![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
129 Cards in this Set
- Front
- Back
|
how do Autonomic Neurons control organs that are not under voluntary control? |
They innervate organs( supply organs with nerves) |
|
|
What are some examples of of innervated organs (efffectors) |
-cardiac muscle -smooth muscle of visceral organs and blood vessels -glands |
|
|
TRUE or FALSE Autonomic Neurons are part of the PNS |
TRUE PNS is divided between the autonomic system and the somatic nervous system |
|
|
Neurons are ________, but there are sensory neurons from the _______for control |
-motor |
|
|
Define Viscera |
the organs in the cavities of the body,especially those in the abdominal cavity. |
|
|
Differences between somatic and autonomic |
Somatic motor neurons - have cell bodies in the sinal cord -One Neuron (travels from spinal cord to effetor Autonomic Motor System -has 2 sets of neuronsn in PNS -First has cell bodies in the brain or spinal cord and synapses in an autonomic ganglion -Second has cell bodies in the ganglion and synapses on the effector |
|
|
Types of paralysis in Upper Motor Neuron |
Classic Paralysis -spactic paralysis found in UMN lesions |
|
|
Types of paralysis in Lower Motor Neuron |
Paralysis |
|
|
Where would you find hypo-reflexia? |
In LMN |
|
|
Where would you find hyper-reflexia? |
In UMN |
|
|
Define hyper-felxia |
overactive or overresponsive reflexes |
|
|
Define Hyporefelxia |
condition of below normal or absent reflexes (can be tested using reflex hammer) |
|
|
Pregnaglionic Neurons (within Autonomic Nervous System) |
-originates in the midbrain or hindbrain or from the thoracic,lumbar, or sacral spinal cord |
|
|
Postganglionic Neurons (within Autonomic Nervous System) |
Originate in ganglion then sysnapes in the effector |
|
|
Where are autonomic ganglia located? |
-head,neck, abs |
|
|
Visceral Effector Organs can be cut but will experience atrophy TRUE or FALSE |
FALSE, they can be cut and exp no Atrophy, unlike skeletal muscle |
|
|
Define denervation hypersensitivity |
Elevated response of a nerve or muscle membrane receptor to a transmitter substance following resection or removal of its afferent nerve supply |
|
|
What do Somatic Motor Neurons release, which is always excitatory? |
ACH( Acetylcholine) |
|
|
What two things do Autonomic neurons release, that may be excitatory or inhibitory? |
ACH and NE (Acetylcholine and Norepinepherine) |
|
|
What is CURARE? And what type of muscles will be effected? |
blocks ACH binding also blocks Nicotine Receptors |
|
|
*****What type of muscles are found in the esophagus or rectum? |
check email |
|
|
What happens in the rectum if CURARE is administered? What kind of muscle is found there? |
the external anal sphicter is found there and it will not be able to contract if CURARE is admin |
|
|
Somatic vs Autonomic Effector Organs |
Somatic-skeletal muscles Autonomic-cardiac muscle, smooth muscle, and glands |
|
|
Somatic vs Autonomic Presence of ganglia |
Somatic-no ganglia Autonomic- cell bodies of postganglionic autonomic fibers lovated in paravertebral (collateral), and terminal ganglia |
|
|
Somatic vs Autonomic Number of Neurons from CNS to effector |
Somatic- one (LMN) Autonomic- two |
|
|
Somatic vs Autonomic Type of neuromuscular junction |
Somatic-specialized motor end plate Autonomic- No specialization of postsynaptic membrane; all areas of smooth muscle cells contain receptor proteins for neurotransmitters |
|
|
Somatic vs Autonomic Effect of nerve impluse on muscle |
Somatic-Excitatory only Autonomic- Either excitatory or inhibitory |
|
|
Somatic vs Autonomic Type of nerve fibers |
Somatic-Fast-conducting, thick (9-13 nano meters), and myelinated Autonomic-Slow-conducting; preganglionic fibers lightly myelinated but thin (3 nano meters); postganglionic fibers unmyelinated and very thin ( about 1.0 nano meters) |
|
|
Somatic vs Autonomic Effect of denervation |
Somatic-Flaccid paralysis Autonomic- Muscle tone and function persist; target cells show denervation hypersensitivity |
|
|
Define Sympathetic Division |
part of the autonomic nervous system originating in the thoracic and lumbar regions of the spinal cord that in general inhibits or opposes the physiological effects of the parasympathetic nervous system, as intending to reduce digestive secretions, speeding up the heart, and contracting blood vessels sympathetic division of the autonomic system |
|
|
Where do pregnaglionic neurons come fromd |
the thoracic and lumbar regions of the spinal cord -also called the thoracolumbar division |
|
|
Preganglionic neurons synapse in sympathetic ganglia that run parallel to the spinal cord TRUE or FALSE |
TRUE |
