![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
|
Describe the female breast, its innervation, blood supply and lymphatic drainage.
|
It consists of mammary glands (modified sweat glands), which consist of ducts and secretory lobules that converge to form lactiferous ducts that open independently onto the nipple.
---The nipple is surrounded by circular pigmented area called areola. Well-developed connective tissue stroma surrounds the ducts/lobules and condenses to form the suspensory ligaments of the breast (continuous with dermis) which support the breast. In non-lactating women, the predominant component is fat, whereas glandular tissue is abundant in lactating women. A layer of loose connective tissue (retromammary space) separates the breast from deep fascia/pectoralis major and allows for some movement over underlying structures. Innervation: Anterior and lateral cutaneous branches of 2nd to 6th intercostal nerves; nipple is innervated by the 4th intercostal nerve. Blood supply: ---Arteries: laterally, vessels from axillary artery (superior thoracic, thoracoacromial, lateral thoracic, subscapular); medially, branches from internal thoracic artery; 2nd-4th intercostal arteries ---Veins: veins parallel arteries and drain into axillary, internal thoracic and intercostal veins. Lymph: Axillary lymph node group (humeral, central subscapular, lateral pectoral and apical) receive 75% of drainage ---lateral pectoral nodes are primary nodes for lymphatic drainage Parasternal lymph nodes drain the remaining 25%. |
|
|
Describe the organization of ribs and sternum.
|
There are 12 ribs that attach to the 12 thoracic vertebrae posteriorly and terminate anteriorly in costal (hyaline) cartilage.
---7 True Ribs: upper seven articulate directly with the sternum through their costal cartilage ---5 False Ribs: ribs 8-10 articulate with costal cartilage which then attaches to sternum ------11 & 12 are floating ribs (don't attach to sternum at all) Sternum made of three parts: ---Manubrium: top portion ---Body: larger middle portion ---Xiphoid process: smallest portion, tip on the end |
|
|
What is the articulation between the manubrium and the body of the sternum called? Why is it important?
|
Sternal angle: creates a plane that separates the superior and inferior mediastinum and marks that superior border of the pericardium; it also separates the end of the ascending aorta from the beginning of the aortic arch and the end of the arch from the beginning of the thoracic aorta; also marks the bifurcation of the trachea into the primary bronchii.
|
|
|
What are the three intercostal muscles, their innervation and function and how are the related to one another?
|
External intercostals: most active during inspiration, moves ribs superiorly; supports intercostal space
---Innervation: intercostal nerves T1-T11 Internal intercostals: most active during expiration, moves ribs inferiorly; supports intercostal space ---Innervation: intercostal nerves T1-T11 Innermost intercostals: acts with internal intercostals ---Innervation: intercostal nerves T1-T11 ---External intercostals are outermost, attaching around the vertebral column and ending at the costal cartilage ---Internal intercostals are the middle layer, attaching around the sternum and ending before the vertebral column ---Innermost intercostals are the inner layer, attaching along the sides at neither the sternum nor the vertebral column. |
|
|
What is the origin and course of intercostal nerves, arteries and veins?
|
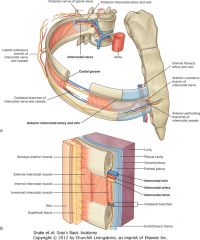
Nerves:
---originate from anterior rami of T1-T11 (T12 lies below rib 12) ---travel between innermost and internal intercostals and forms lateral/anterior cutaneous branches innervate skin; has somatic motor/sensory as well as postganglionic sympathetic fibers Arteries: ---originate from aorta and internal thoracic arteries, pass between the innermost and internal intercostal muscles ---supply thoracic wall and superficial regions; internal thoracic artery eventually splits into superior epigastric (into abdominal wall) and musculophrenic (diaphragm) Veins: ---parallels arteries; intercostal veins drain into azygos system (rigth superior intercostals empty into) or internal thoracic veins which become the brachiocephalic veins (left superior intercostals empty into) ------All form small collateral branches that run along the upper margin of the ribs; arteries anastomose posterior and anterior |
|
|
How should an intercostal nerve block or thoracocentesis be correctly performed?
|
The needle must be inserted in the middle between the ribs, not along the top or bottom of the rib in order to avoid the nerves/arteries/veins that run along the top/bottom of the ribs
---between ribs 7-9 |
|
|
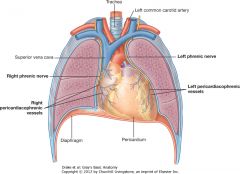
Describe the diaphragm, its innervations, blood supply and structures that pass through it.
|
It is a thin, musculotendinous structure that separates the thoracic cavity from the abdominal cavity; its muscles fibers converge to form a central tendon
---essential for normal breathing, especially resting breaths (contraction flattens and increases thoracic volume) ---Innervation: phrenic nerves (C3-5) Arteries: ---pericardiocophrenic and musculophrenic arteries (from internal thoracic arteries) ---superior/inferior phrenic (from thoracic/abdominal aorta, respectively) Veins: ---veins parallel arteries; drain into brachiocephalic veins (neck), azygos system of veins, or abdominal veins (inferior vena cava/left suprarenal vein) Passing through: ---inferior vena cava (through central tendon at T8) ---esophagus (through muscle at T10) ---Vagus nerve (with esophagus) ---Aorta (behind posterior attachment at T12) ---Thoracic duct (with aorta) ---Azygos/hemiazygos veins (through aortic hiatus) |
|
|
Describe movements of thoracic wall and diaphragm. How does this alter the intrathoracic pressure?
|
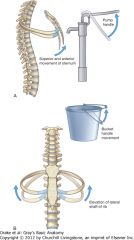
Dimensions change in vertical, lateral and anteroposterior directions:
---elevation/depression of diaphragm alter vertical (depression=contraction/elevation=relaxation) ---elevation/depression of ribs alter anteroposterior/lateral ------sternum moves up/forward when ribs elevate (anteroposterior) ------middle of rib move up/out when ribs elevate (lateral) Pressure: parietal/visceral pleura adhere to one another and parietal pleura attaches to thoracic wall/diaphragm/mediastinal structures so: thoracic wall/diaphragm moves > parietal pleura moves > visceral pleura moves > lungs move and as thoracic cavity expands, so do lungs, which decreases their internal pressure, allowing air to rush in |
|
|
Describe the pleural cavities; what is the difference between parietal and visceral pleura?
