![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
Complement is a _______ system
|
cascade
|
|
|
How many cascade systems of molecules are present in plasma? What are their names?
|
Four. Complement, clotting, fibrinolytic and kinin
|
|
|
What do cascade systems respond to? What to do they induce?
|
Respond to tissue damage, induce inflammation (Complement most important in relation to infection)
|
|
|
Complement is the most important cascade system in relation to...
|
...infection
|
|
|
What are the main roles of the cascades other than complement?
|
Tissue repair
|
|
|
What is a cascade?
|
An entire series of reactions which occurs as a result of a single trigger reaction or compound
|
|
|
What does activation of the complement cascade system result in? (3)
|
Inflammation
Enhanced Phagocytosis Cell lysis |
|
|
What does the complement cascade do? (Also, where does its name originate from?)
|
It 'complements' (enhances) the ability of antibody to dispose of microorganisms
1757121110 |
|
|
There are inhibitors of complement. What is the point of these?
|
They prevent complement from damaging own cells
|
|
|
What is the central component of complement?
|
C3 - it is a major serum protein (the clear liquid that separates from blood on clotting)
|
|
|
What leads to activation of C3?
|
The enzymatic splitting of it
|
|
|
If activation of C3 occurs on the surface of a bacterial cell, most of the C3 is left in the form of the cleavage fragment ___. The function of ___ is to...
|
C3b. Mark out the bacterium for phagocytosis (phagocytic cells have receptors that recognise and attach to C3b)
Bacteria is now said to be OPSONISED |
|
|
What is opsonisation?
|
The process by which bacteria are altered in such a manner that they are more readily and more efficiently engulfed by phagocytes.
E.g. C3b attachment to bacteria is an example of opsonisation |
|
|
Other than to be a marker for phagocytes, what is the other use for C3b?
|
To act as a focus for other complement components (C5,6,7,8,9) to collect and form into small pores that puncture the cell membrane and make it leak --> Leading to death (lysis)
|
|
|
Lysis by membrane attack complex is less important than C3b attachment, normally. However, for which species is this not true?
|
With the Neisseria species
|
|
|
What is the function of C3a? What does it combine with to achieve this?
|
Its function is to promote inflammation - achieved by working together with C5a
|
|
|
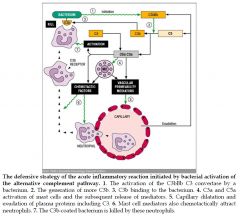
How do C3a and C5a promote inflammation?
|
By attracting neutrophils and activating mast cells
|
|
|
How does attraction of neutrophils and active mast cells cause inflammation?
|
Local vascular permeability increases
|
|
|
What happens as a result of inflammation?
|
Neutrophils, monocytes, antibodies and more complement flow into the tissues
|
|
|
Collectively, C3a and C5a are known as...
|
Anaphylatoxins (Any of several toxic substances that trigger anaphylaxis (An acute allergic reaction to an antigen))
|
|
|
What are the three ways cleavage of C3 can occur?
|
ALTERNATIVE PATHWAY: Spontaneously on the surface of cells (e.g. bacteria) with help from factors B, D and Properdin. Produces C3bBb which converts C3 into C3a and C3b
CLASSICAL PATHWAY: Requires *presence of antibody*. C1q, C1r and C1s bind to antibody attached to pathogen --> Activation of C4 and C2 forms classical pathway C3 convertase (C4b2a) which cleaves C3 into C3a and C3b LECTIN PATHWAY: Antibody *independent*. Triggered by microbial surface sugar recognition by MBL and by MASP-1 and-2 |
|
|
What helps C3 cleave on the surface of some cells like bactera?
|
Factor B, Factor D, properdin. Produces enzyme C3bBb (alternative pathway C3 convertase)
|
|
|
What does the classical pathway of cleavage of C3 require?
|
Antibody
|
|
|
Describe the lectin pathway
|
Mannose-binding lectin binds to mannose residues on carbohydrate or glycoprotein components of microorganisms including bacteria
MBL forms a complex with MASP-I (Mannan-binding lectin-Associated Serine Protease) and MASP-II, two protease zymogens. MASP-I and MASP-II are very similar to C1r and C1s molecules of the classical complement pathway When the carbohydrate-recognising heads of MBL bind to specifically arranged mannose residues on the phospholipid bilayer of a pathogen, MASP-I and MASP-II are activated to cleave complement components C4 and C2 into C4a, C4b, C2a, and C2b. C4b and C2a combine on the surface of the pathogen to form C3 convertase (C4b and C2a --> C4b2a), while C4a and C2b act as chemoattractants. |
|
|
Where are receptors for complement found? (3)
|
Phagocytes
Erythrocytes B lymphocytes |
|
|
How does the Epstein-Barr virus infect?
