![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back
|
Calcium phosphate |
2/3 of the weight of the bone |
|
|
Osteocytes |
Mature bone cells, maintain and monitor the protein and mineral content |
|
|
Osteoblasts |
Cuboidal, single layer on the inner or outer surfaces of a bone, responsible for the production of new bone osteogenesis. Always producing matrix that quickly binds minerals. |
|
|
Osteo progenitor cells |
Flattened or squamous shaped stem cells found in numerous areas including inner most layer of the periosteum and in the Endosteum lining the medullary cavities can divide to produce daughter cells that differentiate into osteoblasts |
|
|
Osteoclast |
Large multi nucleate cells found at sites where bone is being removed erosion process where acids produced involving the exocytosis of lysosomes dissolve the bony matrix and release amino acids and the stored calcium and phosphate equals osteolysis. Always removing matrix and releasing minerals. |
|
|
Osteolysis |
Increases the calcium and phosphate concentrations in body fluids |
|
|
Compact bone |
Relatively dense and solid. Also known as the cylindrical osteon or haversion system. Forms walls. |
|
|
Spongy bone |
Forms an open network of struts and plates |
|
|
What's the difference between spongy bone and compact bone? |
The arrangement of spongy bone into parallel struts or sick branching plates called trabeculae and much lighter than compact bone. Spongy bone is found wherever bones aren't stressed heavily or where stresses arrive from many directions. |
|
|
What is the outer surface of a bone covered in? |
Periosteum. it isolates and protects the bone from surrounding tissues |
|
|
Ossification |
The process of replacing other tissues with bone |
|
|
Calcification |
The deposition of calcium salts within a tissue. |
|
|
Ossification versus calcification |
Any tissue can be calcified but only ossification results in the formation of bone |
|
|
Intramembranous ossification |
Bone develops to form mesenchymal or fibrous connective tissue. For example clavicle, mandible, flat bones of the face and skull |
|
|
Endochondral ossification |
Bone replaces existing Cartlidge model. For example, bones that bear weight such as the vertebral column |
|
|
Joints and articulations |
Connections between bones that may or may not permit movement |
|
|
Synarthrosis |
Immovable: suture- fibrous, gomphosis- teeth-fibrous, synchondrosis-ribs-sternum- cartilaginous, synostosis-head-bony fusion |
|
|
Amiphiarthrosis |
Little movement. Syndesmosis – tibia and Fibula connection – fibers, symphysis – pubic – cartilaginous |
|
|
Diarthrosis |
Free movement. Synovial – ends of long bones. Monaxial – one plane – elbows or ankle. Biaxial – two planes – ribs, wrist. Triaxial – three planes – shoulder and hip. |
|
|
Synovial joints |
Joint capsule, articular Cartlidge, joint cavity filled with synovial fluid, synovial membrane lining capsule, accessory structure, sensory nerves and blood vessels. Function – lubrication, nourishes chondrocytes, shock absorption for joints. |
|
|
Accessory structures such as |
Cartilages, menisci divided synovial cavity. Fat pads – periphery of joint, lightly covered by a layer of synovial membrane. |
|
|
Ligaments |
Support, strengthen and reinforce synovial joints. |
|
|
Intrinsic ligaments versus extrinsic ligaments |
Intrinsic – beginnings of the joint capsule. Extrinsic – separate from the joint capsule |
|
|
Gliding joint |
Monaxial, sternoclavicular joint or intercarpal and tarsal joints |
|
|
Pivot |
Monaxial, Head on atlas and axis |
|
|
Gliding joint |
Monaxial, sternoclavicular joint or intercarpal and tarsal joints |
|
|
Saddle |
Biaxial. First metacarpal joint |
|
|
Intrinsic ligaments versus extrinsic ligaments |
Intrinsic – beginnings of the joint capsule. Extrinsic – separate from the joint capsule |
