![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
87 Cards in this Set
- Front
- Back
|
Immunology def |
*the study of mechanisms that protect living organsims from infection, injury or challenge |
|
|
Immune system charac. |
*specificity *memory *mobility *replicability *cooperativity |
|
|
consequences of immunity |
*natural resistance *recovery *acquired resistance |
|
|
Deficiency of immune system lead to |
*many disorders *allergy *transplant rejection *autoimmune disorders are undesirable consequences |
|
|
1st line of defense |
*unbroken skin and mucosal membranes *normal flora *secretions (mucous in nose and nasopharynx, sebum and lactic acid, ear wax, secretion in GI and urinary tracts) *tears, cilia, stomach acid |
|
|
Nonspecific (natural) immunity |
*natural or innate, inborn *no production of protective ab *depends on species, race or strain and gender |
|
|
Nonspecific immune response |
*major physiologic processes are: Phagocytosis activation of complement inflammation *body defenses
|
|
|
Cells of immune system |
*specific cellular immunity *the lymphocyte (20% of circulating WBCs, arise from hematopoietic stem cells)
|
|
|
Primary Lymphoid organs |
*bone marrow *thymus |
|
|
Secondary lymphoid organs |
*spleen *lymph nodes *appendix *tonsils *other mucosal associated lymphoid tissues *have contact w/ foreign ag |
|
|
Segregated w/in the secondary organs according to function |
*effector T lymphs are regulator *B lymphs produce ab |
|
|
Primary lymphoid organs |
*stem cells initially in yolk sac, later in the liver *at birth, bone marrow takes over this role *main source of hematopoietic cells *lymph stem cells are released and go to primary lymphoid tissues for further maturation |
|
|
Primary lymphoid cells maturity |
*T cells develop in thymus *B cells develop in bone marrow |
|
|
thymus |
*present at birth, atrophies after puberty *produces enough virgin T cells so isn't needed later on *surface ag are acquired in a voyage from the cortex to medulla *mature T lymphs are released from medulla |
|
|
Purpose of secondary lymphoid organs |
*mature T & B cells are released and migrate to secondary organs *lymphopoiesis occurs here, strictly dependent on antigenic stimulation |
|
|
Surface markers |
*proteins are used to differentiate T cells and B cells and developmental stages *CD classification, clusters of differentiation *2 Mature T-cell populations are created helper or inducers cytotoxic or suppressor |
|
|
B cell surface markers!!!! |
*exhibit IgM and IgD on surface *Plasma cells have lots of cytoplasmic igg |
|
|
cell mediated immunity |
*regulatory proteins produced by the T lymphs *memory cell production *enhancing killing of tumor cell or virally infected cells *maturation of stem cells |
|
|
lymphokines |
*part of cell mediated immunity *chemical messengers that influence the activities of other cells -regulate immune response -proliferation of T & B cells -B cell igg class switching |
|
|
cytokines |
*made by cells other than lymphs *autocrine stimulation *paracrine stimulation *regulatory role in the inflammatory response *interleukins, interferons, tumor necrosis factors |
|
|
PMNs |
*largest pop. of leukocytes in peripheral blood *phagocytes w/ distinct granules (contain acid hydrolases, microbicidal proteins, proteases) |
|
|
eosinophils |
*less than 3% of circulating leukocytes *common progenitor cell w/ PMNs *less efficient at phagocytosis *role is not known, suggest ingestion of immune complexes & limiting inflammatory rxns *clearing of parasites and a role in allergic response |
|
|
mediator cells |
*release of biochemical substances *mast cells, basophils, and platelets *activities include inc. vascular permeability, smooth muscle contraction, augmentation of inflammatory response |
|
|
Mononuclear phagocyte system (MPS) |
*formerly reticulendothelial system *tissue macrophages in spleen, liver, lymphoid tissues and circulating monocytes *liver kupffer cells are the most active (others alveolar, lymph node, splenic macrophages) *phagocytic process stimulates macrophages to become secretory cells (synthesize acute phase proteins, proliferate locally in tissues) *ag presentation is a function of macrophages w/ MHC |
|
|
Immunogens |
*trigger the immune response of lymphocytes
|
|
|
Antigen |
*substance that reacts w/ ab (not able to evoke an immune response) |
|
|
influencing factors |
*age *overall health *dose *route *genetic capacity |
|
|
immunologic disease |
*general health and age effect immunity *age-very young and older *nutrition-deficent or excessive intake, error of metabolism, toxic effect and/or allergic rxn *proteins, carbs, and lipids *vitamins and minerals |
