![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
121 Cards in this Set
- Front
- Back
|
where are antibodies made?
|
B cells -> plasma cells -> antibody (released into circulation)
|
|
|
Why are APC necessary?
|
helper T cells cannot recognize, free antigen. T cells can only bind antigen processed and presented on surface via an MHC molecule.
note: MHC II expressed on macrophage, B cell, etc. |
|
|
Where do memory cells originate from?
|

From B-cell clones (in humeral) AND T-cells (in cell-mediated)
During effector phase of humeral immune system, B-cell expressing MHC II antigen on surface bind to T helper cell. Cytokines released from helper T cell, stim. B cells to divide and create clones of B cells, become either memory cells or αB secreting plasma cells. note: these helper T cells were made during activation phase to recognize this antigen/MHC receptor. |
|
|
Chemotaxis
|
phenomenon in which cells, bacteria, etc. direct their mov't according to certain chemicals in environment.
|
|
|
What type of cell does macrophage activate in humoral immune system?
|
helper T cell (aka CD4)
|
|
|
Macrophage presents engulfed antigen on surface by attaching it to what type of protein?
|
MHC class II
|
|
|
4 Steps of Phagocytosis:
|
1a. Chemotaxis: attracts neutrophil via chemical gradient of chemokines (type of cytokine) or complement protein
1b. Neutrophils migrate from vessels (see intergrins) to tissues 2. Adhere to microbe via receptors (with compliment proteins or with Fc part of αB) 3. Ingestion 4. Destruction: O2 dependent (respiratory burst) or O2 independent (phagolysome) |
|
|
precursor to B and T cells
|
lymphoid stem cell
|
|
|
difference between macrophages and monocytes?
|
macs are moncytes that have migrated from blood vessels to tissue
|
|
|
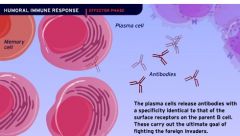
What happens during effector phase of humeral immune system?
|
Following Activation Phase:
B cells expressing antigen with MHC type II on surface become activated by cytokines from helper T cell (cloned during activ.phase), differentiate...into memory cells or antibody producing plasma cells |
|
|
First to respond to inflammation?
|
neutrophils
|
|
|
Domestic species with most neutrophils per unit volume?
|
cats
|
|
|
myeloid stem cell develops into?
|
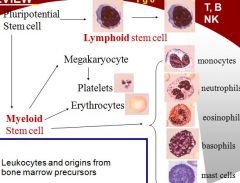
common myeloid progenitor cell is precursor to 3 groups:
1. myeloblast (eosinophil, neutrophil, and basophil) 2. megakaryoblast (platelets) 3. proerythroblast (RBC) ~lymphocytes do NOT originate from myeloid stem cells |
|
|
(edit)
Cells expressing MHC type II on surface? Cells expressing MHC type I on surface? |

APC, macrophages, B cells
Infected epithelial cells (in cell mediated immunity) express MCH type I,,,,recognized by activated cytoxic T cells, and NK killer cells |
|
|
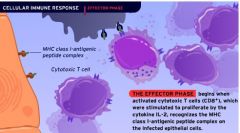
What happens in cell mediated immunity?
|
(activation phase)
APC express MHC II on surface (and infected epithelial cells express MHC I), helper T binds, releases cytokines IL-2 and INT-y to induce proliferation of cytot. T cells (CD8) and NK killers (effector phase). CD8 recognize MHC I on infected epith.cells, perforins released induce lysis. Memory T cells remain for future response. |
|
|
What is "activated" during activation phase?
What next? |
Helper T cells are activated
What next? In humoral immunity they clone themselves; while in cell mediated immunity they release IL2 and interferon gamma to proliferate CD8. |
|
|
How are cytoxic T cells inactivated?
|
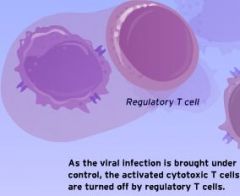
regulatory T cells
|
|
|
lifespan of neutrophils
when do they become active |
6-10 hrs. to a few days
immediately after release from bone marrow |
|
|
leukocyte adhesion molecules?
(allow neutrophils to adhere to endothelial wall and enter tissue) |
integrins
|
|
|
chemokines
|
family of chemostatic cytokines that serve as attractants for spec. cell populations..thus help mediate an inflammatory response
|
|
|
opsonins
|
proteins that promotes binding of pathogens to phagocytes
e.g. some antibodies and complement protein act as opsonins |
|
|
NK cells
Part of what immune system? Recognize what? Target what? Inhibited by what? |
do not recognize antigen but recognize infected cells by other mechanisms (different from CTL's)
part of innate immune system have Fc receptor, recognize Fc of Ab, inhibited by MHC-I molecules. If target cells does not express MHC-I, then NK cell try to kill it. |
|
|
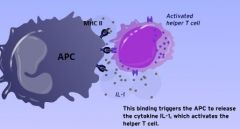
IL-1 is released by ?
