![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
|
What are parasites?
|
- Protozoa e.g. Plasmodium spp., Giardia lamblia, Toxoplasma gonii etc
- Fungi e.g. Pneumocystis jiroveci (although this is debateable) - Worms = helminths • Nematodes - roundworms → whipworms, hookworms, pinworms, ascarids, filarids → mostly harmless • Cestodes = tapeworms → mostly harmless • Trematodes = flukes, flatworms, platyhelminthes → tissue fluke e.g. liver fluke → blood fluke e.g. Shistosoma spp. |
|
|
Describe the key elements in immunity to helminths and allergy
|
- By enlarge Th2-type responses
- Key elements are: • IL4 and IL5 • IgE • Eosinophils and mast cells - These interact to generate the production of a range of mediators which together destroy the worm and activates inflammation |
|
|
Describe the induction phase during immune response to helminths and allergy
|
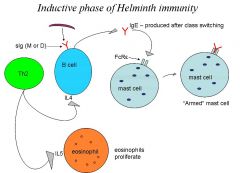
- Sensitization
- APCs activate naive Th0 cells which differentiate into Th2 by co-stimulation by TLR-induced (toll-like receptor) cytokines which promote the Th2 differentiation - Th2 cells drive the proliferation of eosinophils through IL5 - Th2 cells also help the production of IgE through the production of IL4 = help B-cells to class-switch from IgM to become IgE producing plasma cells. It also stimulates B cell to produce the Ab in large amounts - IgE binds to FcRξ on mast cells and eosinophils in a process called arming, and activate eosinphil proliferation |
|
|
Describe why Th1 or Th2 may develop and why this is important
|
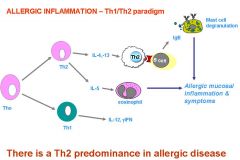
- Th1 develops in response to IFNαβ and IL12
→ developed by cells with PRRs binding components of viruses, or intracellular bacteria e.g. viral dsRNA → cell-mediated immunity - Th2 develops in response to IL4 and IL10 → generated by cells with PRRs binding parasites (and extracellular bacteria) e.g. schistosome egg proteins → humoral immunity - This is important because if the Th1/Th2 balance can be manipulated this will lead to therapeutic strategies e.g. in allergy to reduce the Th2 response (anti-IL4?) e.g. for antiviral vaccines to boost Th1 responses (IL-12 +vaccine) - This may be acieved by targeting PRRs or their signalling proteins |
|
|
What is the difference between HLA class I and HLA class II?
|
- HLA is the name of the major histocompatibility complex (MHC) in humans
- HLA class I antigens present peptides from inside the cell (including viral peptides if present) = enodgenous protein. These peptides are produced from digested proteins that are broken down in the proteosomes. Foreign Ags attract CD8 Tc cells - HLA class II antigens present exogenous peptides to Th-cells, stimulating them to multiply and stimulate B-cells |
|
|
What are the roles of mast cells and eosinophils?
|
- Mast cells are located in tissues = especially in connective tissues underlying surface epithelia (lungs, gut, skin). In healthy individuals most mast cells are in the gut mucosa
- Eosinophils are found both in tissues and in circulation and will home to sites of inflammation - Both mast cells and eosinophils are important in parasite immunity and allergy but the relative important varies with the disease → Mast cells in acute disease or exacerbations? → Eosinophils in late-phase and chronic disease? |
|
|
Describe the effector phase in immunity to helminths
|
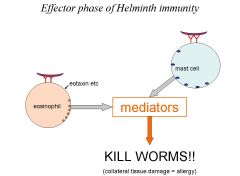
- 'Armed' mast cells and eosinophils generated through sensitization bind worm antigen and degranulate
- The degranulation releases factors that kills helminths and causes inflammation and allergic disease e.g. histimines - However, many other factors may activate degranulation of eosinophils e.g. eotaxin (and other chemokines) which are produced by many cells in response to Th2 cytokines and are chemotactic for eosinophils. Also IL5, stem cells factor, GMCSF, etc |
|
|
Describe the link between helminth infection and allergy
|
- Helminth infections correlate inversely with allergy i.e. are protective
- Hygiene theory suggests that there is increased allergy due to decreased helminth infections as the elimination of pathogens gives the immune response nothing to do, meaning it is more likely to respond to other things instead - Atopy is an inherited propensity to over-produce IgE - Atopic individuals are susceptible to allergy |
|
|
Define atropy
|
Referes to IgE hyperresponsiveness and represents a predisposition to allergic diseases
|
|
|
Define allergy
|
Represents the clinical expression of atopic IgE mediacted diseases
|
|
|
Give 4 common aero-allergens
|
1. Pollen
2. House dust mites 3. Animal dander 4. Fungal spores |
|
|
What are the differences between food allergy and food intolerance
|
Food allergy:
- Mediated by IgE antibody to specific food allergens - Usually manifests within seconds or minutes following exposure - Symptoms could manifest as itchiness, rash (urticaria), swelling or soft tissue (angioedema), wheezing or collapse (anaphalaxis) Food intolerance - Non-IgE mediated - Can occur to any food - Non life-threatening but distressing symptoms - Usually manifests as abdominal discomfort, bloating, vomiting, nausea,diarrhoea, headache, feeling unwell etc - No diagnostic tests - Pathogenesis unknown |
|
|
What are the symptoms of allergic rhinoconjunctivitis?