|
|
Characteristics of immunogens |
*macromolecular size *chemical composition and molecular complexity *foreignness *processed and presented w/ MHC |
|
|
Epitopes |
*key portion of the immunogen in the immune response *Recognized by B & T cells |
|
|
Haptens |
*nonimmunogenic material *complex w/ larger molecules *can react w/ ab alone (no precipitation or agglutination rxns) |
|
|
autoantigens |
belong to the host |
|
|
alloantigens |
from other members of the host's species |
|
|
heteroantigens |
from other species |
|
|
heterophile ag |
*identical or closely similar structures *cross reacts w/ antibody *infectious mono (heterophile ab) |
|
|
adjuvants |
*substance administered w/ an immunogen that increases the immune response *aluminum salts |
|
|
cellular ag |
*MHC *Nucleated cells (HLA) *autoantigens (failure to recognize self-ag) *blood group ag |
|
|
Antibodies |
*specific glycoproteins *immunoglobulins *found in plasma,tears,saliva,colostrum *Primary function: combine w/ antigen *Secondary interaction w/ another effector ie complement |
|
|
Immunoglobulin classes |
*IgG *IgM *IgA *IgD *IgE |
|
|
Immunoglobulin structure |
*4 polypeptide chains (2 heavy & 2 light--kappa, lambda) *the 4 chains are joined by disulfide bonds *2:1 K to lambda!!! |
|
|
Heavy Chain: Isotype |
*H chain is unique to each Ig Class |
|
|
Heavy chain: allotype |
*genetic variations in constant regions *In four IgG subclasses, one IgA subclass and in the kappa chain |
|
|
Heavy chain: Idiotype |
*variations in variable regions *terminal ends of L and H *antigen recognition site |
|
|
Light Chains |
*kappa & lambda *structural differences, but no functional differences *Bence-Jones proteins (normally found in urine |
|
|
Basic Immunoglobulin structure |
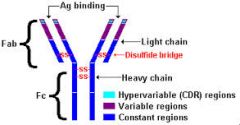
*know where V & C region, hinge, and disulfide bond |
|
|
Papain digestion of IgG |
*yields 3 fragments *2 Fab are identical & are capable of binding specifically w/ ag, but could not cause aggl or ppt rexs (one light chain & one-half of one heavy chain) *1 Fc fragments: 2 halves of 2 heavy chains involved in complement fixation (breaks at hinge), fixation to skin, & placental transport *breaks above disulfide bond |
|
|
IgG treatment w/ pepsin |
*yields a diff. Fab-type fragment *F(ab)'2 *binds w/ ag *capable of causing aggl & ppt rxn *has 2 ag binding sites *2 light chains & 2 halves of heavy chains *breaks below disulfide bond |
|
|
Igg Structure!! |
*each heavy and light chain is composed of a variable domain and 1 or more constant domains *variable domains define specificity *hinge region is located btwn. CH1 & CH2 |
|
|
Igg conclusions |
*variable part provides specificity for binding ag *constant part is associated w/ different biological properties |
|
|
IgG |
*Major ig in adult *can cross the placenta *major functions: crosses the placenta, fix complement, opsonization, toxin and viral neutralization and aggl and ppt rxn *diffuses readily into extravascular spp |
|
|
IgM |
*lg, macromolecule *pentamer held together by a J chain (10 binding site) *found mainly in the intravascular pool *doesn't cross the placenta!! *primary response ab |
|
|
IgM function |
*complement fixation, agglutination, opsonization, neutralization of toxins *most efficient at triggering the classical pathway *surface receptor for ag (presence of membrane IgM classifies lymph as mature B cell) |
|
|
IgA |
*2 subclasses IgA2 is found as a dimer in secretions of respiratory and intestinal tracts and in milk, saliva, tears and sweat *main function is to patrol mucosal surfaces |
|
|
IgD |
*scarce in serum *most is on surface of immunocompetent but unstimulated B lymph *some association w/ certain autoimmune diseases |
|
|
IgE |
*attaches to basophils and tissue mast cells found mainly in the lining of the respiratory & alimentary tract *binding of specific ag by two adjacent IgE molecules causes degranulation of the mast cell (releasing histamine and heparin) *type 1 hypersensitivity or allergic rxn *also triggers acute inflammatory response recruiting neuts and eos |
|
|
Immune Response curve!!! |
*in initial response: IgM is 1st responder, IgG takes over after the decline *in secondary response: IgG has bigger immune response 2nd time |
|
|
Anamnestic response (secondary response)!! |
*re-exposure to same ag *same 4 phases: shorter log phase, longer plateau, gradual decline; IgG is predominant, ab titer higher |
|
|
Ag-Ab interaction |
