![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
87 Cards in this Set
- Front
- Back
|
Describe the osseous components of the pelvis and identify important gender differences in the pelvis.
|
Pelvis: formed from the fusion of three bones
---Ilium ---Ischium ---Pubis The fusion of these three forms the acetabulum Pelvic bones (ilium specifically) articulate with the sacrum at the sacroiliac joint; sacrum articulates with the coccyx inferiorly False pelvis: superior region of upper portion of pelvis/lumbar vertebrae True pelvis: inferior parts of pelvic bones, sacrum, coccyx Gender differences: ---Pelvic inlet: women - wide, oval; men - narrow, heart-shaped ---Sacrum: women - short, straight; men - long, prominent ---Coccyx: women - straighter; men - curves ventrally ---Sciatic notch: women - wide; men - narrow ---Sub-pubic angle: women - broad, rounded (curve of thumb/index); men - deep, acute (curve of index/middle) |
|
|
Name the attachments of the sacrotuberous and sacrospinous ligaments. What foramina do they form?
|
Sacrotuberous ligament: attaches from the ischial tuberosity to the sacrum; forms greater/lesser sciatic notch
Sacrospinous ligament: attaches from ischial spine to sacrum; forms greater/lesser sciatic notch |
|
|
Describe the muscles and fascia of the pelvic floor, their function and innervation.
|
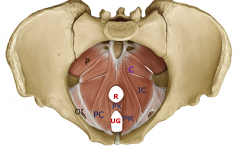
Pelvic floor composed of four paired muscles; pelvic diaphragm consists of two muscles (coccygeus, levator ani)
---Piriformis: lateral rotation of extended hip joint; abduction of flexed hip; innervation: nerve to obturator internus (L5,S1-2) ---Obturator internus: lateral rotation of extended hip joint, abduction of flexed hip; innervation: nerve to obturator internus (L5, S1) ---Coccygeus: contributes to formation of pelvic floor, supporting pelvic viscera; maintains angle between rectum and anal canal and reinforces external anal sphincter; innervation: branches from anterior rami S4 and inferior rectal branch (pudendal) S2-4 ---Levator ani: contributes to pelvic floor, supports viscera; pulls coccyx forward after defectation ------formed from collection of muscle fibers: puborectalis (PR) - important in changing anorectal angle during val salva maneuver, pubovaginalis/pubprostaticus (PX), pubococcygeus (PC), iliococcygeus (IC) ---All covered by endopelvic fascia and peritoneum; obturator internus' fascia forms tendinous arch; perineal membrance is thick fascial triangular structure attached in pubic arch (forms UG diaphragm) |
|
|
Describe the urogenital diaphragm, the function of its muscles and their innervation.
|
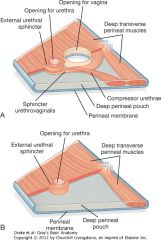
Perineal membrane forms the base; all muscles are innervated by pudendal nerve (S2-4)
---External urethral sphincter: compresses the membranous urethra, relaxes during micturition ---Deep transversalis perineal: stabilizes the position of the perineal body (tendon/converging point of msucles) ---Compressor urethrae (women only): functions as accesssory sphincter of urethra ---Sphincter urethrovaginalis (women only): functions as accessory sphincter of urethra |
|
|
Describe the organization of fascia and peritoneum in the pelvis and the fossae, pouches and folds it creates.