|
|
Gliding joint |
Monaxial, sternoclavicular joint or intercarpal and tarsal joints |
|
|
Pivot |
Monaxial, Head on atlas and axis |
|
|
Saddle |
Biaxial. First metacarpal joint |
|
|
Hingr |
Monaxial. Elbow, knee, ankle |
|
|
Ligaments |
Support, strengthen and reinforce synovial joints. |
|
|
Intrinsic ligaments versus extrinsic ligaments |
Intrinsic – beginnings of the joint capsule. Extrinsic – separate from the joint capsule |
|
|
Gliding joint |
Monaxial, sternoclavicular joint or intercarpal and tarsal joints |
|
|
Pivot |
Monaxial, Head on atlas and axis |
|
|
Saddle |
Biaxial. First metacarpal joint |
|
|
Hingr |
Monaxial. Elbow, knee, ankle |
|
|
Ellipsoidal |
Biaxial. Radiocarpal joint |
|
|
Ligaments |
Support, strengthen and reinforce synovial joints. |
|
|
Intrinsic ligaments versus extrinsic ligaments |
Intrinsic – beginnings of the joint capsule. Extrinsic – separate from the joint capsule |
|
|
Gliding joint |
Monaxial, sternoclavicular joint or intercarpal and tarsal joints |
|
|
Pivot |
Monaxial, Head on atlas and axis |
|
|
Saddle |
Biaxial. First metacarpal joint |
|
|
Hingr |
Monaxial. Elbow, knee, ankle |
|
|
Ellipsoidal |
Biaxial. Radiocarpal joint |
|
|
Ball and socket |
Triaxial. Shoulder, hip joint |
|
|
Ligaments |
Support, strengthen and reinforce synovial joints. |
|
|
Intrinsic ligaments versus extrinsic ligaments |
Intrinsic – beginnings of the joint capsule. Extrinsic – separate from the joint capsule |
|
|
Gliding joint |
Monaxial, sternoclavicular joint or intercarpal and tarsal joints |
|
|
Pivot |
Monaxial, Head on atlas and axis |
|
|
Saddle |
Biaxial. First metacarpal joint |
|
|
Hinge |
Monaxial. Elbow, knee, ankle |
|
|
Ellipsoidal |
Biaxial. Radiocarpal joint |
|
|
Ball and socket |
Triaxial. Shoulder, hip joint |
|
|
Condylar |
Wrist or fingers |
|
|
Excitability |
Ability to respond to stimulation |
|
|
Excitability |
Ability to respond to stimulation |
|
|
Contractility |
Ability to shorten actively and exerts a pull or tension that can be harnessed by connected tissue |
|
|
Excitability |
Ability to respond to stimulation |
|
|
Contractility |
Ability to shorten actively and exerts a pull or tension that can be harnessed by connected tissue |
|
|
Extensibility |
Ability to continue to contract over a range of resting lengths |
|
|
Excitability |
Ability to respond to stimulation |
|
|
Contractility |
Ability to shorten actively and exerts a pull or tension that can be harnessed by connected tissue |
|
|
Extensibility |
Ability to continue to contract over a range of resting lengths |
|
|
Elasticity |
Ability to rebound toward its original length after a contraction |
|
|
Excitability |
Ability to respond to stimulation |
|
|
Contractility |
Ability to shorten actively and exerts a pull or tension that can be harnessed by connected tissue |
|
|
Extensibility |
Ability to continue to contract over a range of resting lengths |
|
|
Elasticity |
Ability to rebound toward its original length after a contraction |
|
|
Somatic |
Skeletal |
|
|
Excitability |
Ability to respond to stimulation |
|
|
Contractility |
Ability to shorten actively and exerts a pull or tension that can be harnessed by connected tissue |
|
|
Extensibility |
Ability to continue to contract over a range of resting lengths |
|
|
Elasticity |
Ability to rebound toward its original length after a contraction |
|
|
Somatic |
Skeletal |
|
|
Autonomic |
Cardiac and smooth |
|
|
Muscle fiber |
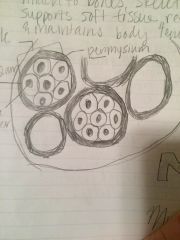
Back (Definition) |
|
|
Endomysium |
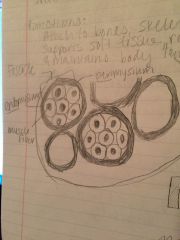
Back (Definition) |
|
|
Fascicles |
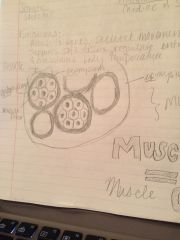
Back (Definition) |
|
|
Perimysium |

Back (Definition) |
|
|
Epimysium |
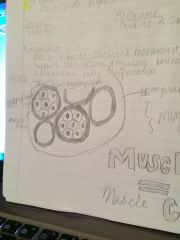
Back (Definition) |
|
|
Myofibrils |
Cylindrical structure allowing muscle contraction |
