![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Neurocysticercosis- dif dx
|
-Equinococcosis/ hydatidosis
-Toxoplasmosis -Brain abscess -CVA -Brain neoplasm -Seizure disorder -Meningitis -CNS TB -Cerebral amebiasis -CNS cryptococcosis -Mycotic granulomas -Neurosyphillis |
|
|
Neurocysticercosis- hx
|
-Often asymptomatic
-Cognitive decline -Headache -Dizziness -Seizures -Hx of eating undercooked pork, infected family members -Found in Mexico, SW US |
|
|
Neurocysticercosis- physical
|
-Depends on location of cysts
-Dysarthia -EOM palsy or paresis -Hemiparesis or hemiplegia -Hemisensory loss -Movement disorders -Hyper/hyporeflexia -Gait disturbances -Meningeal signs -Intracranial HTN: diplopia, hydrocephalus |
|
|
Neurocysticercosis- dx tests
|
-CSF: mononuclear pleocytosis, normal glucose, elevated protein, high IgG, eosinophilia
-CSF ELISA for NCC -Stool exam: taeniasis -CT: variable findings based on stage of infestation -MRI: best |
|
|
Neurocysticercosis- tx
|
-Symptomatic tx w/ phenytoin, mannitol
-Anticysticercal meds: praziquantel, albendazole -W. hydrocephalus d/t intraventricular cyst, place ventricular shunt followed by surgical removal of cyst -Tx concomitant intestinal infect: niclosamide |
|
|
Neurocysticercosis- prognosis
|
-Good prognosis in most patients
-Most frequent complication is chronic epilepsy |
|
|
Neurocysticercosis- pathophys
|
-Caused by fecal-oral cointact injestion of pork tapeworm Taenia solium ova (typically in stool of pts w/ taeniasis) hatch into tissue-invading larval forms migrate to brain & encyst inflammatory rxn
-Fecal-oral route |
|

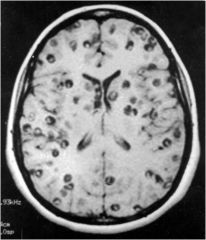
What is this disease?
|
Neurocysticercosis
|
|
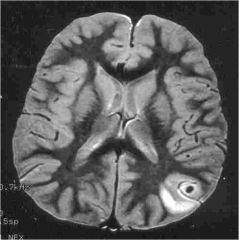
What is this infection?
|
Neurocysticercosis
|
|
What infection is this?
|
Neurocysticercosis
|
|
|
Encephalitis-dif
|
-Meningitis
-Brain abscess |
|
|
Encephalitis- hx
|
-Develops in adults and children w/o prodromal illness
-Fever -Headaches, N/V -Mental status changes: confusion, delirium, confusion, stupor, coma -Seizures: generalized or focal -Mild stiff neck -Possible hx of genital lesions (HSV Type 2) -Hx & clinical signs nonspecific |
|
|
Encephalitis- physical
|
-Hypeerreflexia, Babinski signs, or spasticity
-Less common: tremors, dystonia, papilledema |
|
|
Encephalitis- dx tests
|
-CBC: WBC elevated
-CSF: increased pressure; mononucl. pleocytosis; elevated RBCs; mild-mod elevated protein; nl glucose; neg gram stain -Definitive dx via detection of HSV DNA in CSF by PCR test -EEG: abnormal -MRI: early changes include T2-weighted abnormalities in medial temporal lobe w/ extension into subfrontal and insular cortex -CT: later changes – low-density lesions in one/ both temporal lobes & areas of hemorrhagic necrosis |
|
|
Encephalitis- treatment
|
-HSV: acyclovir IV for 14 days
-RNA viruses (arbo, measles, rabies): symptomatic |
|
|
Encephalitis- prog
|
-HSV: w/o tx w/ acyclovir, 70% mortality; w/ acyclovir – 30% mortality and 30% of survivors make a good recovery
-Arboviruses: 50% mortality for eastern equine encephalitis and Japanese B virus and 10-15% mortality from WNV - |
|
|
Encephalitis- pathophysiology
|
-Summary: Diffuse infection of brain parenchyma
-Viruses are most common infectious agents but bacteria (T. pallidum), and protozoa (toxoplasmosis) also cause diffuse brain infections -HSV is most common: type 1 is acquired; type 2 is assoc w/ genital lesions -Arboviruses (mosquito or tick transmitted) can occur -Pathology: widespread brain inflammation w/ perivascular cuffing (lymphocytes adjacent to blood vessels) and focal necrosis w/ secondary gliosis; virus-infected cells w/ intranuclear inclusionbody |
|
|
Meningitis - bacterial-dif dx
|
-Brain abscess
-Encephalitis -Vasculitis -SAH |
|
|
Meningitis - bacterial-hx
|
-Rapidly progressive