|
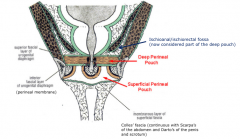
Perineum:
---superficial fascia: fatty layer (usually thick) ---deep fascia: Colles'; fibrous layer ---Superficial perineal pouch: from Colles' fascia to perineal membrane; contains genitalia and musculature ---Deep perineal pouch: from perineal membrane to endopelvic fascia of pelvic diaphragm; includes the UG diaphragm Peritoneum: ---Women: ---recto-uterine pouch is posterior, between uterus/recturm; vesico-uterine pouch is anterior, between bladder/uterus ---broad ligament: sheetlike fold from lateral pelvic wall to uterus; composed of three parts - mesometrium (lateral/attaches to body), mesosalpinx (superior/suspends uterine tube), mesovarium (posterior/attches to ovary) ---suspensory ligament of ovary: raised fold of peritoneum; contains ovarian vessels, nerves, lymph ---round ligament of uterus: passes over pelvic inlet through inguinal canal to labium majus ---Men: ---rectovesical pouch: between bladder/rectum |
|
|
Describe the ligaments found in the female pelvis.
|
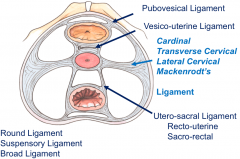
All work as stabilizers/supporters of the uterus, rectum and bladder
---Round ligament, suspensory ligament and broad ligament are formed from peritoneum; for uterine support ---Vesico-uterine ligament, pubovesical ligament, cardinal (transverse cervical) ligament and utero-sacral (recto-uterine/sacro-rectal) ligaments are formed from fascia; extend between bladder/uterus and from cervix to anterior, lateral and posterior pelvic walls, respectively ***Cardinal ligament: contains uterine artery (which is superior to ureter)*** |
|
|
Describe the location of the urinary bladder in the pelvis and the ligaments that support it.
|
Most anterior element of the pelvic viscera; when empty, is entirely in pelvis, but expands superiorly into abdominal cavity when full
---shaped like three-sided pyramid on its side Ligaments: anchor the neck (most inferior portion) ---women: pubovesical ligaments - attach bladder to posteroinferior aspect of pubis; work with perineal membrane, associated muscles, levator ani and pubic bone to support bladder ---Men: puboprostatic ligaments - attach bladder to posteroinferior aspect of pubis; blend with fibrous capsule of prostate |
|
|
What is the neurovascular supply of the bladder?
|
Blood supply:
---from branches of the anterior trunk of the internal iliac artery ---superior vesical artery (from umbilical artery) ---inferior vesical artery (men)/vaginal artery (women) ---Veins: follow arteries; also form pelvic venosus plexus Innervation: ---Sympathetic: preganglionic - T10-12 (lesser/least splanchnic) and L1-2 (lumbar splanchnic); ganglia - pelvic ganglia; postganglionic - hypogastric plexus ---Vasoconstriction, relaxation of bladder smooth muscle, contraction of smooth muscle of internal urethral/anal sphincters, contraction of smooth muscle of reproductive tract, ejaculation ---Parasympathetic: preganglionic - S2-4 (pelvic splanchnic); ganglia - located in wall of organ; postganglionic - hypogastric plexus ---vasodilation, contraction of bladder smooth muscle, relaxation of smooth muscle and internal anal sphincter, modulate activity of enteric nerves to increase peristalsis of distal colon/rectum, erection |
|
|
What is the process of micturition and how is it controlled neurologically?
|
Micturition is regulated by an autonomic spinal cord reflex (micturition reflex); involves impulses traveling form bladder to sacral spinal cord and back to bladder
---can be inhibited/facilitated by neurons located in the cerebral cortex or brainstem Two phases: ---Bladder filling: controlled by sympathetic (symp. stores) - lumbar/sacral splanchnic (L1-2)/inferior hypogastric plexus; hypogastric nerves cause relaxation of detrusor muscle and contraction of internal sphincter to allow filling ---Bladder emptying/voiding: controlled by parasympathetic - sensory stretch fibers in bladder wall/parasymp. fibers in pelvic splanchnic nerves; located in sacral spinal cord and regulated by higher centers of the brain ---first sense urge for voluntary empyting at 150mL, fullness at 400-500mL ---sensory info conveyed through visceral afferent fibers with pelvic splanchnic; synapse in sacral spinal cord, also conveyed to brain ---Completing the voiding: ---visceral afferent stimulate parasymp. in sacral spine causing contraction of detrusor; stimulate ascending pathways that result in conscious desire to urinate ---descending impulses decrease symp. output via hypogastric plexus to internal urethral sphincter allowing relaxation; stimulate parasymp. for detrusor contraction; inhibit pudendal nerve activity to allow for voluntary relaxation of external urethral sphincter ---Inhibiting micturition reflex: ---efferent impulses from brain inhibit preganglionic parasympathetic in sacral spinal cord and continue to stimulate contraction of external sphincter via pudendal nerve |
|
|
Describe the anatomy of the pelvic parts of the GI system and their neurovascular supply.