|
|
Sarco- |
Flesh |
|
|
Actin |
Thin filaments, troponin blocks active sites |
|
|
Myofibrils |
Cylindrical structure allowing muscle contraction |
|
|
Sarco- |
Flesh |
|
|
Actin |
Thin filaments, troponin blocks active sites |
|
|
Myosin |
Thick filaments |
|
|
Sarcolemma |
Cell membrane |
|
|
Cytoplasm |
Sarcoplasm |
|
|
Internal membrane system |
Sarcoplasmic reticulum |
|
|
Myoblasts |
Groups of embryonic cells combined to create individual skeletal muscle fibers |
|
|
Muscle fiber contraction sequence of events |
Chemicals released by motor neuron at synapse alters the transmembrane potential of sarcolemma. Transverse tubules. The change in the transmembrane potential of the t-tubules triggers the release of calcium ions by the sarcoplasmic reticulum which equals a contraction. |
|
|
Muscle fiber contraction sequence of events |
Chemicals released by motor neuron at synapse alters the transmembrane potential of sarcolemma. Transverse tubules. The change in the transmembrane potential of the t-tubules triggers the release of calcium ions by the sarcoplasmic reticulum which equals a contraction. |
|
|
Acetylcholine |
Expanded tip of the axon at neuromuscular synapse – synaptic terminal – synaptic vesicles with acetylcholine equals neurotransmitter |
|
|
Muscle fiber contraction sequence of events |
Chemicals released by motor neuron at synapse alters the transmembrane potential of sarcolemma. Transverse tubules. The change in the transmembrane potential of the t-tubules triggers the release of calcium ions by the sarcoplasmic reticulum which equals a contraction. |
|
|
Acetylcholine |
Expanded tip of the axon at neuromuscular synapse – synaptic terminal – synaptic vesicles with acetylcholine equals neurotransmitter |
|
|
A narrow space |
Equals synaptic cleft separates synaptic terminal from motor end plate of skeletal muscle fiber |
|
|
Muscle fiber contraction sequence of events |
Chemicals released by motor neuron at synapse alters the transmembrane potential of sarcolemma. Transverse tubules. The change in the transmembrane potential of the t-tubules triggers the release of calcium ions by the sarcoplasmic reticulum which equals a contraction. |
|
|
Circular skeletal muscle fibers |
Sphincter. Example – mouth or eyes |
|
|
Prime mover |
Agonist. A muscle who's contraction is chiefly responsible for producing a particular movement |
|
|
Antagonist |
Muscles his actions oppose that of the agonist. If agonist produced flexion antagonist will produce extension |
|
|
Synergist |
Assists prime mover |
|
|
Acetylcholine |
Expanded tip of the axon at neuromuscular synapse – synaptic terminal – synaptic vesicles with acetylcholine equals neurotransmitter |
|
|
A narrow space |
Equals synaptic cleft separates synaptic terminal from motor end plate of skeletal muscle fiber |
|
|
Synaptic cleft |
Contains acetylcholine esterase which breaks down acetylcholine |
|
|
Type one muscle fiber |
Slow fibers or red fibers. Three times longer to contract. Aerobic metabolism. Specialized to continue contracting for extended periods of time because mitochondria continue producing ATP. Also known as slow twitch. |
|
|
Type two muscle fiber |
Fast fibers, white fibers. Large densely packed myofibrils, large glycogen reserves, few mitochondria, powerful contractions using a lot of ATP and mitochondria can't keep up so they fatigue rapidly. Supported primarily of anaerobic glycolysis – glycogen – lactic acid – fermentation |
|
|
Intermediate muscle fibers |
Pink. right in between fast and slow fibers |
|
|
Parallel skeletal muscle fibers |
Along longitudinal axis. Example – biceps brachii |
|
|
Convergent skeletal muscle fibers |
Common attachment site. Example – pectoral muscles |
|
|
Pinnate skeletal muscle fibers |
Feather like. For example rectus femoris, deltoid muscle |