|
It uses receptors for complement on B-cells to attach to them and infect, causing glandular fever.
|
|
|
What attracts phagocytes to where they are needed?
|
Chemotactic gradients (complement is important in regard to this, as well as microbial and other immunological molecules)
|
|
|
How does the phagocyte attach to the bacterium?
|
*Pattern recognition receptors* (PRRs) on the surface pf phagocyte recognise *pathogen-associated molecular patterns* (PAMPS) on the surface of the microbe.
Binding is enhanced if complement or antibody has coated the microbe, and they are recognised by corresponding complement receptors and receptors for antibody (Fc receptors) on the phagocyte |
|
|
What are Fc receptors?
|
Receptors on phagocytes that recognise antibody on a bacterium.
Bacterium with antibody on them are easier to engulf There are also 'complement' receptors |
|
|
When the bacterium is taken into the phagocyte, it is said to be in a...
|
...phagosome
|
|
|
What does the lysosome destroying the bacteria contain?
|
Oxygen free radicals and granules possessing toxic proteins
|
|
|
The fused phagosome and lysosome is referred to as a...
|
...phagolysosome
|
|
|
When a phagocyte engulfs a microbe there us usually a __________ _____ during which there is generation of microbicidal...
|
'respiratory burst'. Generation of microbicidal oxygen free radicals (inc. superoxide - leading to production of hydrogen peroxide and hypochlorite)
|
|
|
What are the ways of non-oxidative killing? (4)
|
Lysozyme
Defensins (produced in the milk of the mother) Lactoferrin Protease |
|
|
What are the oxidative killing methods?
|
Reactive oxygen intermediates (O2- (superoxide), H2OH, OH' (hydroxyl radical) OCL- (hypochlorite))
|
|
|
What are the nitric oxide-relating killing methods?
|
Reactive nitrogen intermediates
|
|
|
Where are mast cells found?
|
CT, skin, lung, intestine
|
|
|
What is the term used when mast cells release the contents of their granules?
|
They are said to 'degranulate'
|
|
|
What does degranulation of mast cells achieve?
|
It helps initiate the acute inflammatory response
|
|
|
What do the granules in mast cells contain a lot of? What does it act on?
|
Histamine. Acts on blood vessels and smooth muscle
|
|
|
What does histamine release cause?
|
Increased blood flow to area and process of damage-limitation and control of infection begins.
|
|
|
Which complement components stimulate mast cells?
|
C3a and C5a and specific antigen (when sensitised by IgE antibody)
|
|
|
Mast cells are involve with innate/adaptive immunity
|
Both
|
|
|
Blood basophils are very similar/different to mast cells
|
Similar
|
|
|
When can inflammatory response be dangerous?
|
When it occurs in a limited area like the airways or brain, or if it leads to breakdown of vital tissue (e.g. burst appendix)
|
|
|
What is the intention of inflammatory response?
|
Restricting infection, limiting tissue damage and initiating repair
|
|
|
.
|
|
|
What part of complement triggers mast cells to release inflammatory mediators?
|
C3a and C5a
|
|
|
What part of complement is a chemotacic factor for neutrophils and macrophages?
|
C5a
|
|
|
What complement parts trigger lysis of cells? (By punching holes in cell membranes)
|
C5b - 9
|
|
|
Which part of complement causes opsonisation?
|
C3b
|
|
|
Which part of complement helps with transport of immune complexes?
|
C3b
|
|
|
RBCs have complement T/F
|
T
|
|
|
RBCs can take immune complexes (Erythrocytes with complement and antibody on them) to which organs?
|
The spleen and liver
|
|
|
Prokaryotes often have which sugar at the end of their cell membrane chains? Why is this important?
|
Mannose. Used for Mannose Binding Lectin (MBL) - important in phagocytosis
|
|
|
What is the C3 convertase of the classical pathway?
|
C4b2a
|
|
|
What is the C3 convertase of the Lectin pathway?
|
C4b2a
|
|
|
What is the C3 convertase of the alternative pathway?
|
C3bBb
|
|
|
What happens to C3 if left on its own?
|
It will slowly autocatalyse.
|
|
|
How many molecules of C9 combine when doing cell lysis?
|
7
|
|
|
What is an example of something that PAMP recognises?
|
Exposed mannose
|
|
|
What does a line above C3bBb mean?
|
That it is active
|