|
Rectum:
---follows concave of sacrum, is continuous with sigmoid superiorly and anal canal inferiorly; lacks taenia coli and haustra; rectal ampulla is an expanded portion in the lower part Anal canal: ---begins at terminal portion of the rectal ampulla, passes through the pelvic floor and terminates as the anus in the perineum; surrounded by internal/external anal sphincters; is lined by mucosa proximally/non-keratinized stratified squamous distally; has longitudinal folds (anal columns) united inferiorly by anal valves which form the pectinate line as well as depressions (anal sinuses) superior to the valves Innervation; ---Sympathetic: lumbar/sacral splanchnic nerves (L1-2); hypogastric plexus and pelvic ganglia ---Parasympathetic: pelvic splanchnic (S2-4); hypogastric plexus ---Somatic: pudendal nerve - controls the external anal sphincter Blood supply: ---Arteries: middle rectal artery (from anterior trunk of internal iliac) supplies rectum; anastomoses with superior rectal artery (inferior mesenteric) and inferior rectal artery (from internal pudendal) |
|
|
What are hemorrhoids and what are common causes of this condition?
|
An engorgement of veins related to the anal sphincter
---have slight genetic disposition but straining during bowel movements, obesity and sedentary lifestyle can also produce them, as well as portal hypertension ---internal hemorrhoids originate from internal rectal venous plexus and usually bleed ---external hemorrhoids originate form the external rectal plexus and occur at distal boundary of anal canal |
|
|
What are the boundaries and divisions of the perineum?
|
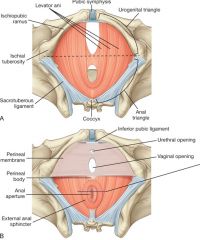
Diamond-shaped region inferior to pelvic floor between thighs
---anterior: urogenital triangle/diaphragm - contains openings of urinary/reproductive systems ---posterior: anal triangle - contains anus and external anal sphincter ***pudendal nerve and internal pudendal artery are the major nerve/artery*** |
|
|
Describe the external genitalia, its vascular supply and somatic/visceral innervations.
|
Lie within the superficial perineal pouch; has both erectile tissue (penis/clitoris) and skeletal muscle associated with erectile structures attached to perineal membrane/bone
Erectile tissue: central core of expandable vascular tissue and surround connective tissue capsule ---Two sets join together: ---corpora cavernosa: pair of cylindrically shaped, anchored to pubic arch at proximal end (crura); form body of clitoris/dorsal part of penis ---surrounds opening of urogenital system: Women - bulbs of vestibule (pair) on each side of vaginal opening, anchored to perineal membrane; bands of erectile tissue connect to glans clitoris, which is midline at end of body of clitoris and anterior to urethral opening; Men - corpus spongiosum anchored at base (bulb) to perineal membrane, forms ventral part of penis/glans penis; urethra is enclosed in it Muscles: three pairs ---ischiocavernosus: anterior, along pubis; move blood from crura to body of erect penis/clitoris ---bulbospongiosus: medial, surrounding root of penis/clitoris; move blood into glans, (men) remove urine from urethral/pulsatile ejaculation ---superficial transverse perineal muscles: posterior, between ischial tuberosities; stabilize perineal body Blood supply: ---Arteries: internal pudendal artery*, external pudendal, testicular/ovarian arteries, and cremasteric arteries ---branches of internal pudendal: inferior rectal (anastomoses with superior/middle rectal arteries), perineal artery, terminal part supplies deep perineal pouch/erectile tissues ---Veins: accompany arteries, join internal pudendal vein; except deep dorsal vein of penis/clitoris, which joins venous plexus Innervation: ---Somatic: pudendal - three major branches are inferior rectal nerve, perineal nerve and dorsal nerv of penis/clitoris ---Visceral: cutaneous - postganglionic sympathetic delivered along pudendal; erectile - pass through deep perineal pouch through inferior hypogastric plexus |
|
|
What are the boundaries of the ischio-anal fossae and what neurovascular structures are found in this region?