Purpose of IL-1? |
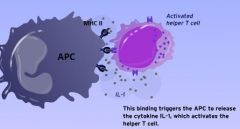
During activation phase of humoral immunity, *APC* releases IL-1 after it binds to helper T-cell,
Purpose is to activate helper T-cell to release IL-2! |
|
|
Another name for CD8+ ?
|
cytotoxic T cell
|
|
|
Another name for CD4+ ?
|
helper T cell
|
|
|
IL-2 is released by ?
Purpose of IL-2? |
During activation phase of humoral immunity, HELPER T-CELL releases IL-2 which stimulates itself to *clone*.
Thus producing many <helper T-cell>, each with receptor containing same original antigen. Also during activation phase of cell mediated immunity, HELPER T-CELL releases IL-2 (along with IFN-Y) which stimulates cytotoxic T cell to proliferate |
|
|
antibody is made by ?
|
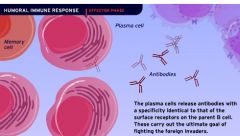
"plasma cells"
(B cell differentiate into plasma cells and memory cells.) Plasma cells then release αB with specificity identical to surface receptors on parent B cell |
|
|
Examples of possible APC's?
|
macrophages, dendritic cells, B-lymphocytes
NOT neutrophils! |
|
|
Where does humoral immune response get its name?
|
* B/c it is directed against extracellular invaders (while CMIS is directed against intracellular infection).
* Also antibodies are made to promote destruction of invaders, and these αB reside in body fluids (or "humors"). |
|
|
What kind of cells have Fc receptors?
|
NK cells, macrophages, neutrophils <- cells of innate immune system have receptor for Fc part of ANTIBODY
(antibodies bind @ fc receptor, tagging the antigen so these phagocytic can do their job) |
|
|
What are some major cytokines produced by macrophages?
|
IL-1 IL-6 IL-12 TNF-alpha
|
|
|
What are the molecules of the immune system that an antigen can interact with?
|
Antibody TCR on T-lymphocytes BCR on B-lymphocytes MHC molecules
|
|
|
Where are dendritic cells not found?
|
Brain Parts of eye Parts of testes
|
|
|
What are some types of dendritic cells?
|
Langerhans cells
Interdigitating dendritic cells Thymic dendritic cells |
|
|
What are some diseases linked to specific MHC molecules?
|
Bovine lymphoma
Bovine Leukemia virus - resistance? Marek's Autoimmune diseases - resistant poultry developed MHC molecules present in animal (which antigens able to present to immune system) determine how susceptible are too these diseases. All autoimmune diseases relate to type of MHC molecules present. Present self antigen. |
|
|
What is the small portion of the immunogenic molecule that actually binds to antibody, TCR, BCR, etc...?
|
Epitopes
|
|
|
What are some sites of foreign material removal performed by macrophages?
|
Blood sinusoids of liver and spleen Lungs
|
|
|
What are small molecules that bind to antibody but do not induce an immune response?
|
Hapten
|
|
|
What are cytokines that interfere with viral replication?
|
Interferons
|
|
|
Which APC is the only APC that can present and activate naive T-cells?
|
Dendritic cells
|
|
|
Where are dendritic cells prominent?
|
Lymph nodes skin mucosal surfaces
|
|
|
Which MHC molecule is only expressed on Antigen-Presenting cells (APCs)?
|
MHC-II
|
|
|
What is a B-cell that differentiates into an antibody secreting cell?
|
Plasma cell
|
|
|
What are the microbial molecules that are common among microbes?
|
Pathogen-Associated Membrane patterns (PAMP)
|
|
|
Is it possible for endogenous antigen to be processed as exogenous antigen?
|
Yes, if phagocytic cell engulfs infected cell
|
|
|
How do macrophages and neutrophils recognize microbes?
|
Pattern recognition receptors (PRR)
|
|
|
What are proteins that act as growth and differentiation factors for cells of the immune system?
|
Interleukins
|
|
|
If a protein epitope's recognition is dependent on the correct folding of the protein then it is called...?
|
Conformational epitope
|
|
|
What is the main mechanism of killing in NK cells?
|
Apoptosis
|
|
|
What part of the cell do the viral contents enter when infecting a cell?