*specificity -ab chooses one ag over another -combining site on the Fab molecule *cross-reactivity -function of specificity *affinity -attraction--strength of interxn btwn. epitope and ab's ag binding site *avidity (how strong binding is) -measure of overall strength of ab-ag complex |
|
|
Immune complexes |
*small (soluble) or lg (precipitating) *removed from circulation by phagocytic cells *results in disease when normal process doesn't occur |
|
|
ab synthesis |
*antigenicity of a foreign substance is related to presentation to lymph, and route of entry *previous exposure elicits a memory response |
|
|
Primary ab response |
*IgM response in four phases -lag -log -plateau - decline |
|
|
lag |
when no ab is detectable |
|
|
log |
ab titer rises logarithmically |
|
|
plateau |
ab titer levels off |
|
|
decline |
ab is catabolized |
|
|
classic pathway |
*trimolecular complex of C1 (C1q, C1r, C1s), *C4, *C2 are unique to classic pathway |
|
|
Alternate pathway |
*C3w & C3b, factors B, D and properdin activate it |
|
|
Lectin pathway |
*mannose-binding lectin or serum ficolin initiates it |
|
|
Properties of complement |
*role in cytolytic destruction of cellular ag *activity in ag-ab rxn destroyed by heat at 59 for 30 min (c1 and c2) *IgM and IgG only igs that react w!!!! *complement is bound to all ag-ab rxn, if proper ab class *no increase w/ immunization *contribute to chemotaxis, opsonization, immune adherence, anaphylatoxin formation, virus neutralization *can be activate by nonserologic rxn *anticoagulants that chelate Ca2+ and Mg2+ *storage affects C4 *increase vascular permeability *recruit monocytes and neutrophils *don't need ag-ab rxns to activate alternate pathways |
|
|
Classical pathway triggers |
*IgM is the most efficient then IgG, IgG3, IgG1, and IgG2 *C1q can also be activated by (CRP, some viruses, mycoplasmas, some protozoa, certain GN bacteria |
|
|
recognition unit |
*C1qrs complex=1 C1q+2 C1r+ 2 C1s-stabalized by calcium *binding sites on C1q are exposed to the Fc region of 2 adjacent ab molecules *C1q binds ab *proenzyme C1r and C1s become active enzymess |
|
|
Know the complement pathways!!! |
1. classical 2. alternative 3. lectin |
|
|
Membrane attack complex (same in all pathways) |
*C6 binds to C5b, attaches to the cell surface *C7 binds to C5b6 *C5b67 binds hydrophobically to a membrane *C8 attaches forming a transmembrane channel *up to six C9 surround the site to prevent resealing and accelerate lysis |
|
|
alternate pathway recognition unit |
*predominantly a non ab initiated pathway *factor B and D *triggering substances (bacterial/fungal cell walls, yeast, viruses, tumor cell lines, some parasites) |
|
|
Lectin pathway for complement activation |
*ab not present *lectins are proteins that bind to carb *provides nonspecific recognition of carbs that are constituents of microbial cell walls |
|
|
Mannose-binding lectin |
*MBL binds to mannose or related sugars to initiate *Ca dependent *acute phase protein *similar structure to C1q |
|
|
Biological consequences of complement activation |
*amplification *anaphylatoxins *immune adherence *oponization *chemotaxis *kinin activation *lysis |
|
|
alterations in complement levels |
*elevations in complement levels are common and non specific *inflammatory, trauma, acute illness, acute phase response *decreases due to consumption or deficiencies (functional studies, CH50) |
|
|
acute phase response |
*increase hepatic synthesis of plasma proteins *fever, and increase in granulocyte counts
|
|
|
Positive acute phase response |
*CRP *a1-antitrypsin *a2-macroglobulin *fibrinogen *haptoglobin *ceruloplasmin C3 |
|
|
Negative acute phase response |
albumin |
|
|
inflammation |
*redness, swelling, heat and pain *kill the adversary, mop up and repair |
|
|
4 stages of inflammation |
1. vascular permeability 2. emigration of PMNs 3. emigration of mononuclear cells 4. cellular proliferation |
|
|
Specific immunity |
*adaptive, acquired *respond to a specific stimulus, an immunogen *composed of cellular and humoral elements (Major cellular component is the lymph, ab is major humoral) |
|
|
humoral-mediated immunity |
*immunity can be acquired actively or passively
|
|
|
Active humoral mediated immunity |
*natural exposure in response to infection *artificial as in intentional injection of ag *both cases ab is produced by host w/ long duration |
|
|
acquired immunity: passive |
*naturally by the fetus from the maternal circulation (newborn in colostrum) *infusion of serum or plasma w/ high conc. of ab produced in another host can confer artificial passive immunity *in both ab is not produced by the host, and is of short duration |