-Highest incidence in elderly, infants, and immunosuppressed -Fever -Headache: caused by inflammation, irritating pain fibers along the base of the brain -Stiff neck -Confusion -Less common: stupor/ coma, seizures |
|
|
Meningitis - bacterial- physical
|
-Seldom presents with focal signs
-Hemiparesis, aphasia, ataxia, and visual loss may develop later in clinical course -Less common: papilledema -Positive Kernig sign: w/ pt supine, flex hip & extend leg at the knee pain in back of leg |
|
|
Meningitis - bacterial-dx tests
|
-Definitive dx via CSF examination/ emergency LP – cloudy, elevated opening pressure, protein > 100, decreased glucose, high WBCs, few RBCs, pleocytosis w/ polymorphonuclear predom
-CBC: WBC > 20,000; elevated neurophils, left shift (immature cells) -Elevated ESR & CRP -CT: no abnormalities but important to r/o increased ICP -MRI w/ gadolinium: enhancement of meninges, esp in basal cistern area -EEG: normal -Labs: CBC, blood culture |
|
|
Meningitis - bacterial- tx
|
-Prompt administration of IV broad-spectrum antibiotics that cross BBB, often 3rd gen cephalosporin or vanco until sensitivies obtained
-Administer for 10-14 days -Early admin of corticosteroids for 2-4 days reduces death and long term neuro sequelae -Symptomatic tx w/ phenytoin for sz |
|
|
Meningitis - bacterial-prog
|
-Mortality ranges from 5-25%
-In surviving children, 15% have language disorders, 10% mental retardation, 10% hearing loss, 5% weakness or spasticity, 3% epilepsy -Can lead to focal cerebritis abscess formation |
|
|
Meningitis - bacterial- patho
|
-Caused by bacterial entry into URT asymptomatic infection bloodstream invasion crosses BBB replicate and release endotoxins (gram neg) or teichoic acid (gram pos) macrophages & microglia release cytokines (IL-1, TNF) recruits neutrophils inflammation of the meninges d/t most commonly gram positive and negative aerobic bacteria
-Children <5 yo w/o vaccine: Haemophilus influenza; w/ vaccine: E. coli, group B Strep, Listeria monocytogenes -Children <15 yo: H. influenza, Neisseria meningitides, Streph pneumoniae -Chronic meningitis can be caused by Borrelia burgdorferi, Mycobacterium tubercolosis, and T. pallidum -Most common cause in young adults is Streptococcus pneumonia: gram positive diplococcus |
|
|
Meningitis – viral-dif dx
|
-Bacterial or fungal meningitis
-ADEM -Aseptic meningitis -HIV CNS infections -Hydrocephalus -Lyme disease -Brain neoplasm -Migraine variant -Neurcysticercosis -Subdural empyema |
|
|
Meningitis – viral-hx
|
-Severe headache
-Constitutional sx: N/V/D, cough, myalgias, fatigue, fever -Irritability -Stiff neck -Mild photophobia -Possible seizure |
|
|
Meningitis – viral-phys
|
-Fever
-Nuchal rigidity -Kernig sign -Look for signs of specific viral infections: pharyngitis, skin manifestations (zoster eruption), maculopapular rash, vesicular eruption, lymphadenopathy and splenomegaly (EBV), parotitis & orchitis (mumps), gastroenteritis & rash (enteroviruses) |
|
|
Meningitis – viral-dx
|
-CT before LP to r/o intracranial hematoma, mass effect, or hydrocephalus
-CSF: clear, protein 10-100, glucose normal, <10 WBCs, 10-1,000 RBCs for HSV, otherwise few RBCs; do viral PCR CMV, acid-fast stain, VDRL -Labs: Chem 7, CBC w/ diff -Blood, fecal, and throat viral serology & cultures -Serum titers of HIV, toxoplasma, RPR, lyme antibody |
|
|
Meningitis – viral- tx
|
-1st rule out bacterial infection or start empiric antibiotics
-Supportive care w/ rest, hydration, antipyretics, and NSAIDs -Pts w/ signs & sx of meningoencephalitis should receive acyclovir early -Prevent viral septic shock in babies w/ broad-spectrum antibiotics and acyclovir -Seizures: IV lorazepam, phenytoin |
|
|
Meningitis – viral- prog
|
-Uncomplicated meningitis: clinical course is self-limited w/ complete recovery in 7-10 days
