflammation |
|
|
adaptive immunity |
acquired immunity against unique species of pathogens by highly specialized immune cells |
|
|
5 attributes of adaptive immunity |
-specificity -inducibility -clonality -unresponsivesness to self -memory |
|
|
4 functions of antiboides |
-neutralization -opsonization -oxidation -agglutination |
|
|
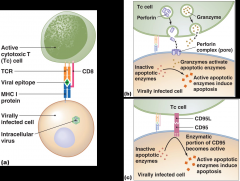
cellular immune response |
|
|
etiology |
-study of the cause of disease |
|
|
germ theory of disease |
disease caused by infections of pathogenic microorganisms |
|
|
Koch's postulates |
-suspected agent must be present in every case of the disease -agent must be isolated and grown in pure culture -cultured agent must cause disease when it is inoculated in a healthy, susceptible experimental host -same agent must be reisolated from the diseased experimental host |
|
|
exceptions to Koch's postulates |
-some pathogens can't be cultured in lab -disease caused by combo of pathogens & other cofactors -ethical considerations prevent applying Koch's postulates to pathogens that require a human host |
|
|
difficulties in satisfying Koch's postulates |
-disease can be caused by more than 1 pathogen -pathogens that are ignored as potential causes of disease |