|
There are two (either side of mediastinum):
---extend above rib 1, to just above costal margin, with the mediastinum making up the medial walls ---Cavity is lined by single layer of flat cells, mesothelium and layer of supporting connective tissue Parietal pleura: lines walls of pleural cavity Visceral pleura: covers the lungs |
|
|
What are the boundaries of the pleural cavity at the midclavicular and midaxillary lines?
|
Midclavicular line:
---pleural cavity: extends inferiorly to approximately rib 8 ---lungs: (quiet respiration) inferior margin crosses rib 6 Midaxillary line: ---pleural cavity: extends to rib 10 ---lungs: (quiet respiration) inferior margin crosses rib 8 |
|
|
What are the two major pleural recesses in the thorax?
|
Costomediastinal recesses:
---anteriorly, occur where costal pleura is opposed to mediastinal pleura (largest on left) Costodiaphramatic recesses: ---largest and most clinically important ------between inferior margin of lung and inferior margin of pleural cavity (deepest after forced expiration/shallowest after forced inspiration) |
|
|
What is sensory innervation of parietal pleura? Visceral pleura?
|
Parietal pleura:
---somatic afferent fibers; from either intercostal nerves of phrenic nerves (pain referred to thoracic wall or C3-5 dermatomes of lateral neck/shoulder) Visceral pleura: ---visceral afferent fibers; no pain sensors |
|
|
Describe the organization of the lungs.
|
Lungs: half-cone shaped, right (three lobes) slightly larger because heart bulges into left (two lobes)
---Root: short tubular collection of structures connects lung to mediastinum (contains: 1 pulmonary artery, two pulmonary veins, main bronchus, bronchial vessels, nerves, lymphatics) ---Hilum: outlined by pleura, where structures enter/leave ---Pulmonary ligament: folded projection of pleura below root extends from hilum to mediastinum stabilizes lung/allow movement of structures in root during breathing |
|
|
Describe the organization of the bronchial tree.
|
Trachea: flexible tube, extends from C7 to T4/5 where is bifurcates into the right and left main bronchus
---held open by C-shaped cartilage rings (opening face posterior), with posterior wall composed of smooth muscle Main bronchus: enters root of lung and passes through hilum into lung then divides into lobar (secondary) bronchi, which supply each lobe ---in right lung, superior lobar bronchi originates in root of lung Lobar bronchi divide into segmental (tertiary) bronchi which supply bronchopulmonary segments Segmental bronchi then give rise to further divisions and eventually bronchioles, which further subdivide and supply respiratory surfaces ---bronchi are held open by discontinuous plates of cartilage ---bronchioles don't have cartilage |
|
|
What are bronchopulmonary segments?
|
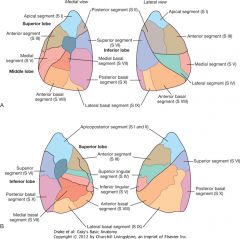
They are areas of the lung supplies by segmental bronchus and accompanying pulmonary artery branch
---smallest functionally independent region of a lung and smallest area that can be isolated and removed without affecting adjacent regions ---there are 10 in each lung (some fuse in left lung |
|
|
Where do adults usually aspirate materials?
|
Right main bronchus is wider and more vertical, so inhaled foreign bodies tend to lodge on the right more than left
|
|
|
How is blood supplied to the lungs?
|
Arteries:
---Right and left pulmonary arteries carry deoxygenated blood from lungs to heart ------originate from pulmonary trunk (bifurcation at T4/5, anteroinferior to trachea) ------Right: longer than left, enters root and gives off large branch into superior lobe, main vessel continues through hilum, gives off second (recurrent) branch to superior lobe and divides to supply middle/inferior lobes ------Left: shorter, passes through root and hilum, then branches ---bronchial arteries: originate from thoracic aorta, supply pulmonary tissue and interconnect with pulmonary arteries in lung Veins: ---each side has superior and inferior pulmonary veins which carry oxygenated blood from heart to lungs (begin at hilum, drain into left atrium ---bronchial veins: drain into pulmonary veins or left atrium and into azygos vein (right) or superior intercostal vein/hemiazygos vein (left) |
|
|
How are the lungs innervated?
|
Innervation: supplied by visceral afferents/efferents through the anterior/posterior pulmonary plexuses
---plexuses lie anterior/posterior to tracheal bifuraction (anterior smaller); originate from sympathetic trunk and vagus nerves ------vagus nerves constrict bronchioles ------sympathetic system dilates bronchioles |
|
|
What is the mediastinum?
|
It is a broad central partition that separates the two laterally placed pleural cavities.
Contains: ---heart inside pericardial sac ---trachea ---esophagus ---great vessels ---nerves (phrenic/vagus) ---azygos vein system ---sympathetic chain/splanchnic nerves ---thoracic duct |
|
|
What defines the middle mediastinum, what are its contents and how do they physically relate to one another?
|
It is centrally located in the thoracic cavity and it contains the pericardium (fibrous outer layer defines boundaries), heart, origins of great vessels, nerves and smaller vessels
|
|
|
Describe the pericardium, its innervation and blood supply.
|
It is composed of two layers, which are continuous with great vessels:
---fibrous pericardium: tough connective tissue outer layer; attaches to central tendon of diaphragm and sternopericardial ligament to stabilize heart in its position ---serous pericardium: thin and consists of two layers ------parietal layer: lines inner surface of fibrous pericardium ------visceral layer (epicardium): adheres to heart, forming outer covering ---pericardial space between parietal/visceral layer has fluid to allow for uninhibited movement Innervation: phrenic nerves (pass through fibrous pericardium), vagus nerve, sympathetic trunks Arteries: internal thoracic, pericardiacophrenic, musculophrenic and inferior phrenic arteries and thoracic aorta Veins: enter azygos system, internal thoracic and superior phrenic veins |
|
|
Why is pain from pericarditis referred to the shoulder region?