|
---Lateral wall formed by ischium, obturator internus and sacrotuberous ligament
---Medial wall formed by levator ani muscles ---Superiorly, medial/lateral walls converge where levator ani attach to obturator internus fascia Contains the pudendal nerve and internal pudendal artery |
|
|
Describe the structures of the spermatic cord, their coverings and their origins.
|
Spermatic cord contains:
---ductus deferens, artery to ductus deferens (from inferior vesical artery), testicular artery, pampiniform plexus of veins, cremasteric vessels, genital branch of genitofemoral nerve, sympathetic/visceral afferent nerve fibers, lymph and remnants of processus vaginalis Covered by: ---internal spermatic fascia: innermost, arises from transervsalis fascia ---cremasteric fascia: arises from internal oblique muscle ---external spermatic fascia: outermost, arises from external oblique muscle |
|
|
Explain the function of the cremasteric and dartos muscles in the scrotum and describe the cremasteric reflex.
|
The muscles help to regulate the temperature of the scrotum by drawing the scrotum up towards the body in cold enviroments.
Cremasteric reflex: ---Stroking the skin of the superior/medial thigh stimulates sensory fibers that run with the ilioinguinal nerve and serve as the afferent limb; motor fibers that run with the genital branch of the genitofemoral nerve are distributed to the cremasteric muscle, where they cause contraction, elevating the testis (efferent limb) |
|
|
Describe the testis.
|
Oval-shaped, enclosed in elongated musculofascial pouch continuous with the anterior abdominal wall and projects into scrotum; connected to the spermatic cord
---covered by closed sac of peritoneum, tunica vaginalis (parietal/visceral layers) ---composed of seminiferous tubules (produce spermatozoa) and interstitial tissue surrounded by thick connective tissue capsule, tunica albuginea; tubules become rete testis, where efferent ductules branch from into the epididymis |
|
|
Describe the epididymis.
|
Single, long coiled duct that courses along the posterolateral side of the testis; where spermatozoa acquire the ability to move/fertilize an egg; end is continuous with ductus deferens
Composed of: ---efferent ductules: form enlarged coiled mass that sits on posterior/superior pole of testis and forms head ---true epididymis: single long coiled duct where efferent ductules drain |
|
|
Describe the ductus deferens.
|
Long muscular duct that transports spermatozoa to ejaculatory duct; is part of the spermatic cord and joins the duct of the seminal vesicle to from the ejaculatory duct.
|
|
|
Describe the seminal vesicle.
|
Accessory gland of the male reproductive system, develops as a blind-ended tubular growth from the ductus deferens; has numerous pocket-like outgrowths and is encapsulated by connective tissue to form an elongate structure
---joins with ductus deferens to form the ejaculatory duct ---produces secretions the contribute 60-85% of the ejaculate; it is alkaline (counter acidity), contains fructose (energy), prostaglandins (sperm motility/vaginal stimulation), fibrinogens (semen coagulation) and vitamin C |
|
|
Describe the prostate gland.