|
|
When is sympathetic nervous system activated? |
-before exam -before workout -fighting becuase its excitatory |
|
|
Is digestion excitatory? |
No, its not related to the sympathetic nervous system |
|
|
Preganglionic comes from _________ |
brain |
|
|
sympathetic nervous system does what do the digestion track and to motility? |
it inhibits it |
|
|
Define Sympathetic chain of paravertebral Ganglia |
Along the length of the sympathetic trunk are ganglia known as ganglia of sympathetic trunk or paravertebral ganglia. The ganglia are distinguished as cervical, thoracic, lumbar, and sacral and, except in the neck, they closely correspond in number to the vertebrae. |
|
|
Define sympathetic trunk |
The sympathetic trunks (sympathetic chain, gangliated cord) are a paired bundle of nerve fibers that run from the base of the skull to the coccyx. |
|
|
Define Coccyx |
a small, triangular bone at the base of the spinal column in humans and some apes, formed of fused vestigial vertebrae |
|
|
Define Convergence and Divergence |
Divergence- one pregangnlionic neuron synapses on several postganglionic neurons at different levels
Convergence- several perganglionic neurons at different levels synapse on one postganglionc neuron |
|
|
What does the convergence and divergence allow the sympathetic division to do ? |
to act as a single unit through a mass activation and to be tonically active |
|
|
define tonically active |
tonic refers to a slow, continous action. When reference to tonically active neurons, it is regarded as continous firing/ dischargain at the synapse. |
|
|
Define Collateral ganglia |
sympathetic neurons that exit the spinal cord below the diaphragm do not synapse in the sympathetic chain of the ganglia.
-Instead they form splanchnic nerves which synapse in collateral ganglia. |
|
|
What does collateral ganglia include? |
-celiac, superior, mesenteric, and inferior mesenteric ganglia |
|
|
What do postganglionic neurons innervaate which organs? |
-digestive, urinary, and productive systems |
|
|
What does the adrenal medulla secrete? |
epinephrine and norepinephrine |
|
|
Where do preganglionic neurons come from? |
the brain and the sacral region of the spinal cord |
|
|
another word for brain or sacral region of the spinal cord? |
carniosacral division |
|
|
Define Terminal Ganglia |
a parasympathetic ganglion situated on or close to an innervated organ and being the site where preganglionic nerve fibers terminate |
|
|
Preganglionic Neurons travel with somatic neurons
TRUE or FALSE |
FALSE, preganlionic neurons do not travel with somatic neurons, sympathetic postganglionic neurons do. |
|
|
The occularmotor, facial, glosso-pharyngeal, and vagus nerves carry what kind of neurons? |
parasympathetic preganglionic nerves/neurons |
|
|
what do cranial neurons/nerves and parasympathetic division all carry? |
they all carry parasympathetic preganglionic nerves/neurons |
|
|
facial nerve, glossopharynegeal, and vagus nerve carry what kind of nerves? |
parasympathetic preganglionic nerves |
|
|
define glossopharyngeal |
-preganglionic fibers synapse on otic ganglion. -postganglionic fibers innervate salivary glands |
|
|
Define octic ganglion |
small, oval shaped, flattened parasympathetic ganglionof a reddish-gray color, located immediately below the foramen ovale in theinfratemporal fossa. It gives innervation to the parotid gland for salivation. |
|
|
Define Vagus Nerve |
Preganglionic fibers exit medulla, branch into several pexi and nerves, and travel to ganglia within effector organs |
|
|
name the effector organs |
-heart -lungs -esophagus -stomach -pancreas -liver -intestines |
|
|
define plexi nerves |
is a branching network of vessels or nerves. |
|
|
parasympathetic fibers in vagus nerve start from and innervate where |
preganglionic fibers exit medulla, branch into plexi and nerves, travel to ganglia within effector organs (heart, lungs, esophagus, stomach, pancreas, liver, intestines) |
|
|
preganglionic nerves form the sacral region of the spinal cord provide innervation to where? |
the lower part of the large intestine, rectum, urinary and reporductive organs |
|
|
Origin of Preganglionic FIbers and Effector Organs
Oculomotor (third cranial) nerve |
-Midbrain (cranial) -Eye (smooth muscle in iris and ciliary body) |
|
|
Origin of Preganglionic FIbers and Effector Organs
Facial (7th cranial) |
-Pons (cranial) -Lacrimal, mucous, and salivary glands
|
|
|
Origin of Preganglionic FIbers and Effector Organs
Glossopharyngeal (9th cranial) |
-Medulla Oblangata (cranial) -Parotid gland
|
|
|
Origin of Preganglionic FIbers and Effector Organs
Vagus Nerve |
-Medulla Oblangata ( cranial) -Heart, lungs, gastrointestinal tract, liver, pancreas