-Mortality <1% (excluding neonates) |
|
|
Meningitis – viral- patho
|
-Cause: hematogenous or neural (axonal retrograde transport of HSV, VZV) route into CNS inflammation of leptomeninges w/o spinal cord or parenchymal involvement
->85% caused by nonpolio enteroviruses |
|
|
Meningitis – Cryptococcus neoformans- dif dx
|
-CNS Toxoplasmosis
-CNS lymphoma -CNS abscess -CNS neoplasm -TB meningitis -HIV encephalopathy/ dementia -Meningococcal meningitis -Seizure |
|
|
Meningitis – Cryptococcus neoformans- hx
|
-Immunocompromised pts
-HIV CD4 < 200 -Insidious onset w/ waxing/waning course -Initial fever and malaise -Headache -N/V -Stiff neck -Visual disturbances -Seizure |
|
|
Meningitis – Cryptococcus neoformans- phy
|
-Depends on location of lesions
-Focal neurologic deficits -Papilledema -Altered mental status |
|
|
Meningitis – Cryptococcus neoformans-dx
|
-CSF: opening pressure >200; clear/ turbid appear; protein levels >45; glucose is normal; india ink stain positive; test for cryptococcal antigen – rapid, 90% sensitive; fungal culture is gold standard but takes days
-CT: screening study; may be nonspecific or nl -MRI: T1- low intensity lesions in basal ganglia; leptomeningeal enhancement |
|
|
Meningitis – Cryptococcus neoformans- tx
|
-High dose amphotericin B with flucytosine, fluconazole
-May need repeated LPs or ventriculoperitoneal shunt to manage intracranial HTN d/t basal meninges obstruction -No primary prophylaxis -Secondary prevention includes fluconazole -Treat seizures |
|
|
Meningitis – Cryptococcus neoformans- prog
|
-Fatal if untreated
-Acute mortality 6-14% -Relapse after treatment is 30-50%; 0-7% with fluconazole prophylaxis -6% mortality rate despite aggressive therapy |
|
|
Meningitis – Cryptococcus neoformans- patho
|
-Pathophys: Hematogenous spread from lungs (possible subclinical infection) to CNS
-May present as space occupying lesion, meningitis, or meningoencephalitis -Most common fungal illness in HIV pts -Abscesses are most common in cerebellum and basal ganglia |
|
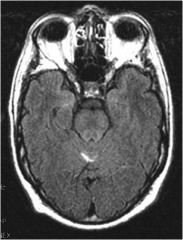
What disease?
|
Cryptococcus neoformans
|
|
|
Brain abscess- dif dx
|
-Meningitis
-Necrotic or cystic primary and metastatic brain neoplasm -Granuloma -Subdural empyema -Atypical cerebral infarction or hematoma |
|
|
Brain abscess- hx
|
-Headache, N/V
-Mental status changes: confusion, stupor, coma -Seizures: generalized or focal |
|
|
Brain abscess- physical
|
-CN 6 palsy
-Hemiparesis -Papilledema -Focal neurologic signs depending on location of abscess |
|
|
Brain abscess-dx tests
|
-Examine for primary site of infection
-Dx made by CT/MRI -Elevated WBCs -Elevated ESR, CRP -Increased ICP -Surgically remove pus from abscess: gram stain, Giemsa stain, fungal stain, culture, histologic examination |
|
|
Brain abscess- tx
|
-Prompt reduction in size of life-threatening masses
-Corticosteroids may be administered briefly to reduce surrounding edema -Definitive tx w/ antibiotics (3rd-4th gen cephalosporins plus metronidazole for 4-8 weeks) and neurosurgical drainage or evacuation -ID and elimination of source of abscess -Prevention of sz w/ phenytoin -Neurologic rehab |
|
|
Brain abscess- prog
|
-10-20% mortality
-20-60% of survivors have neurologic sequelae including hemiparesis, aphasia, ataxia, and visual loss -Chronic seizures are common, may be focal or generalized, and may be difficult to suppress w/ anticonvulsants |
|
|
Brain abscess- pathophys
|
-Summary: Localized mass infection within the brain parenchyma that develops over 1-2 weeks
-Most commonly occur from bacterial infection, but fungi, M. tuberculosis, and protozoa can cause focal brain infection -Microorganisms reach brain via bloodstream, directly from infected sinuses or mastoid air cells, depressed skull fractures, or surgical procedures |