|
Accessory structure of male reproductive system that surrounds the urethra; surrounded by a fibrous capsule with thick fibromuscular septa, with two lobes that have branching tubular glands
---contributes 15-30% of ejaculate, is alkaline to slightly acidic, contains fibrinogens (coagulation), fibrinolytic agents (un-coagulate), citric acid (energy), zinc, (robusticity) and prostate-specific antigen (cancer marker) |
|
|
Describe the bulbourethral gland.
|
One on each side, are small, pea-shaped mucous glands that are lateral to membranous part of urethra
---contribute to the lubrication of the urethra and pre-ejaculatory emission from penis |
|
|
What is a vasectomy and how is it performed?
|
It is used for male contraception; the ductus deferens is found through palpation near the superficial inguinal ring and is amenable to surgical dissection/division - if bilateral, the patient is rendered sterile.
|
|
|
What is testicular torsion and how does it present?
|
It is the rotation of the testes about the spermatic cord, usually toward the penis (medial rotation); is a medical emergency because compression of testicular vessels results in ischemic necrosis within 6 hours - patients experience sudden excruciating scrotal pain
|
|
|
Describe the uterus.
|
Thick-walled muscular organ in midline; consists of body and cervix, joins with vagina inferiorly and superiorly has uterine tubes the project laterally towards adjacent ovaries
---where implantation of the blastocyst occurs and during pregnancy, uterus expands |
|
|
Describe the uterine tubes.
|
Extend from the body of the uterus to lateral pelvic wall and are enclosed within mesosalpinx portion of broad ligament
---has expanded trumpet shaped end (infindibulum) that curves around the ovary and has small fingerlike projections (fimbrae) to faciliate collection of ovulated eggs from ovary ---lumen opens into peritoneal cavity, has an expanded ampulla medially (where fertilization usually occurs) and narrows to form the isthmus before entering the uterus |
|
|
Describe the cervix.
|
Forms inferior part of the uterus, shaped like short, broad cylinder with narrow central channel; end is domed, bulges into vagina and gutter is formed around the margin of the cervix where is joins the vaginal wall
---external os: opening into the vagina ---internal os: opening into the uterus |
|
|
Describe the vagina.
|
Copulatory organ in women; distensible fibromuscular tube the extends from perineum to cervix; opens posterior to the external opening of the urethra
---forms vaginal fornix around the margin of the cervix ---canal is normally collapsed, with a widening near the uterus (vaginal vault); this is where semen is deposited during intercourse |
|
|
Describe the neurovascular supply of the female reproductive organs.
|
Blood supply:
---Arteries: internal pudendal supplies the clitoris, vaginal artery supplies the vagina, uterine artery supplies the uterus (anastomoses with ovarian artery/vaginal artery), ovarian artery supplies ovaries Innervation: ---Sympathetic: preganglionic - thoracic splanchnic (lesser/least) T10-12 and lumbar splanchnic L1-2; ganglia - aorticorenal (for ovaries)/pelvic (for all other reproductive organs); postganglionic - (ovaries) ovarian plexus/(all other) hypogastric plexus ---Parasympathetic: pelvic splanchnic nerves (S2-4) via hypogastric plexus |
|
|
What is an ectopic pregnancy and what is the usual location it occurs in?
|
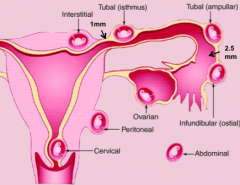
It is when the blastocyst implants in outside the uterus; this usually occurs in the ampulla of the uterine tube
|
|
|
What is the causal relationship between childbirth and incontinence? What are some treatment options?
|
The external urethral sphincter does not completely surround the urethra because the urethra fuses posteriorly with the anterior wall of the vagina; after childbirth, this space gets stretched even more, reducing the sphincter's ability to maintain closure
Treatments: |
|
|
Describe the development of the bladder and urethra.