|
The phrenic nerves carry the somatic afferent fibers for the pericardium and the dermatomes (C3-C5) relate to the shoulder region, so pain is referred to that area
|
|
|
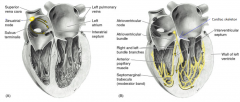
Describe the orientation of the individual chambers of the heart in situ.
|
Base (posterior surface): left atrium, portion of the right atrium, and proximal parts of the great veins (SVA/IVC and pulmonary veins)
---the esophagus is immediately posterior Anterior surface: mostly right ventricle with some right atrium and some left ventricle Diaphragmatic surface (side heart rests on): left ventricle and small portion of right ventricle Left pulmonary surface: faces left lung, with left ventricle and portion of left atrium Right pulmonary surface: faces right lung, with right atrium |
|
|
Describe the structure of the heart.
|
It consists of two pumps separated by a partition
---right pump (atrium/ventricle) receives deoxygenated blood from body and sends it to lungs ---left pump (atrium/ventricle) receive oxygenated blood from lungs and send it to body Each atrium and ventricle are separated by a valve ---atria are thin-walled chambers that receive incoming blood ---ventricles have thicker walls because they pump blood out ------more force is need to pump blood to body than to lungs, so Left ventricle is more muscular/thicker than right The chambers are each separated by interartial, interventricular and atrioventricular septa |
|
|
Describe the components of the right atrium.
|
Blood is delivered to the atrium via:
---superior or inferior vena cava (from the body) ---coronary sinus (from the heart's circulation) Blood passes from atrium to ventricle via a tricuspid valve ---crista terminalis: connects between vena cavae and is a smooth muscular ridege on roof of atrium ---sinus venarum: is posterior to crista and has smooth thin walls where vena cavae empty into ---pectinate muscles: are in both atrium and auricle and fan out from crista ---interartial septum: separates right from left atrium ---fossa ovalis: depression in the septum, marks location of foramen ovale |
|
|
Describe the components of the right ventricle.
|
---conus arteriosus: smooth walled area where blood exits via pulmonary trunk
---trabeculae carnae: muscular irregular structures from ridges by attaching to the walls ------papillary muscles: trabeculae that only attach to wall at one end, with other end serving at point of attachment for tendon-like cords ------there are 3 (anterior, posterior, and septal) ---chordae tendinae: tendon-like cords that connect to the free edge cusps of the tricuspid valve ---septomarginal trabecula (moderator band): forms bridge from anterior papillary muscle to the interventricular septum Tricuspid valve: has three cusps (anterior, posterior, septal) ---papillary muscles and chordae tendinae keep cusps from everting into atrium Semilunar pulmonary valves: right, left and anterior; outflow from ventricles pushes them open, then recoil of blood fills them cusps and forces them closed (prevents trunk from refilling ventricle |
|
|
Describe the components of the left atrium.
|
Blood enters the atrium via the four pulmonary veins (smooth walls near their entrance)
---contains pectinate muscles, but nothing distinctly separates the smooth from the muscular ridges ---the interartial septum on this side has the depression of the valve of the foramen ovale (from fetal development) |
|
|
Describe the components of the left ventricle.
|
Blood exits via the aorta through the aortic vestibule, which has smooth walls
---walls are thicker, more muscular ---trabeculae carnae: thin and delicate compared to right ---has two papillary muscles/chorae tendinae for the bicuspid/mitral valve; tend to be larger (anterior/posterior) ---interventricular septum: forms right wall, has two parts: ------muscular: thick, forms major part of septum ------membranous: thin, forms upper part Mitral valve: two cusps (anterior/posterior), function papillary muscles/chordae tendinae keep the cusps from everting under pressure into atrium Semilunar aortic valves: right, left and posterior; right and left cover the openings for the right and left coronary arteries during outflow of blood; recoil fills the cusps and forces blood into the coronary arteries. |
|
|
What is the cardiac skeleton and what is its function?
|
It consists of dense, fibrous connective tissue that forms four rings (anulus fibrosus) around the atrioventricular orifices, the aortic vestibule and the pulmonary opening
---maintains integrity of openings and provides point of attachment for cusps; separates atrial/ventricular musculature; electrically isolates atria from ventricle so AV bundle is the only connection between the two |
|
|
What are the two types of valve disease and what are some specific issues?
|
Incompetence: poorly functioning valves
Stenosis: narrowing of orifice, caused by valve's inability to open fully ---mitral valve disease: mix of stenosis/incompetence; leads to left ventricular hypertrophy, increased pulmonary venous pressure, pulmonary edema and enlargement/hypertrophy of left atrium ---aortic valve disease: both stenosis/regurgitation (backflow) can produce heart failure ---valve disease in right (tricuspid or pulmonary): caused by infection; produces abnormal pressure changes in either atrium or ventricle and can induce cardiac failure |
|
|
Describe where a stethoscope should be placed to listen for heart sounds and what are the specific valves?
|
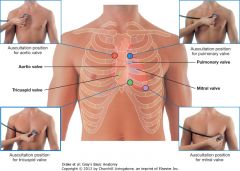
Tricuspid valve: heard just to left of sternum near fifth intercostal space
Mitral valve: head over apex of heart in left fifth intercostal space at the midclavicular line Pulmonary valve: head over medial end of left second intercostal space Aortic valve: heard over medial end of right second intercostal space |
|
|
Describe normal/balance coronary arterial distribution of the heart.
|
---posterior interventricular artery arises from the right coronary artery
---left coronary artery has small posterior branch for the left ventricle ---right coronary artery supplies posterior wall of right ventricle, posterior wall of left ventricle and posterior interventricular septum |
|
|
Describe the coronary arterial supply of a right dominant heart.
|

---very large posterior interventricular branch from right coronary artery
---circumflex branch from left coronary artery is weakly developed ---right coronary artery supplies everything but anterior wall of left ventricle and small area of anterior right ventricle (no variability in supply to atria/nodes) |
|
|
Describe the regions of the heart that would be damaged if the left marginal artery were occluded.
|
A portion of the left ventricle (obtuse margin of heart)
|
|
|
Describe the regions of the heart that would be damaged if the left circumflex branch were occluded.
|
Portion of left ventricle/atrium (passes through coronary sulcus, onto base/diaphramatic suface ending before posterior interventricular sulcus)
|
|
|
Describe the regions of the heart that would be damaged if the left anterior descending artery were occluded.
