![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Myeloid stem cell
|

Determined by chemical mediators, differentiate into RBC's, megakaryocytes, macrophages, granulocytes, dendritic cells or mast cells
|
|
|
Lymphoid stem cell
|

Lymphoid stem cells further differentiate into dendritic cells, t-cells, b-cells, and NK lymphocyte cells
|
|
|
Innate Immunity
|
Begins immediately in response to tissue damage
|
|
|
physical barriers
mechanical barriers chemical barriers |
- Skin, mucous membranes
- Ciliary beating, blinking, sneezing - pH of skin, stomach acid |
|
|
Phagocytosis
|
Cells are attracted to a specific site of infections or tissue damage in order to engulf and destroy pathogen
|
|
|
Cytokines
|
Small signaling proteins
- signal increased expression in adhesion molecules - attract leukocytes to infection site - increase fluid that leaves circulation - signal bone marrow to produce more leukocytes |
|
|
Chemokines
|
molecules that set neutrophils and monocytes in motion via chemotaxis (signal via certain chemicals in their environment). Locally produced throughout body
|
|
|
Adaptive immunity
|
Highly specialized, systemic cell and processes that eliminate pathogenic growth
- Antigen specific, only in vertebras - quicker and stronger response to repeat infection - efficient enough that symptoms don't develop - can be long lasting, but usually not permanent |
|
|
Adaptive immunity repsonse
|
Synthesis of anti-body to antigen and promote elimination
- T-cell (CD4= T helper cells, CD8= T cytotoxic cells) killing of virus infected cells - T-cell activation of macrophages to destroy phagocytized pathogens resistant to destruction |
|
|
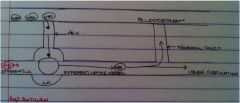
Innate and Adaptive Immunity
|
Work together to fight off infection
- Innate = fast, immediate response - Adaptive = slow, more "potent" response |
|
|
Primary lymphoid organs
|
White cells develop and mature:
- Bone marrow - B cells and Hematopoiesis - Thymus - where T cells finish development |
|
|
Secondary (peripheral) lymphoid organs
|
Function to bring together leukocytes and Ag
- Lymph nodes - collect Ag from tissue - Spleen - blood born antigens encounter immune system - MALT - mucosa-associated lymphoid tissue (respiratory tract, appendix, peyers patch (lymph tissue of gut)) |
|
|
Trafficking of Immune Cells
|
WBC = T and B cells, enter lymph node via HEV (high endothelial venuoles); hang out, do not need to be in contact with Ag to leave, can leave whenever and continue trough lymph circulation or bloodstream
|
|
|
Lymphocytes
|
Small round cells with a large nucleus
- Antigen specific leukocytes - Adaptive are called B and T cells - Each lymphocyte recognizes one specific antigen with receptor - Each lymphocyte has ~100k identical copies of its membrane antigen receptor |
|
|
Membrane Immunoglobulin or B cell receptor or Antibody
|
Antigen receptor on B-Lymphocytes (antibody)
- antibodies can bind both protein and non-protein Ag - the site on the Ag where it is bound is called the epitope |
|
|
T Cell Receptor
|
The antigen receptor on T Lymphocytes
- TCR needs to be presented Antigen by an Antigen presenting cell for it to function (macrophages, b cells, and dendritic cells) |
|
|
Immune Repetoïre
|
the ability of lymphocytes to undergo recombination to be able to be specific to millions of different Antigens creates a very large immune repertoire
|
|
|
Mature Naive T and B cells
|
Those that have not yet bound nor encountered foreign anti-bodies
- If a lymphocyte binds an Ag it proliferates into a clone of antigen eliminating effector cells (plasma, T cell, T helper) |
|
|
Primary response
|
1-2 week response time needed for specific T and B cells to activate
- memory cells for this antigen are also produced at this same time |
|
|
Secondary response
|
After repeat exposure to the same antigen the response is faster, stronger and longer lasting - due to expansion of memory lymphocytes formed during initial exposure
|
|
|
Response to antigen
|
In most cases the body is bombarded with antigens at any given time, the brisk immune response keeps microbial replication under control
- only after a certain threshold has been reached do symptoms present themselves |
|
|
Active adaptive immunity
|
- Natural infection with the organism
- Vaccination with a killed or weakened (attenuated) pathogen, or inactivated (toxoid) - takes 1-3 weeks to become established and may be very long lasting (years to lifetime) |
|
|
Passive adaptive immunity
|
From an immune person by the transfer of antibodies
- starts protection as soon as the antibodies are transferred - lasts only weeks as transferred antibodies are removed from circulation by process called turnover - ex: anti-venom after a snake bite |

