![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is NETs |
Neutrophil extracellular traps- after neutrophils become activates by IL-8 or LPS, neutrophils secrete out their granule proteins and chromatin, forming an ec fibrous network, which attracts and kills microbes |
|
|
|
How does the receptor mediated endocytosis work |
Specific binding of ligand and receptor occura at the cell membrane. Then the receptor ligand complex move to clathrin coated pits, where it forms an invagination. Once inside the cell as a vesicle, the clathrin coat gets removed and the receptor and ligand separate; receptor vesicle gets transported to the cell membrane where it fuses and gets exocytosed. Whereas the ligand containing vesicle becomes an endosome and gets sent to the Golgi ehrre it becomes processed. |
|
|
|
How does pinocytosis work and how is it different from receptor mediated endocytosis |
In pinocytosis, small molecules/ligands bind onto nonspecific receptors ,forming an invagination. Receptor and ligand seperate into different vesicles, the ligand containing endosome gets hydrolyzed by lysosomes and the receptor vesicle gets exocytosed. Pinocytosis requires a large amount of ATP and generates little amount of ATP. It is also non specific. |
|
|
|
What are NK cells |
They are lymphocytes of the innate immunity system. They can recognize stressed cells without the MHC on its surface, thus can provide a fast immune response |
|
|
|
What are Fc receptors |
They are proteins found on several immune cells, including phagocytes, macrophages, neutrophils, etc. Fc receptor is where the antibody on the pathogen binds on, allowing these cells to identify and remove the microbial pathogen |
|
|
|
What is the major basic protein? |
Proteoglycan 2(PRG2) A protein residue secreted by the eosinophil granules. It is a potent enzyme against helminths and is toxic towards bacteria. It stimulates mast cells and basophila to secrete histamine, and activates neutrophils and alveolar macrophages |
|
|
|
What is the NADPH oxidase |
It's a membrane associated enzyme found in neutrophils that reduces O2 into O2- (superoxide, free radical) and NADP+. It is used to kill invading bacteria by releasing free radicals |
|
|
|
What are the functions of neutrophils |
Degranulation, phagocytosis, NaDph oxidase dependent killing, adhere onto the vasvular endothelium which increases vascular permeability, produce NETs |
|
|
|
Which chemokine mainly attracts neutrophils |
iL8 |
|
|

What kind of phagocytosis is this |
Receptor mediated endocytosis |
|
|
|
How does AMP attack and harm invading microbes |
By targeting the LPS layer of the cell membrane and forming pores on it, causing efflux of essential ions and nutirents |
|
|
|
What is antimicrobial peptides (AMP) |
Another mode the innae immunity uses to kill invading microbes. it is also called the cationic host defense peptide which can kill both gram +and -bacteria, enveloped viruses, fungi and even cancerous cells. |
|
|
|
What is the respiratory burst |
When immune cells such as macrophages and neutrophils quickly release ROS when in contact with bacteria |
|
|
|
What is the function of NADPH oxidase (NOX)? |
Found in neutrophils. Produces superoxide radicals by reducing O2 to O2-, then to H2O2. |
|
|
|
Which two proteins can NK cells release to cause degranulation and what are their function |
Perforin (pore forming cytolytic protein) is secreted first, then once pores form, granzymes( induce apoptosis)are able to diffuse through the damaged cell and induce apoptosis |
|
|
|
Gram - bacteria cell wall contains what carb |
LPS |
|
|
|
Which PRR binds to the LPS of gram neg bacteria to induce innate immunity? |
TLR4 |
|
|
|
What is the process of cytokine release via the interaction of TLR and PAMP? |
TLR and PAMP of the microbe bind, which sends a signal to the receptor, which triggers its gene to release cytokines |
|
|
|
What is CD14 |
A PRR; a surface receptor for bacterial LPS |