|
Anterior portion of left ventricle and right ventricle, interventricular septum (descends obliquely toward apex with some diagonal branches)
|
|
|
Describe the regions of the heart that would be damaged if the left coronary artery were occluded.
|
Left atrium, all of left ventricle except 1/2 of posterior, 1/2 of anterior right ventricle and anterior 2/3 of interventricular septum
|
|
|
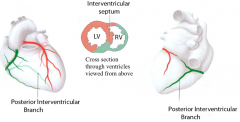
Describe the regions of the heart that would be damaged if the posterior interventricular branch were occluded.
|
Right ventricle and posterior interventricular septum (lies in posterior interventricular sulcus)
|
|
|
Describe the regions of the heart that would be damaged if the right marginal artery were occluded.
|
Right ventricle (continues towards apex of heart)
|
|
|
Describe the regions of the heart that would be damaged if the sinu-atrial nodal branch were occluded.
|
SA node
|
|
|
Describe the regions of the heart that would be damaged if the right coronary artery were occluded.
|
Right atrium, 1/2 of posterior wall of left ventricle, 1/2 of anterior and all of posterior and lateral walls of right ventricle, posterior 1/3 of interventricular septum, SA node and AV node
|
|
|
Describe the coronary venous supply of the heart.
|
Coronary sinus empties into right atrium and receive four main tributaries:
---great cardiac vein: begins at apex, ascends parallel to anterior interventricular artery, then follows the left circumflex branch to gradually enlarge and become the sinus ---middle cardiac vein: begins at apex and parallels posterior interventricular artery ---small cardiac vein: begins in coronary sulcus between right atrium and ventricle, paralleling right coronary artery ---posterior cardiac vein: lies on posterior surface of left ventricle to left of middle cardiac vein |
|
|
Describe the cardiac conduction system.
|
It initiates and coordinates contraction of the musculature of the atria and ventricles; it is a unidirectional pathway, with each branch isolated from surrounding myocardium by connective tissue, decreasing inappropriate stimulation of myocardium
---Sinu-atrial node: impulses begin here (cardia pacemaker); collection of cells located in crista terminalis of right atrium; excitation signals spread across atria, causing contraction ---Atrioventricular node: is stimulated by SA node; located near opening of coronary sinus within atrioventricular septum; forms beginning of atrioventricular bundle ---Atrioventricular bundle: direct continuation of AV node; follows lower border of membranous interventricular septum before splitting into right and left bundles ------right bundle branch: continues on right side of septum to apex of right ventricle, then enters septomarginal trabecula to reach base of anterior papillary muscle, then divides into final component ------left bundle branch: passes on left side of septum and descends to apex, giving off branches of final component ---Subendocardial plexus of conduction cells (purkinje fibers): continuous with left/right bundle branches; spreads impulse throughout ventricle to supply musculature including papillary muscles |
|
|
Describe the autonomic innervation of the heart. How does this affect the cardiac conduction system?
|
Regulates heart rate, force of each contraction and cardiac output
---these branches affect nodal tissue and other conduction system components Parasympathetic and sympathetic fibers both contribute to the cardiac plexus ---superficial part: inferior to aortic arch, between it and pulmonary trunk ---deep part: between aortic arch and tracheal bifurcation Parasympathetic: decreases HR, reduces force of contraction, constricts coronary arteries ---preganglionic fibers reach heart from branches of right and left vagus nerves; synapse in ganglia in plexus or on atrial walls Sympathetic: increases HR, increases force of contraction ---fibers reach plexus through sympathetic trunk (preganglionic: upper four/five thoracic spinal cord segments synapse in cervical/upper thoracic sympathetic ganglia/postganglionic: proceed as bilateral branches to plexus) Visceral afferents: pass through plexus and return to CNS via sympathetic trunk and vagal cardiac branches ---Vagus: sense changes in BP and blood chemistry (cardiac reflexes) ---Sympathetic: return to cervical/thoracic and re-enter via upper four/five thoracic spinal cord segments |
|
|
Describe how referred pain works in regards to myocardial ischemia and what nerve fibers are involved.
|
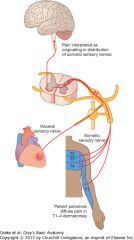
When cardiac cells die (ischemia), visceral afferent (pain) fibers are stimulated; these fibers follow the course of sympathetic fibers that innervated the heart and enter the spinal cord at T1-T4
---both somatic and visceral fibers synapse with the same fibers that ascend to the somatosensory area of the brain and it is unable to distinguish between the visceral/somatic distribution, so pain is interpreted as somatic ---this leads to medial arm pain and front chest pain because of T1-T4 dermatomes |
|
|
What is the thymus?
|
It is a bilobed gland that is involved in early development of the immune system and usually atrophies after puberty.
|
|
|
Where are the right and left brachiocephalic veins found?
|
They form at the junction between the internal jugular and subclavian veins and join to form the superior vena cava
---left is longer than right |
|
|
Where is the left superior intercostal vein found and what does it receive?
|
Receives posterior intercostal veins, left bronchial veins and sometimes the left pericardiacophrenic vein
Passes over left side of aortic arch and enters left brachiocephalic vein |
|
|
Describe the superior vena cava.
|
It begins at the right first costal cartilage, where brachiocephalic veins join and terminates where it joins with the right atrium
|
|
|
Describe the aortic arch and its branches.
|
Arch begins once ascending aorta leaves the pericardial sac and ends on left at T4/5; is anterior, then lateral to trachea
Three branches: ---brachiocephalic trunk: first, largest branch (anterior), eventually divides into right subclavian and right common carotid arteries ---left common carotid artery: ascends along left side of trachea ---left subclavian artery: most posterior, third branch, ascends along left side of trachea |
|
|
Describe the trachea and esophagus within the superior mediastinum.
|
Trachea: midline structure, bifurcates just at/inferior to sternal angle into right/left main bronchik
Esophagus: posterior to trachea, immediately anterior to vertebral column, continues into posterior mediastinum ---both have significant mobility in their vertical positioning ---both are crossed laterally by azygos vein on right and aortic arch on left |
|
|
Describe the vagus and phrenic nerve paths within the thorax and what structures they associate with.