|
Bladder:
---starts as primitive urogenital sinus, and forms during septation of the cloaca into bladder and rectum by the urorectal septum; from endoderm Urethra: caudal part of the UG sinus ---urachus: formed from the allantois as bladder/urethra formed; connects apex of bladder with umbilicus (becomes median umbilical ligament after birth) |
|
|
What are some defects that can occur in the urachus?
|
Persistence: should close after birth to become median umbilical ligament
---Lumen of allantois persists: can allow urine to leak from bladder ---Middle allantois persists: creates urachal cyst ---Upper allantois persists: creates urachal sinus |
|
|
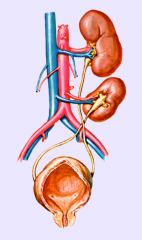
Describe which components of the kidney derive from the ureteric bud and which directly from intermediate mesoderm.
|
All of kidney is derived from intermediate mesoderm
---during 3-5 wks: three kidneys develop ---pronephros: cervical nephrotomes; vestigial excretory units (may not develop in humans); differentiate in 3rd wk, disappears at end of 4th wk ---Mesonephros: upper thoracic to L3 segments; differentiates in 4th wk, regresses in 8th wk ---Metanephros: kidney; differentiates in 5th wk; ureter buds off from mesonephric duct Excretory tubules form from intermediate mesoderm ---lengthen to form s-shaped loop, with capillary tuft forming a glomerulus ---tubules form Bowman's capsule around glomerulus and enter a longitudinal collecting duct (mesonephric duct) ---there is a cranial to caudal wave of mesonephric tubule formation followed by a wave of degeneration ---in females: disappears completely; males: mesonephric ducts/tubules become part of male reproductive tract Ureteric bud: kidney (metanephros) begins as bud; branches repeatedly to form the ureter, renal pelvis, calyces and collecting ducts ---accumulate a cap of *intermediate mesoderm* which become kidney tubules/nephrons ---through embryonic induction: metanephric tissue caps form nephrons - vesciles elongate to form s-shaped tubules that hook up to collecting ducts; capillaries grow out of distal end to form glomeruli; tubules develop features of mature nephrons (still ongoing at birth) |
|
|
Describe the movement of the kidneys and their subsequent vascularization
|
Kidneys shift cranially from pelvic region due to growth of the body in lumbar/sacral regions
---ascend towards suprarenal glands ---during ascent, kidneys are vascularized by series of arteries from aorta Renal arteries: accessory renal arteries derive from persistence of embryonic arteries that formed during ascent ---more common than accessory veins ---can obstruct ureter ---if accessory renal arteries are damaged/ligated, part of kidney can become ischemic |
|
|
Describe the suprarenal glands.
|
Derived from intermediate mesoderm adjacent to kidney and developing gonadal ridge
---coordinate stress response and metabolism ---fetal suprarenal cortes secretes hormones that maintain pregnancy (DHEA or diepihydrosterone) and regulate lung, liver, GI tract maturation and parturition ---neural crest cells migrate into medulla and differentiate into chromaffin cells (postganglionic sympathetic neurons that release epinephrine/norepinephrine) |
|
|
When are the kidneys functional?
|
By the 12th week
---urine is passed into amniotic cavity, mixes with amniotic fluid, which is swallowed by fetus and recylced through the kidneys |
|
|
Describe the role of primordial germ cells in gonad development.
|
Bilateral gonadal ridges form medial to mesonephric kidneys
---primordial germ cells (PGCs) migate from hindgut to gonadal ridges; are endodermal ---first appear among endoderm cells in wall of yolk sac close to allantois; migrate along dorsal mesentery to gonadal ridges in wk 5-6 ---gonads don't develop in PCGs fail to reach ridges Before and during arrival of germ cells, epithelium of ridges proliferate/invades underlying mesenchyme to form primitive sex cords ---cords are connected to surface epithelium |
|
|
Describe the role of mesonephric ducts in male development.