|
|
|
Origin of Preganglionic FIbers and Effector Organs
Pelvic spinal nerves |
-S2 to S4 (sacral) -Lower half of large intestine, rectum, urniary bladder, and reproductive organs
|
|
|
define sympathectomy |
s an irreversible procedure during which at least onesympathetic ganglion is removed. |
|
|
What are the 2 major divisions of the autnonomic nervous system? |
-sympathetic functions -parasympathetic functions
|
|
|
which is the neurotransmitter involoved in preganglionic neurons |
ach and ne acetycholine and norephinphrine
|
|
|
the sympathetic divisions activates the body for which action throught the release of norepinephrine from postganglionic neurons and the secretion of epinephrine from the adrenal medulla |
-fight or flight |
|
|
sympathetic and preganglionic have what length and what neurotransmitter |
short/ach
|
|
|
parasympathetic and preganglionic have what length and what neurotransmitter? |
long/ach
|
|
|
sympathetic and postganglionic have what length and what neurotransmitter? |
long /NE |
|
|
parasympathetic and postganglionic have what length and what neurotransmitter? |
short/ach |
|
|
what is the site of origin for the sympathetic in the autonomic nervous system? |
center of spinal cord T1-L5 |
|
|
what is the site of origin for the parasympathetic in the autonomic nervous system? |
Gray matter of cranium |
|
|
define cholionergic synaptic transmission steps |
1. action potential comes to axon terminal 2. voltage gated CA- channels open 3. Triggers ACh Release 4. empty vesicles will refill while reserve moves to active site 5. Ach bind to ligand-gated channels 6. Na produces post synaptic potential |
|
|
ACh is the neurotransmitter used by all preganglionic neurons (symp and para)
TRUE or FALSE |
TRUE |
|
|
Adrenergic Synaptic Transmission Steps |
1. (NE) receptor bounded to G protein 2. NE binding releases G protein 3. G protein binds to adenylate cyclase (converts ATP to cAMP) 4. cAMP causes multiple possible effects 5. opens ligand gated channels 6. activates enzymes 7. genetic transcription (copying of DNA to RNA)
|
|
|
Define varicosities |
-axons of postganglionic nerves that have various swellings - |
|
|
name of receptors of parasympathetic nervous system |
muscarinic receptors |
|
|
define muscarinic receptors (agonist) |
an agent that activates the activity of the muscarinic acetylcholine receptor |
|
|
define agonist |
the prime mover, the muscle doing the movement -drugs that promote the process stimulated by the NT (neurotransmitter) |
|
|
define antagonist |
the muscle resisting movement -durgs that block the action of the NT (neurotransmitter) |
|
|
parasympathetic |
decrease heart rate |
|
|
lets say you get a subtance that is an agonist of muscarinic receptors, what effect will if have on humans, more specifically on your heart? |
1. decreased heart rate, becuase its in the parasympathetic ANS (rest and digest) |
|
|
where do you find muscarinic receptors |
in the parasympathetic autonomic nervous system |
|
|
response to adrenergic stimulation, can be epinephrine in the blood or ___ from the sympathetic nerves |
norepinephrine |
|
|
Response to adrenergic stimulation
can_________ or ________, depnding on the receptors |
-stimulate -inhibit
|
|
|
What does adrenergic stimulate in the body? |
heart, dilatory muscles of the iris, smooth muscle of many blood vessels (causes vessel constriction) |
|
|
What does adrenergic inhibit in the boyd? |
in lungs, other blood vessels; inhibits contraction and casues dilation of theses structures |
|
|
How many Adrenergic receptors are there? and what are they? |
two types of alpha= alpha 1 and alpha 2
two types of beta= beta 1 and beta 2
|
|
|
what neurotransmitters are the beta more succeptible to ? |
epinephrine
|
|
|
what neurotransmitters are alpha more succesptible to ? |
norepinephrine |
|
|
what do all alpha and beta adrenergic receptors act on? |
g-proteins and second messanger systems |
|
|
beta recptors use______ |
cAMP (Cyclic adenosine monophosphate) |
|
|
Alpha receptors use_______ |
Ca+ second messenger system |
|
|
What is the Adrenergic effects in the EYE? how does it effect the Sympathoadrenal System, and which Adrenergic Receptor is used? |
-Contraction of radial fibers of the iris dialtes the pupils, and alpha 1
|
|
|
What is the Adrenergic effects in the heart? how does it effect the Sympathoadrenal System, and which Adrenergic Receptor is used?
|
-increase in heart rate and contraction strength, and beta 1 primarily |
|
|
What is the Adrenergic effects in the Skin and visceral vessels? how does it effect the Sympathoadrenal System, and which Adrenergic Receptor is used?