|
Vagus: provides parasympathetic innervation to thoracic viscera and carry visceral afferents from viscera
---visceral afferents relay info to CNS about normal physiological processes and reflexes; they do not transmit pain ------Right: passes along lateral surface of trachea, posterior to root of right lung and crossed by azygos vein; branches into esophagus, cardiac/pulmonary plexus ------Left: crosses left side of aortic arch, posterior to root of left lung; branches into esophagus, cardiac/pulmonary plexus; also gives rise to left recurrent laryngeal nerve: ascends to larynx between trachea and esophagus Phrenic: (C3-C5) supply motor and sensory innervation to diaphragm and associated membranes; innervate mediastinal pleura, fibrous pericardium and parietal layer of serous pericardium ------Right: enters lateral to vagus, continues on right of SVC, is accompanied by pericardiacophrenic vessels ------Left: lies lateral to vagus nerve and aortic arch, is accompanied by pericardiacophrenic vessels |
|
|
Describe the thoracic duct in the superior mediastinum.
|
Major lymphatic vessel in body, passes through posteriorly.
|
|
|
Describe the location and structures of the posterior mediastinum.
|
---posterior to the pericardial sac and anterior to bodies of mid/lower thoracic vertebrae
Contains: ---esophagus and associated nerve plexus ---thoracic aorta and branches ---azygos system of veins ---thoracic duct and lymph nodes ---sympathetic trunks ---thoracic splanchnic nerves |
|
|
Describe the thoracic aorta and its branches (7). How do these arteries contribute to collateral circulation in the thorax?
|
It is a portion of descending aorta starting at T4 and ending at T12, gives off many branches
---Pericardial branches: to posterior pericardial sac ---Bronchial branches: vary in number, size, origin ---Esophageal branches: four/five form anastomotic chain with branches from inferior thyroid artery (superior), left inferior phrenic and left gastric arteries (inferior) ---Mediastinal branches: supply lymph nodes, vessels, nerves, areolar tissue ---Posterior intercostal arteries: supply lower nine spaces; anastomose with anterior intercostal arteries ---Superior phrenic arteries: supply posterior part of superior diaphragm; anastomose with musculophrenic and pericardiacophrenic arteries ---Subcostal artery: lowest pair of branches inferior to rib 12 |
|
|
Describe the azygos system of veins.
|
Drain blood from body wall and move it superiorly to SVC; blood from some thoracic viscera may also enter; anastomoses form with abdominal veins
---important anastomotic pathway for venous blood from lower body to heart if IVC is blocked Azygos vein: arises at junction between right ascending lumbar and right subcostal veins (L1/2) or can be direct branch from IVC; enters thorax through aortic hiatus of diaphragm and joins SVC ---Tributaries: right superior intercostal vein, right posterior intercostal veins, hemiazygos and accessory hemiazygos veins, esophageal veins, mediastinal veins, pericardial veins and right bronchial veins Hemiazygos vein: arises at junction of left ascending lumbar and left subcostal veins; ascends on left until T9, then passes posterior to esophagus/thoracic duct/aorta to enter azygos vein ---Tributaries: lower left posterior intercostal veins, esophageal and mediastinal veins Accessory hemiazygos vein: descends from left, crosses vertebral column to join azygos; usually connected to left superior intercostal veins ---Tributaries: higher posterior intercostal veins, left bronchial veins ------Origin, course, tributaries, anastomoses and termination is variable |
|
|
How is the muscle in the wall of the esophagus organized?
|
Upper 5% is only skeletal muscle; middle 45% is both skeletal muscle and smooth muscle; distal 50% is only smooth muscle
|
|
|
What are the five sites of normal esophageal constriction?
|
1. The junction of the pharynx and esophagus
2. at the aortic arch* 3. at the tracheal bifurcation where left main bronchus crosses esophagus 4. at the left atrium* 5. at the esophageal hiatus in diaphragm |
|
|
What is the vascular supply of the esophagus?
|
Arteries:
---cervical: inferior thyriod arteries (from subclavian>thryocervical>) which give off ascending and descending branches that anastomose across the midline ---thoracic: four/five branches from thoracic aorta ---abdominal: left gastric artery (abdominal>celiac>) Veins: ---cervical: to inferior thyroid veins (to brachiocephalic>SVC) ---thoracic: esophageal plexus (to azygos veins>SVC) ---abdominal: left gastric vein (to portal vein>hepatic sinusoids>central veins>hepatic veins>IVC) |
|
|
How is the esophagus innervated?
|
Striated (skeletal) muscle is upper portion is innervated by branchial efferents from vagus nerves
Smooth muscle is innervated by parasympathetic fibers and visceral efferents from vagus nerves ---preganglionic fibers synapse in myenteric and submucosal plexuses of enteric nervous system in esophageal wall Sensory innervation involves visceral afferent from vagus nerves, sympathetic trunks and splanchnic nerves ---Vagus: relay info to CNS about normal physiological processes and reflexes (no pain recognition) ---Sympathetic (incl. splanchnic): primary receptors for pain and transmission of this info |
|
|
Describe the features of cardiac muscle.
|
It has three layers:
1. Epicardium: outer most layer (visceral pleura), surrounds all muscle ---subepicardial space: (loose connective tissue) contains blood vessels and parasympathetic ganglia 2. Myocardium: middle layer, contains striated muscle cells in bundles 3. Endocardium: inner most layer, made of simple squamous epithelium which prevents blood clots from forming ---subendocardial space: contains blood vessels and branches of the cardiac conduction system |
|
|
Describe the features of cardiac muscle cells.
|
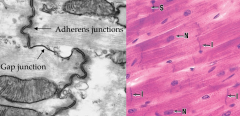
Striated, formed by individual branching cells each with own single nucleus
Connected by intercalated discs: formed from gap junctions (allows for passage of ions to adjacent cells; no need for nerves as depolarizing signal passes from one cell to another); adherens junctions/desmosomes (acts like Z-line, α-actinin) Has single large T-tubule at Z-line and limited SR Contraction dependent on large influx of extracellular Ca2+ High density of mitochondria (40% volume) Undergoes hypertrophy when worked hard |
|
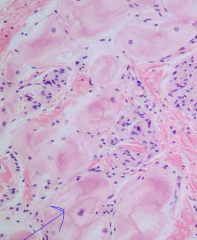
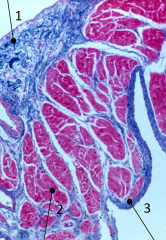
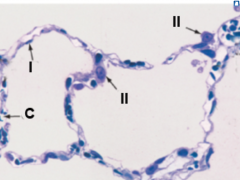
What types of cells are these and where are they found? Why is their staining so light?