|
- Sneezing
- Nasal blockage - Rhinorrhoea - Itchy nose/throat/eyes - Watery and sticky eyes - Sinustitis - Impaired concentration and QOL |
|
|
Describe the symptoms of atopic asthma
|
- Dry cough
- Chest tightness - SOB - Wheezing |
|
|
Describe how to diagnoses an allergy
|
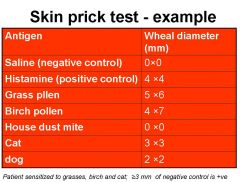
- Clinical history
→ symptoms → temporal association with allergen exposure - Demonstration of specific IgE → Skin prick test (SPT) → Intradermal test (IDT) → RAST (test blood directly for specific IgE - Challenge testing = give person what they are supposed to be allergic to (very dangerous) |
|
|
How would you diagnose someone as being atopic?
|
- Atopic = a tendency to exaggerated IgE antibody production
- Predisposition to develop allergy - Usually defined by the presence of 1 or more positive skin prick tests to common aero-allergens |
|
|
What is food-related exercise-induced anaphylaxis?
|
- Patient sensitised to certain food e.g. peanut
- Is able to tolerate the peanut normally - Is able to exercise normally - Develops anaphylaxis is undertakes exercise following ingestion of peanut |
|
|
Describe the treatments for systemic allergic reactions
|
- Closely observe and monitor PEFR, pulse, BP and symptoms
- Antihistimines = oral fast-acting or parentral as necessary - Bronchospasm = β2 agnonists inhaler or nebuliser as necessary - Hydrocortisone = 100mg IV/IM stat in grade 3-4 reactions - Oxygen = 60-100% - In severe angioedema or anaphylaxis: treat early with 1:1000 adrenaline IM (0.5-1 mg stat), repeat dose if no improvement. Keep 1:10,000 adrenaline for very slow IV use just in case. - On dischage: → continue antihistimines for 2-3 days e.g. T. clarityn 10mg/d → Step-up asthma treatment fir 3-5 days → Consider oral steroids - rapidly reducing the course for 3-5 days → Written self-management plan for treatment of acute allergic reactions, emergency kit and epipen training |
|
|
What is contact dermatitis?