|
-Arterioles constrict due to sympathetic nerve activity, and alpha 1 |
|
|
What is the Adrenergic effects in the lungs? how does it effect the Sympathoadrenal System, and which Adrenergic Receptor is used?
|
-Bronchioles (airways) dilate due to smooth muscle relaxation and beta 2 |
|
|
What is the Adrenergic effects in the stomach and intestine? how does it effect the Sympathoadrenal System, and which Adrenergic Receptor is used?
|
-contraction of sphincters slows pasage of food and alpha 1 |
|
|
What is the Adrenergic effects in the liver? how does it effect the Sympathoadrenal System, and which Adrenergic Receptor is used?
|
-Glycogenolysis and secretion of glucose and alpha 1 and beta 2 |
|
|
if given beta 2 blockers to your what will happen? |
cause smooth muscle relaxation, resulting in dilation of bronchial passages, vasodilation in muscle and liver, relaxation of uterine muscle, and release of insulin. |
|
|
where are alpha 2 receptors located? |
on presynaptic axons |
|
|
what happens when alpha 2 receptors are stimulated |
they result in inhibition of norepinephrine release in the synapse
|
|
|
What happens in response to cholinergic stimulation in preganglionic and postganglionic neurons? |
-ACh relased from preganglionic neurons of both the sympathetic and parasympathetic division is stimulatory -ACh from postganglionic neurons of the parasympathetic division is usually stimulatory, but some are inhibititory, depending on receptors -in general, sympathetic and paraysmpathetic effects are opposite |
|
|
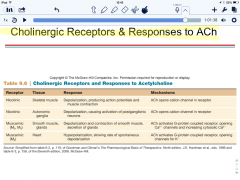
NAme two main Cholinergic Receptors |
Nicotinic and Musacrinic |
|
|
Where is nicotininc receptors found? |
in autonomic ganglia |
|
|
How are nicotinic receptors stimulated |
stimulated by ACh from preganglionic neurons |
|
|
Where is muscarinic found and how is it stimulated? |
in visceral organs and stimulated by release of ACh form postganglionic neurons |
|
|
what blocks nicotinic? |
curare |
|
|
what blocks muscarinic? |
atropine |
|
|
learn |
|
|
Nitric Oxide is very important for the erection of the penis
TRUE or FALSE |
TRUE |
|
|
NO can also produce smooth muscle relaxation in where? |
-the stomach, intestines, urinary blaffer, and brain |
|
|
Most visceral organs are innervated by only the sympathetic neurons
TRUE OR FALSE |
FALSE, most visceral organs are innervated by both sympatheric and parasympathetic neurons |
|
|
what do symp and parasymp do to the ; heart rate, digestive functions, and pupil diameter |
heart rate -symp=increases -parasymp=decreases
Digestive functions -symp=decreases -parasymp=increases
Pupil Diameter -symp=dialtes -para=constricts
|
|
|
What complementary effects occur when both divisions produce simliar effects on the same target |
-salivary gland secretion: parasymp division stimulates secretion of watery saliva,symp constricts blood vessels so the secretion is thicker |
|
|
What cooperative effects occur when both divisions produce different effect that work together to promote a single action? |
-Erection and ejaculation: parasymp division causes vasodialation and erction; symp causes ejaculation -Urination: parasymp division aids in urinary blaffer contraction; smyp helps with baldder muscle tone to control urination |
|
|
Organs without dual innervation (sympathetic only) |
-adrenal medulla -arrector pili muscles in skin -sweat glands in skin -most blood vessels
|
|
|
the ANS is controlled by higher brain centers
TRUE or FALSE |
TRUE, many visceral functions are regulated by autonomic reflexes |
|
|
how does the ANS and higher brain centers work together |
sensory input is send to brain centers (usually by the vagus nerve), which intergrate the information and modify the activity of preganglioinc neurons. |
|
|
what functions does the medulla oblangata control? |
cardio, pulmonary, urinary, reproductive, and digestive |
|
|
Which higher brain regions regulate the medulla |
hypothalamus, limbic system, cerebellum, frontal and temporal lobes |
|
|
what is the function of the hypothalamus? |
major regulatory center of the ANS-body temp, hunger, thirst, pituitary gland
|
|
|
what is the function of limbic system |
responsible for autonomic responses during emotional states (blushing, pallor, fainting, cold sweating, raceing heart)
|
|
|
what is the function of the cerebellum? |
motion sickness nausea, sweating, cardio changes
|
|
|
what is the function of the frontal and temporal lobes? |
emotion and personality |
|
|
when you age there is decreased levels of sympathetic tone and there fore decreased levels of hypertension and cardio disease
TRUE or FALSE |
FALSE, when you age there is increased sympathetic tone and increased risk in hypertnesion and cardio disease |