|
Purkinje cells: located in subendocardial space
---lost myofilaments (light staining), so can't contract, but has lots of gap junctions to spread signals |
|
|
Describe the features of smooth muscle cells.
|
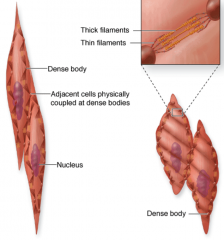
Non-striated: has myofilaments that are attached to the plasma membrane through dense bodies
Two sources of Ca2+ (needed for contraction) ---Ca2+ channels in cell membrane: allow for influx of Ca2+ in response to signal to contract ---Ligand receptors on cell membrane trigger second messangers (cAMP/IP3) which cause release of Ca2+ from Caveolea/SR (storage site) -------Increase cytoplasmic Ca2+ binds to Calmodulin (protein) that activates Myosin Light-Chain Kinase (MLCK); also causes exposure of myosin binding sites on actin thin filaments ------MLCK actives myosin through phosphorylation of light chains on myosin heads, leading to conformational change and increased ATP binding/ATPase activity (sliding filament model) -------All leads to increased muscle tension |
|
|
Describe the features of blood vessels.
|
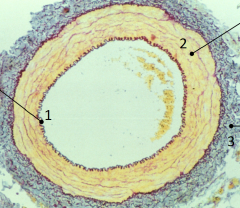
Arteries and veins:
1. Tunica intima: inner-most layer; composed of single layer of endothelium with non-thromobogenic properties; important in regulation of contraction of smooth muscle in tunica media 2. Tunica media: middle layer; formed from concentric circles of smooth muscle with elastic fibers, type III collagen and proteoglycans 3. Tunica adventitia (externa): outer-most layer; composed of fibroblasts, type I collagen and few elastic fibers ---larger vessels have vaso vasorum in adventitia/media; composed of arterioles, capillaries and venules to provide nutrients to outer layer because so thick (most in veins because transport deoxygenated blood) ---larger vessels also have vasomotor nerves (sympathetic) in adventitia to regulate contraction in tunica media (vasoconstriction) Capillaries: composed of single layer of endothelial cells |
|
|
Describe the cardiac conduction system.
|
Sinuatrial (SA) node: found at junction of SVC with right atrium in subepicardial space; acts as pacemaker of heart (automatically depolarizes at fixed rate)
---signal passes through myogenic transduction (1 cell receives signal, passes it to adjacent cells) ---impulse is sent to right and left atria, then to AV node Atrioventricular (AV) node: will assume pacemaker role if SA node destroyed; located in right atrial septum near coronary sinus, connects to bundle of His AV bundle of His: travels in subendocardial space on right side of cardiac skeleton; splits in interventricular septum to right/left branches ---left branch further divides ---portion of right branch passes through moderator band to supply anterior papillary muscle Purkinje cells: termination of conduction system (continuous with bundle branches); found in subendocardial space, transmit signal through gap junctions |
|
|
Describe the three different types of arteries.
|
1. Elastic (conducting): alternating layers of smooth muscle and elastic laminae in thick tunica media; abundant vaso vasorum; helps to maintain blood pressure by contracting/recoiling
---found in thoracic aorta (lots of blood flow) 2. Muscular (distributing): narrower tunica intima, internal/external elastic lamina, fewer elastic lamina in tunica media ---Radial/ulnar/brachial arteries: involved in regional distribution of blood flow 3. Arterioles: wall thickness equal to diameter of lumen; one to three layers of smooth muscle in tunica media ---regulation of blood flow into tissue capillary beds |
|
|
Describe the three different types of capillaries.
|
All associated with pericytes (regulation proliferation of endothelia cells/blood flow)
---provide fluid, gas and small molecule exchange 1. Continuous: tight intercellular junctions; have lots of vesicles for transporting materials ---found in muscle, nervous and connective tissue 2. Fenestrated: permanent channels or fenestrations across endothelial cells; allow for more movement of material ---found in GI and endocrine systemes 3. Sinusoidal: large discontinuities between endothelial cells; easy movement across membrane ---found in bone marrow, liver, spleen and lymph nodes |
|
|
Describe how fluid exchange is regulated in the capillary bed/surrounding tissue by hydrostatic and osmotic forces.
|
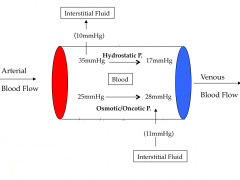
Hydrostatic pressure: higher in arterial side than osmotic pressure, so forces fluids out of capillaries
Osmotic pressure: higher in venous side than hydrostatic pressure, so forces fluid in to capillaries ---driven by protein concentration (higher concentration=low fluid, so brings fluid in on venous end) |
|
|
How does tissue edema occur?
|
Edema: excess fluid in interstitial space
Occurs by affecting either hydrostatic or osmotic pressure: 1. Increase venous pressure (hydrostatic): decreased pressure forces less fluids in 2. Hypertension: increase hydrostatic pressure at arterial end; forces more fluid out 3. Liver disease: not producing plasma proteins, decrease osmotic pressure; less fluid in 4. Lymphatic obstruction: decreased uptake of fluids into lymphatic system |
|
|
Describe angiogenesis.
|

Formation of new capillaries from existing capillaries
Normal: occurring in wound healing, menstruation Abnormal: occurring in tumors, retina due to diabetes 4 steps: 1. stimulation of endothelial cells by angiogenic factors (ex: low oxygen) 2. degradation of parental vessel basal lamina by activated endothelial cells and the formation of endothelial sprouts 3. endothelial cell migration and proliferation 4. new vessel stabilization/maturation ---synthesis of new basal lamina |
|
|
Describe the conducting portion of the respiratory system.