|
cytosol
|
|
|
What is the most important group of pattern recognition receptors?
|
Toll-like receptors (TLR)
(expand on this) |
|
|
How many peptides can a given MHC molecule present at a time?
|
One
|
|
|
What type of presenting complex are endogenous antigens usually expressed on?
|
MHC-I
|
|
|
What kind of surface receptors do neutrophils have?
|
complement proteins and Fc part of Ab.
|
|
|
Can identical or similar epitopes be found on apparently unrelated molecules? Give example of this:
What can this cause? |
Yes e.g. some intestinal bacteria possess gp’s with A or B side chains on cell walls identical to those found on mammalian red blood cell gp.
In what is known as *cross-reactivity*, these gp's can be absorbed through intestinal wall into bloodstream and trigger antibody response. |
|
|
What are two things that allow TLR to recognize PAMP on an object in the body?
|
Phagocytosis
Production of cytokines |
|
|
Antigenicity vs immunogenicity
|
Antigenicity = ability of antigen to BIND w/immune components including (aB; B-cell via the BCR; T-cells via the TCR, or MHC molecule.
Immunogenicity = ability of antigen to INDUCE immune response Not all antigens are immunogens, but are all immunogens antigens? |
|
|
Properties of good immunogen?
|
1. Molecular Size: Needs to be >1kDa
2. Complexity/Chemical composition: e.g. glycoproteins, prokaryotic N.A. (esp.CpG motifs). 3. stability 4. foreigness (foreign proteins best) |
|
|
What of these are more complex and/or better immunogens:
Eukaryotic nucleic acids? prokaryotic N.A? Bacterial LPS? Carb.polymer? Plastics? Lipids? Glycoproteins? Proteins? |
1. prokaryotic N.A
2. Bacterial LPS 3. Glycoproteins, proteins |
|
|
Will identical twins accept eachother's tissue grafts?
|
Yes, foreignness in key characteristic of good immunogen, and in this case tissue would NOT be foreign.
|
|
|
A single immunogenic molecule may have several different _____; each will be recognized by different antibody and TCRs.
|
epitopes
note: antigen can also have multiple repeated epitopes |
|
|
What might cause protein epitopes to lose their immunogenicity?
|
if conformation protein epitope is denatured or structures are changed by degradation
|
|
|
What level protein organization might u find beta-pleated sheet and α-helix?
What level organization might u find Monomeric polypeptide molecule? |
Secondary structure
Tertiary structure |
|
|
quarternary structure?
|
Polymeric e.g. hemaglobin
|
|
|
How can type O pig which has never been exposed to type AB blood have severe reaction to AB blood transfusion?
|
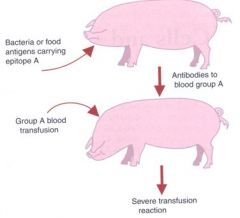
cross reactivity!
Pig developed antibodies against food antigen or bacteria with very similar epitope, Similar enough that αB recognize blood antigens. |
|
|
What might cause a cow to be incorrectly thought to have prior exposure to B. abortus: important pathogenic bacteria in cattle?
|
Strains of Yersinia enterocolitica (benign bacterium) share very similar epitope. Y. enterocolitica may provoke cattle to make αB that cross-react with B. abortus. Thus, a Yersinia-infected cow may be wrongly thought to have been exposed to B. abortus.
|
|
|
Where does precursor lymphoid stem cell develop?
Where do T cells develop? To what point in their maturity? |
bone marrow
T cells mature in thymus for (primary lymph.organ). Most importantly, by time T cells leave thymus they are already committed to becoming either cytotoxic T cells OR helper T cells! Once ready to leave, mature but still naive, having never seen antigen. |
|
|
Approximately how many days do T cells remain in thymus to mature?
|
~4 to 5 days
|
|
|
What happens if thymus of newborn is removed? What happens to composition of circulating lymphocytes? What sort of immune deficiencies might this animal have?
|
* W/o it, would see a major drop in circulating T-lymphocytes. (B cells aren't normally as prevalent).
* Would be unable to reject foreign tissue grafts, b/c involves cell-mediated immune.resp. and T-cells. * drop in αB response to Ag, as they are dependent on T-cells as well |
|
|
What percentage of developing lymphocytes are destined for destruction? *Why?*
|
90%, if they recognize self antigen presented to them by dendritic cell, they get signal to die.