|
|
|
What is within bacterial dna that makes it play a significant role in the innate immunity? |
Unmethylated dinucleotide cytosine guanosine (CpG) |
|
|
|
What can CpG do that makes bacterial dna important in the innate immunity |
CpG can bind and activate many sentinel cells via their TLR9 |
|
|
|
Function of bacterial LPS in the innate immunity |
LPS released from Gram neg bacteria binds on to LPS binding protein (lbp). lBP then transersbLPS molecules onto CD14. But since CD14 is a surface receptor which does not penetrate the cell membrane, it has to bind onto TLR4 in order to signal cells. Now the lps molecules can bind onto the CD14/TLR4 complex, |
|
|
|
What complex does bacterial LPS molecule bind onto |
CD14/ TLR4 complex |
|
|
|
What does bacterial LPS bind onto |
LPS binding protein (LBP) |
|
|
|
Mature macrophages in the CT are called |
Histiocyte |
|
|
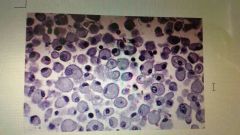
What type of cell is displayed here |
Macrophage |
A lot of cytoplasm, single beanlike round nucleus |
|
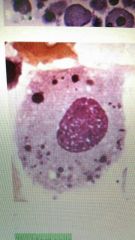
What is this |
Macrophage |
Has organelles in the large cytoplasm, round and large nucleus |
|
|
What causes mast cells to degranulate and release histamine |
The binding of the antibody IgE with the antigen of the invading microbe triggers the degranulation of mast cells, thus activating it |
|
|
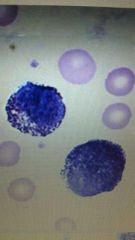
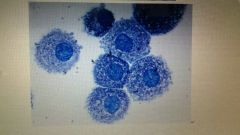
Whats this |
Mast cell |
Toluidine blue stain, highly granulated cytoplasm, nucleus masked by the granules |
|
|
Mast cell |
|
|
|
What do cytokines secrete |
Superoxides, leukotrienes, prostaglandin |
|
|
|
What is TNF α |
A type of cytokine released by macrophages or mast cells |
|
|
|
Functions of TNF α |
1) stimulates the macrophages to secrete IL-1, and together, they trigger critical changes of the vascular endothelial cells,causing cardinal signs of inflammation 2) attract neutrophils to sites of inflammation, increasing their adherence to vascular endothelium 3)stimulates the release of prosaglandin E2, oxidants 4)activates mast cells |
|
|
|
what is septic shock |
A sepsis induced hypotension that leads to tissue hypoxia |
|
|
|
What is an opsonin |
Any molecule that binds onto an antigen, marking it for the recognition of a phagocytic cell to engulf it |
|
|
|
What are the 3 main functions of complement proteins? |
Opsonization, form the membrane attack complex, enhance inflammation |
|
|
|
What is opsonization? |
It is when compliment proteins coat the antigen of invading microbes with opsonin, allowing phagocytes to easily engulf the pathogens |
|
|
|
What is the membrane attack complex |
When compliment proteins lyse the invading pathogen,causing efflux of ions and nutrients |
|
|
|
The end goal of the three compliment pathways is |
To cleave C3 to c3a and c3b |
|
|
|
C3a function |
Enhances inflammation |
|
|
|
C3b function |
Induce opsonization and MAC |
|
|
|
Describe the lectin pathways(2) |
1) the CP ficolin binds onto the olygosaccharide of the pathogen. MASP1&2 (bound to MBP)will then induce the cleavage of C4 to c4a and c4b, as well as the cleavage of C2. Then c4b and c2 forms the c4b2a/C3 convertase 2) the CP ficolin binds onto the mannose of the pathogen, which then activates the MASP1&2 to cleave C4 and C2 to form the C3 convertase from c2a annd c4b |
|
|
|
Describe the alternative pathway |
Circulating c3b in the plasma (cleaved from C3) will bind onto the LPS of the pathogen. Then factor d will trigger the binding of factor b to c3b , forming the C3bB complex(factor b cleaves into Bb and Ba). C3b and factor Bb forms the C3bBb complex, which then forms the C3 convertase. C3 convertase then cleaves to c3a and b. The binding of c3b onto c3bBb forms C5, which is regulated by Properdin. |
|
|
|
What are acute phase proteins |
Secreted by the liver in response to inflammation. Include the mannose binding lectin, complemebt proteins, c-reactive protein |
|