|
Composed of:
---trachea ---primary bronchi ---secondary (lobar) bronchi: 3 on right/2 on left ---tertiary (segmental) bronchi: bronchopulmonary segments ---bronchioles Structural trends with decreasing diameter: ---decreased cartilage ---decreased glands/goblet cells ---decreased height of epithelium (columnar>cuboidal>squamous) ---increased smooth muscle/elastic connective tissue ***bronchioles: do not have cartilage rings, only smooth muscle |
|
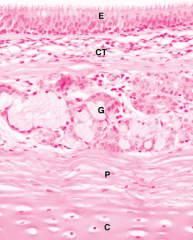
Describe the different layers found in the trachea.
|
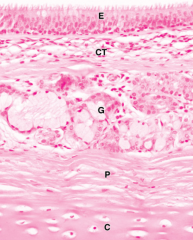
E: Mucosa - respiratory epithelium (pseudostratified ciliated columnar)
---has goblet cells, connected to basal lamina CT: Lamina propria - loose connective tissue G: Submucosa - seromucous glands in loose connective tissue; produce mucosa to trap inhaled molecules and serous to lubricate P: Perichondrium - part of adventitia C: Hyaline cartilage - part of adventitia |
|
|
Describe the respiratory portion of the respiratory system.
|
Composed of alveolar sacs:
---gases are exchanged between alveoli and surrounding capillary beds formed by pulmonary arteries and veins |
|
|
Describe the composition of an alveoli.
|
Composed of two different types of cells:
1. Type I alveolar cells: ---contributes to ~97% of alveolar surface ---simple squamous epithelium; involved in gas exchange 2. Type II alveolar cells: ---contributes to ~3% of alveolar surface ---simple cuboidal epithelium; secretes pulmonary surfactant (phospholipids, cholesterol, surfactant proteins) to decrease surface tension and prevent alveolar collapse during expiration C: capillaries |
|

Describe how the respiratory membrane works. What happens when it doesn't work?
|

Blood-air barrier:
---consists of type I alveolar cells, capillary epithelium and intervening basal lamina ---permeable to molecular oxygen, carbon dioxide, carbon monoxide and other gases Pulmonary edema: results from increased permeability of fluid, protein and leukocytes moving from capillary and interstitial space into alveolar space ---prolonged damage to respiratory membrane can result in deposition of excess fibrous connective tissue (fibrosis); increased thickening/decreased compliance leads to decreased oxygen diffusion capacity and restrictive lung disease. |
|
|
Where do the cells that form the early embryonic heart originate from?
|
Heart develops in 3rd week from lateral plate splanchnic mesoderm; the cardiogenic area lies above the neural tube.
|
|
|
How does the early tubular heart form?
|
It starts as angiogenic clusters in each splanchnic mesoderm, which form into endocardial tubes (one on each side). Lateral folding brings the two splanchnics together and the endocardial tubes fuse into one tube.
|
|
|
How does the heart move into its position in the body?
|
The cardiac area and pericardium start above the neural tube (head) and move into the thorax as head fold forms, rotating medially.
|
|
|
What is the basic plan of the circulatory system in early development (3.5 weeks)?
|
Series of aortic arches carry blood from heart to dorsal aortae (carry deoxygenated blood); veins carry oxygenated blood
---some portions of this system degenerate resulting in normal anatomy of great vessels |
|
|
What are the distinct regions of the early tubular heart? What regions do they form in the adult heart?
|
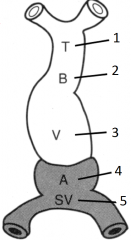
---Arterial portions:
1. Truncus arteriosus: forms proximal aorta and pulmonary trunk 2. Bulbus cordis: forms conus arteriosus (on right), aortic vestibule (on left; outflow tracks), and trabeculated part of right ventricle 3. Primitive ventricle: forms trabeculated part of left ventricle --Venous portions: 4. Primitive atrium: trabeculated parts of right and left atria (auricles) 5. Sinus venosus (has two horns): smooth part of right atrium (right horn), coronary sinus (left horn), and oblique vein of left atrium |
|
|
How does looping of the heart occur?
|

Ventricular region start above the atrial region
---ventricular region bend ventrally, caudally and to the right ---atrial region shifts dorsally, cranially and to the left |
|

What is this condition called and what causes it?
|

Dextrocardia: right-sided heart
---heart looped to left and ended up on right ------heart normally loops to right and ends up on left |
|
|
How does septation of the atrioventricular canal occur?
|
After looping during weeks 4-5:
---endocardial cushions (dorsal/inferior and ventral/superior) are masses of tissue that grow towards each other and fuse in middle, leaving two canals on right and left |
|
|
How does septation of the atria occur?
|
Septum primum forms in roof of primitive atria (between right and left)
---foramen primum remains open between septum primum and AV cushions ---foramen secundum forms in center of septum primum through cell death, superior to foramen primum ------once secundum forms, primum closes ---septum secundum forms to right of septum primum ---foramen ovale is the opening left in septum secundum (no cell death, just doesn't form) |
|
|
Why are the foramena that are formed during atrial septation so important?
|
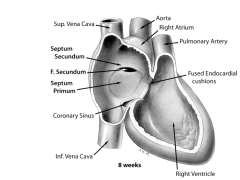
The lungs are not functioning in an unborn fetus, so there is no reason for blood to pass through
---the thin, flexible septum primum allows blood from right atrium to pass into left atrium through foramen ovale in septum secundum ------After birth, once infant takes first breath, pressure of blood in the left atrium pushes septum primum into septum secundum and the two fuse |
|
|
What happens when there is incomplete fusion of septum primum and septum secundum after birth?
|
Atrial septal defect (ASD):
---results in a left to right shunt of blood (because pressure is higher on left) ------usually compatible with many years of symptom-free life; long term may lead to right atrial hypertrophy and pulmonary hypertension Potential causes: excessive tissue resorption around foramen secundum or hypoplastic growth of septum secundum forming a large foramen ovale ---6.4/10,000 births (2:1 female to male) |
|
|
How does ventricular septation occur?
|
The walls of the ventricles grow quickly and they become closely opposed, forming the muscular portion of the interventricular septum
---formed by myocytes The upper most portion of the interventricular septum, closest to the atria, forms a membranous portion from AV cushions and the aorticopulmonary septum |
|
|
How does outflow tract septation occur?