Why? Because lymphocytes like B & T cells are suppose to recognize foreign antigen, not self! |
|
|
Role of CD3
|
* While in thymus, all T-cells (both CD4 and CD8) start expressing CD3
* molecular marker and signal transducer for any T-cell * tells cell when antigen has interacted w/TCR |
|
|
What must occur for B & T cells to become 'effector cells'?
|
must encounter antigen
e.g. B cell become plasma cells which make aB |
|
|
Major difference between B cells and T cells in terms of how react with antigen?
|
T-lymphocytes require that antigen is presented to them attached to MHC molecule (MHC-I or MHC-II).
B-cells can recognize linear epitopes on unprocessed antigen free in solution! Also TCR is never secreted, just expressed on surface, while BCR is secreted in form of aB |
|
|
structure of antibodies?
|
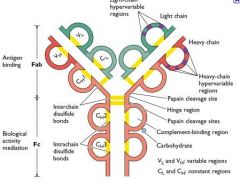
identical to BCR from parent plasma B cell from which it is secreted, but enclosed in membrane,
2 light chains 2 heavy chains variable region (attaches to antigen) Fc region (attaches to cell e.g. neutrophil) |
|
|
How do lymphocytes (BCR and TCR) generate so much diversity in terms of what antigens they recognize?
|
* Somatic gene rearrangement or recombination that occurs during maturation in primary lymph organs (bone marrow and thymus)
|
|
|
What happens if binding affinity between TCR or BCR and antigen is too weak?
|
If bond is too weak, won't get strong enough signal to activate lymphocyte into effector cell.
|
|
|
CD25
|
* receptor molecule able to bind IL-2.
* therefore any cell expressing CD25 can respond to IL-2. |
|
|
Main function of IL-2
|
important cytokine which usually tells cells to proliferate
|
|
|
hapten and carrier
|
a small molecule (<6kd) that is not immunogenic unless it binds to a carrier protein, permitting anti-hapten immune response
|
|
|
What is unique about respiratory burst (RB), a type of destruction within a phagocyte?
|
It is oxygen dependent
|
|
|
What are some examples of Intracellular pathogens that are able to survive inside macrophage?
How do they survive? |
Mycobacterium sp.
Rhodococcus equi Listeria monocytogenes Brucella abortus Salmonella *resistant to lysosomeal contents or inhibit phagolysosomal fusion |
|
|
PMN
|
polymorphonuclear leukocytes or Granulocytes
|
|
|
BLAD
|
integrin deficiency in cow
neutrophil can;t get out of blood stream |
|
|
basophil
|
granulocyte that promotes inflammation and allergies
mast cells also involved in inflammation |
|
|
Vaccination is example of
|
artificial passive immunity
|
|
|
How are macrophages downregulated?
|
steroids and prostaglandins
|
|
|
What phagocytic cell does NOT have sustained phagocytosis?
|
neutrophil
(but other macrophages like Kupffer and monocytes, etc. use sustained phagocytosis) |
|
|
Interleukins and monokines (pro-inflammatory proteins) are examples of ?
|
cytokines
|
|
|
interleukins are
|
growth and differentiation factors (cytokines) for cells of immune system
|
|
|
Major cytokines of macrophages?
Which is adjuvant for vaccine? |
IL-1
IL-6 IL-12 (adj. for vaccine) TNF-a |
|
|
PRR
What do they do? Example of important group of PRR? |
pattern recogn. receptors
all macrophages have identical receptors, e.g. for recognizing groups of pathogens PRR recognize PAMP's (pathogen ass. membrane patterns) Toll-like receptor are PRR expressed on dendritic cell, mast cells, eosinphils |
|
|
What are two results of TLR recognize PAMP on an object in the body?
|
Phagocytosis
Production and secretion of cytokines, |
|
|
NK cells kill ?
What inhibit NK cells? |
antibody coated cells (not expressing MHC-I)
|
|
|
Virally infected cells produce what?
This attracts? |
INF-a
NK cells |
|
|
2 example hapten protein complex
|
1. albumin + penicillin
2. PI toxin + skin |
|
|
Exogenous antigen
Where made? Processed by? MHC molecule presented with? |
Antigen made by the pathogen outside any host cell.
Processed by APC (like macrophage), presented on surface w/MHC-II |
|
|
Endogenous antigen
Where made? Processed by? MHC molecule presented with? |
made by intracellular pathogen inside inf.host cell e.g. virus replicates and makes viral protein inside host cell expressing MHC-I
Inf. cell lysed cytotoxic T cell (CD8+) |
|
|
Mature DCs are best for ?
Immature DCs are good at ? |
Mature DCs are best for processing and presenting antigen.