|

Mesonephric (Wolffian) duct:
---differentiates into male internal sexual structures ---SRY gene on Y chromosome endoces for sex-determining region Y called testes-determining factor (TDF), crucial for testes differentiation ---After PGCs migrate to gonadal ridges: 1a. cords of sertoli cells surround PGCs 2a. sertoli cells produce MIS (mullerian inhibiting substance) 3a. MIS causes regression of paramesonephric duct 1b. Leydig (interstitial) cells produce testosterone 2b. Testosterone allows mesonephric duct and adjacent tubules to persist TDF protein causes primitive sex cords to proliferate and form testis cords ---towards hilum, cords break up to form rete testis ---tunica albuginea separates testis cords from surface epithelium Mesonephric tubules become efferent ductules and mesonephric duct becomes epididymis and ductus deferens |
|
|
Describe the role of paramesonephric ducts in female development.
|
Paramesonephric (Mullerian) ducts:
---begins near cranial end of mesonephros as invagination of celomic epithelium and grows caudally adjacent to mesonephric duct ---cranially opening into the body cavity becomes the uterine tube ---differentiate into female internal sexual structures After PGCs migrate to gonadal ridges: 1. No leydig cells = no testosterone, which leads to the regression of mesonephric duct and tubules 2. No sertoli cells = no MIS, so paramesonephric duct persists Surface epithelium proliferates to form cortical cords; cords split into clusters that surround PGCs, which then develop into oogonia and cord cells into follicular cells ---paramesonephric ducts become uterine tube and uterus |
|
|
Describe the difference in the number of germ cells between males and females.
|
The number differs with age:
---females: germ cells develop (meiosis begins) in utero and numbers peak around 5 months (before birth) at 10^6; number decreases with age ---males: meiosis doesn't begin until puberty, after a burst of testosterone and the number increases with age |
|
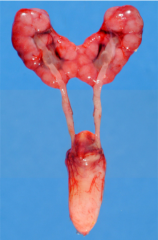
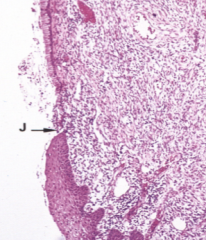
What congenital anomaly is this and what caused it?
|
Horseshoe kidney:
---fusion of the inferior poles of the kidneys during ascent ---can only rise until IMA because get caught ---occurs in 1/600 people |
|

What congenital anomaly is this and what caused it?
|
Bifed ureter:
---ureteric bud bifurcates before it enters the metanephric blastema ---can lead to urine blockage, infection or urinary stones |
|
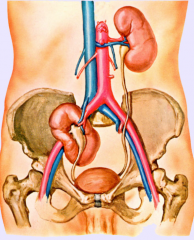
What congenital anomaly is this and what caused it?
|
Pelvic kidney:
---kidney doesn't ascend completely ---can lead to urine blockage, infection or urinary stones |
|
What congenital anomaly is this and what happened?
|
Ectopic kidney:
---a kidney crosses to the other side ---can lead to urine blockage, infection or urinary stones |
|
What congenital anomaly is this and what happened?
|
Thoracic kidney:
---kidney ascends to thorax ---can create urine blockage, infection or urinary stones |
|
|
What congenital anomalies can form during uterine development?
|
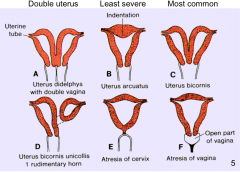
Septate/bicornate uterus:
---remnants of uterine septum Duplicated uterus: ---incomplete fusion of the paramesonephric ducts ---can either have double vagina or where one horn is rudimentary/non-functional Uterus arcuatus: ---indentation of fundus Atresia of cervix or vagina |
|
|
Describe the development of the vagina.
|
Develops as two evaginations from UG sinus, sinovaginal bulbs
---bulbs proliferate to form solid vaginal plate ---plate is canalized but lumen separated from UG sinus by thin tissue (hymen) ---endoderm ---expansions of vagina around uterus (fornices) are derived from paramesonephric ducts ---intermediate mesoderm |
|
|
Describe the development of the broad ligament.