|
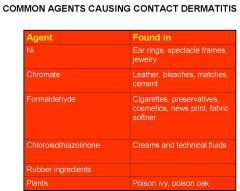
- Different from immediate (type I) hypersensitivity
- Type IV hypersensitivity - Symptoms occur 24-72 hours following exposure to the causative agent - Mediated by T-cells causing inflammation and oedema in the skin - Caused by low molecular weight substances (<1kDa) called 'haptens' that have to link to 'carrier' proteins to form antigens - Not the same as irritant dermititis, where there is direct damage of the cells e.g. due to heat or chemicals |
|
|
Describe the incidence of asthma in the UK
|
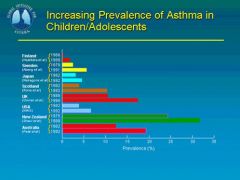
- UK has one of the highest asthma prevalences in the world
- In many countries there is increasing incidence of asthma in all age groups |
|
|
Describe the burden of allergic disease in the UK
|
- GP prescriptions for asthma and allergy cost 10% of all precription costs = £5.6bn
- Over 18 million people in the UK have at some point been diagnosed as having allergic illness - In any year >20% of the populations (20 million) have active allergy and are likely to be receiving treatment - 10% of children and adults <40 have greater than 2 atopic disorders - Hospital admission for serious anaphylaxis has increased 7 fold and admissions for food allergy have increased 5 fold in the last decade - Allergy costs the NHS £900m/year - 6% of GP consultations are for allergic diseases |
|
|
Describe some of the possible reasons for the rising prevalence of allergies
|
- Outdoor environment = air pollution (not directly linked to asthma, but does worsen asthma symptoms)
- Antibiotic usage - Indoor environment = housing conditions - Diet - Intrauterine factors and environment - Maternal smoking during pregnancy - Pet ownership - Cleaner environment and less infections so less endotoxin exposure in early life - E.g. Allergies less prevalent in East Germany compared to West Germany, despite having a less clean environment, less pets, non-insulated houses, larger families and lower SE status than those in West Germany |
|
|
Describe the long-term treatment of allergic diseases
|
- Allergen avoidance
- Patient education - Symptomatic relief = antihistimines - Antiinflammatory therapies: • Topical steroids (inhalers, nasal sprays, ointments) • Leukotriene antagonists • Cromones = sodium cromoglycate (stabilise mast cells and stop degranulation) - Immunomodulatory therapies • Specific allergen immunotherapy (desensitisation) • Anti-IgE mAb • SIT + IgE • Peptide immunotherapy • DNA vaccines being investigated in clinical trials |
|
|
What are the 4 classifications of hypersensitivity disorders?
|
1. Type I
- Known as immediate or anaphylactic hypersensitivity - The reaction may involve skin (urticaria and eczema), eyes (conjunctivitis), nasopharynx (rhinorrhea, rhinitis), bronchopulmonary tissues (asthma) and gastrointestinal tract (gastroenteritis). - The reaction usually takes 15 - 30 minutes from the time of exposure to the antigen, although sometimes it may have a delayed onset (10 - 12 hours). - Immediate hypersensitivity is mediated by IgE. The primary cellular component in this hypersensitivity is the mast cell or basophil. The reaction is amplified and/or modified by platelets, neutrophils and eosinophils. - IgE has very high affinity for its receptor on mast cells and basophils. A subsequent exposure to the same allergen cross links the cell-bound IgE and triggers the release of various pharmacologically active substances - Cyclic nucleotides appear to play a significant role in the modulation of immediate hypersensitivity reaction, although their exact function is ill understood. Substances which alter cAMP and cGMP levels significantly alter the allergic symptoms. Thus, substances that increase intracellular cAMP (e.g. adrenaline) seem to relieve allergic symptoms, particularly broncho-pulmonary ones, and are used therapeutically - E.g. asthma 2. Type II - Cytotoxic hypersensitivity / antibody dependent - May affect a variety of organs and tissues - Reaction time is minutes to hours - Primarily mediated by antibodies of the IgM or IgG classes and complement - The antigens are normally endogenous - Treatment involves anti-inflammatory and immunosuppressive agents. - E.g. Goodpasture's syndrome, autoimmune haemolytic anaemia, thrombocytopenia 3. Type III - Immune complex hypersensitivity - The reaction may be general, or involve individual organs e.g. skin, joints, kidneys, lungs - May take 3-10 hours after exposure to the Ag - It is mediated by soluble immune complexes and complement. They are mostly of the IgG class - The Ag may be endogenous or exogenous and is soluble and not attached to the organ involved - The damage is caused by platelets and neutrophils - E.g. SLE, arthus reaction, rheumatoid arthritis 4. Type IV - Cell mediated or delayed type hypersensitivity - The classical example of this hypersensitivity is tuberculin (Montoux) reaction which peaks 48 hours after the injection of antigen (PPD or old tuberculin). - The lesion is characterized by induration and erythema. - May be one of three types: • Contact = 48-72 hours. Causes eczema by lymphocytes follwed by macrophages. Epidermal contact antigen • Tuberculin = 48-72 hours. Appears as local induration caused by lymphocytes, monocytes and macrophages. Intradermal antigen e.g. tuberculin, lepromin • Granuloma = 21-28 days. Appears as a hardening caused by macrophages, epitheloid and giant cells, and fibrosis. Caused by persisitant antigen or foreign body presence (TB, leprosy etc) - Cytotoxic T cells (Tc) cause direct damage whereas helper T (TH1) cells secrete cytokines which activate cytotoxic T cells and recruit and activate monocytes and macrophages, which cause the bulk of the damage - Corticosteroids and other immunosuppressive agents are used in treatment. - E.g. contact dermatitis, chronic transplant rejection |