Immature DCs are good at antigen capture. |
|
|
What is the term for an MHC molecule to form a variable region (ability to express a number of different MHC molecules)?
|
MHC polymorphism (MHC Allelic Diversity)
|
|
|
What is MHC restriction?
|
Ag can only trigger an immune response if they are bound to a self-MHC molecule
|
|
|
How can a particular pathogen be expressed on MHC-I and MHC-II at the same time, stimulating T-helper and CTL?
|
Cross-priming
|
|
|
What is the term for a circumstance when exogenous antigens may enter the edogenous antigen pathway?
|
Cross-prsentation (cross-priming)
|
|
|
Present ENDOGENOUS antigen … originates within the body’s own cells. The foreign proteins being made inside infected cell reside within the ______ of the infected cell and are not inside a ____.
|
Present ENDOGENOUS antigen … originates within the body’s own cells (NOT phagocytosed material). The foreign proteins being made inside the infected cell reside within the CYTOPLASM of the infected cell and are not inside a PHAGOSOME .
|
|
|
Heat-shock proteins (HSP):
|
Molecular chaperones where they can direct other proteins through cell when under stress
bind [endocytosed] exogenous viral antigens shuttles to endogenous pathway. (facilitate cross presentation type) Example: killed virus vaccine consists of killed virus particles. Viral particles taken up by APCs and thus are taken into EXOGENOUS pathway. Then HSP can shuttle these antigens into the ENDOGENOUS pathway and stimulate a CTL response via MHC-I presentation of antigen to CTLs. |
|
|
True or Falso:
APC can present both MHC I and MHC II-bound Ag at the same time |
True, both these are different molecules!
MCH I presents to CTL MCH-II presents antigen to Th (CD4+) via extracellular Exogenous pathway |
|
|
What can defective somatic gene rearrangement lead to?
|
Severe immunodeficiency
|
|
|
What type of molecules regulate lymphocyte function?
|
Receptor molecules
Co-stimulatory molecules Adherence molecules MHC molecules |
|
|
What are some types of receptor molecules for lymphocytes?
|
Antigen receptors (TCR, BCR)
Receptors for cytokines (CD25) Receptors for antibody (FcR) Receptors for complement proteins |
|
|
How are subsets of T-lymphocytes defined?
|
By specific molecules they express and the functions they do
|
|
|
Are all TCRs on the same cell identical and bind the same epitope?
|
Yes (check on this)
"BCR and TCR are clonal=all progeny from a mature B?T cell express identical antigen receptors/recognize identical epitopes of antige" |
|
|
Would Bursectomized newborn chicks reject skin grafts?
|
yes, would still have T cells and CMI response
|
|
|
Can APC (like B cells) express endogenous antigen?
|
Yes, although usually associated with exogenous Ag, APC have nuclei and can be infected with virus e.g. Boivine Leukemia Virus. Endogenous Ag is processed and presented to CTL.
|
|
|
What are some types of receptor molecules for lymphocytes?
|
Antigen receptors (TCR, BCR)
Receptors for cytokines (CD25) Receptors for antibody (FcR) Receptors for complement proteins |
|
|
How many TCR-MHC peptide interactions are needed to stimulate a single CD4 T-cell?
|
1,000
|
|
|
How many types of T-helper cell subsets are there? What are they?
|
Th1 - (CMI) secrete IL-2 and Interferon-y
Th2 - secrete Interleukin-4 and 5 |
|
|
Th1 secrete
|
IL-2. Activates other T-cells, B cells and NK cells
* Interferon-y: also made by some other cells; activate macrophages primarily and thus promotes cell-mediated response.. Thus, promotes resistance to intracellular pathogens. Think CMI when you think of Th1 cells |
|
|
Th2 secrete ?
|
* Interleukin-4 and-5
stimulate B cell proliferation and antibody secretion… Thus, promote resistance to extracellular pathogens *Think Humoral Immunity when you think of Th2 cells |
|
|
How many Th cells does B cell need to be fully activated?
|
Usually B-cell will need help from 2 Helper T-cells (Th2) to become fully activated -> plasma cells.
|
|
|
Antibody plasma cells makes
Is identical to ? |
Antibody plasma cells makes
Is identical to the aB bound to the B-cell (BCR) that gave rise to the plasma cell. (It's a secreted BCR) |
|
|
What immune cells have receptors for Fc part of Ab and for complement?....Can kill target cells by releasing perforin from granules, and are important in viral immunity and defense against tumors.
|
Natural killer (NK) cells
|
|
|
Would neutrophils express antigen or MHC type II on surface?
|
No, because neutrophils are not APC.
APC include macrophages, B cells, dendritic cells, etc |