|

Separation of aorta and pulmonary trunk:
---ridges (truncoconal cushions) form on opposite sides of outflow tract and spiral down toward ventricle ------spiraling necessary for aorta to come off left and pulmonary trunk to come off on right (if switched, oxygenated/deoxygenated blood would pump the wrong way) ---fusion of ridges form the aorticopulmonary (spiral) septum, which divides the outflow tract into aortic/pulmonary trunks ------inferior ends form the membranous ventricular septum |
|
|
What happens when the ventricular septum doesn't completely close?
|
Ventricular septal defect (VSD):
---typically occurs in membranous portion (where multiple tissues converge); less common in muscular part ------results in left to right shunt of blood; long term leads to right ventricle hypertrophy, reversal of shunt and pulmonary hypertension ***most common congenital cardiac anomaly (12/10,000) |
|
|
What happens with there are anomalies in spiral septum formation?
|
---No septum forms: there is one common arterial trunk and oxygenated/deoxygenated blood runs together
---Septum doesn't spiral: transposition of great arteries (TGA); aorta transports deoxygenated blood and pulmonary trunk transports oxygenated blood ---Persistant ductus arteriosus (between aorta and pulmonary trunk) in presence of pulmonary stenosis (too small trunk): some oxygenated blood is carried back to lungs through trunk ---Tetrology of Fallot: pulmonary stenosis, overriding aorta (takes both oxy/deoxy), patent interventricular septum with right to left shunt, hypertrophic right ventricle ------most common: 9.6/10,000 |
|
|
Describe fetal circulation.
|
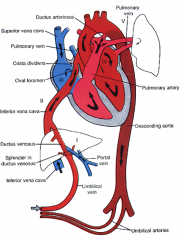
Blood enters from placenta (80% O2) > umbilical vein > (I) mixes with blood from portal vein (oxy mixes with deoxy); ductus venosus shunts blood to IVC, bypassing liver and regulates blood flow > (II) mixes with blood from lower limbs in IVC > into right atrium (two paths):
1. (III) mixes with blood from head/arms from SVC into right ventricle > pulmonary trunk > ductus arteriosus > *descending aorta, (V) mixes with blood from DA* 2. foramen ovale > left atrium, (IV) mixes with blood from lungs > left ventricle > ascending aorta > *descending aorta, (V) mixes with blood from DA* |
|
|
Describe neonatal circulation.
|
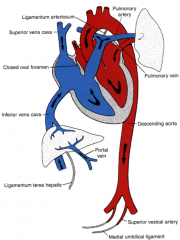
Respiration begins (pressure is relieved on pulmonary arteries) > umbilical arteries close > umbilical veins/ductus venosus close (become umbilical ligaments/ligamentum teres hepatis) > ductus arteriosus contracts due to branykinin from lungs (becomes ligamentum arteriosum) > blood to lungs increases > pressure in left atrium increases > foramen ovale closes as septum primum is pushed against septum secundum (forms fossa ovale)
|
|
|
Describe the formation of the lungs.
|
Lungs are derivatives of primitive gut tube; lateral folding established ventral body wall and gut tube
Lung bud: forms from the ventral foregut ---tracheoesophageal ridges separate lung bud from foregut; ridges fuse into tracheoesophageal septum, dividing trachea/bronchial buds from esophagus ---bronchial buds form right/left main bronchi > branch into 3R/2L secondary bronchi > each branch into 10 tertiary (segmental) bronchi ***epithelium of larynx, trachea, bronchi and lungs: endoderm ***other components: splanchnic mesoderm |
|
|
What happens when there is an abnormality in the tracheoesophageal septum formation?
|

5 different scenarios:
---Tracheoesophageal fistual: esophagus is cut in the middle, leading to a proximal blind-end part of esophagus and a distal end connected to the trachea (90%) ---Esophageal atresia: esophagus is completely severed, with no connections to trachea (4%) ---Communication of esophagus with trachea: incomplete separation, with part of esophagus still attached to trachea but esophagus one piece (4%) ---Proximal end of esophagus stays connected to trachea, with distal end severed (1%) ---Proximal and distal ends of esophagus connect to trachea but not to each other (1%) |
|
|
Describe the maturation of the lungs.
|
1. Pseudoglandular period (5-16 wk): branching forms 10 terminal bronchioles
2. Canalicular period (16-26 wk): terminal bronchioles divide into respiratory bronchioles; vascularization of visceral mesoderm; epithelium is cudoidal (no gas exchange) 3. Terminal sac period (26 wk to birth): terminal sacs (primitive alveoli) form and capillaries establish contact; epithelium differentiates into thin type I alveolar cells; type II alveolar cells produce surfactant 4. Alveolar period (8 mo to 8 yr): mature alveoli have well developed epithelial-endothelial (capillary) contacts |
|
|
Describe respiratory distress syndrome.
|
If the infant is born too early (before 26 wk), they have not produced surfactant, which lowers the surface tension at air-alveolar interface, and alveoli collapse during expiration due to increased surface tension
---20% of newborn deaths are caused by insufficient surfactant Artificial surfactant or glucocorticoids to stimulate surfactant production allows survival of babies as young as 5.5 mo gestation ---can test for surfactant production through amniocentesis and measure lecithin-sphingomyelin (phospholipids) ratio |
|
|
Describe the formation of the pericardial and pleural cavities.
|
---lung bud endoderm/mesoderm push into the developing pleural cavity
---mesoderm cells lining pleural cavities form the parietal and visceral pleurae ---folds of tissue fuse to separate pleural and pericardial cavities ---lungs expand as pleural cavities enlarge, surrounding heart on sides |
|
|
Describe heart sounds.
|
Systole: first heart sound "lub", caused by closure of tricuspid and mitral valves
Diastole: second heart sound "dub", caused by closure of aortic and pulmonary valves |
|
|
Describe the coronary arterial supply of a left dominant heart.
|

---posterior interventricular branch arises from circumflex branch of left coronary artery
---right coronary artery is weakly developed on posterior ventricular wall ---left coronary artery supplies everything but lateral wall of right ventricle (no variability in supply of atria and nodes) |