|
Forms from the paramesonephric ducts as they unite in midline
|
|
Identify the genital tubercle, urogenital/urethral folds and genital swellings in an embryo at the indifferent stage. Specify the adult structures that each gives rise to in male/female.
|
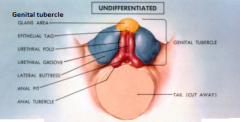
These differentiate into male/female genitalia under influence of hormones, such as testosterone
---all derived from intermediate mesoderm (with ectodermal covering) External genitalia are similar through wk 12 ---cloacal folds unite cranial to cloacal membrane to form genital tubercle and caudally are subdivided into urethral and anal folds ---in males: genital tubercle and urethral folds elongate to form shaft/glans of penis ---in females: genital tubercle becomes clitoris; urethral folds develop into labia minora ---genital swellings become scrotum (male)/labia major (female) |
|
|
Describe the formation of the penile urethra.
|
Fusion of urethral folds encloses portion of UG sinus in form penile urethra.
|
|

What congenital anomaly is this and what happened?
|
Hypospadias:
---results from failure of formation/fusion of urethral folds (penile hypospadias) or abnormal canalization of urethral plate within glans penis (glans hypospadias) |
|
|
Describe the development of male accessory glands.
|
Prostate, seminal vesicle and bulbourethral glands:
---they form off from the urethra ---prostate surrounds urethra, with ejaculatory duct passing through |
|
|
Describe the descent of the testes and the role of processus vaginalis.
|
Descent depends on several factors:
---degeneration of mesonephros and paramesonephric ducts ---enlargement of processus vaginalis ---shortening of gubernaculum Testes reach deep inguinal ring at 4 months, descend through inguinal canal to reach scrotum shortly before/after birth Processus vaginalis: ---develops lateral to inferior epigastric vessels and testes descend posterior to it ---creates tunica vaginalis (parietal/visceral layers) |
|
|
Describe the abnormal developments of the processus vaginalis.
|
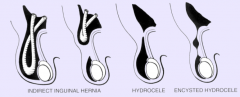
Indirect inguinal hernia:
---weakened area allows hernia into scrotal sac Hydrocele: ---fluid can build up in scrotum because vaginalis still connected to peritoneal cavity Encysted hydrocele: ---cyst develops in processus vaginalis |
|
|
What does Wnt4 do in females?
|
Anti-testes factors: actively inhibit differentiation into male
---from the somatic support cells in XX gonad ---helps maintain oocyte number |
|
|
What is the role of MIS, testosterone, 5-alpha reductase and dihydrotestosterone in males?
|
Sertoli cells produce MIS: cause paramesonephric (Mullerian) ducts to degenerate
5-alpha reductase converts testosterone into dihydrotestosterone, which leads to male development Dihydrotestosterone leads to development of: ---penis, scrotum, prostate Testosterone (produced by leydig cells) leads to development of: ---epididymis, ductus deferens, seminal vesicles; male brain differentiation ---after surge in puberty: maturation of seminiferous tubules, spermatogenesis and other pubertal changes ***present in males/females but only works in males*** |
|
|
Describe the development of the ovarian and round ligaments and the movement of the ovaries.
|
Ovaries descend partially, but do not enter labia majora; attached to body wall by suspensory ligament of ovary
Growth of uterus divides the inguinal ligament into ovarian ligament and round ligament |
|
|
Describe the anatomical and histological organization of the testis.
|
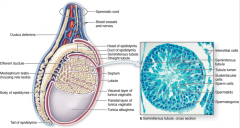
Histology:
---Each testis is surrounded by capsule of dense connective tissue (tunica albuginea); divided into lobules that contain seminiferous tubules surrounded by interstitial loose connective tissue and Leydig cells Anatomy: ---surrounded by derivative of peritoneal cavity, tunica vaginalis, which has visceral and parietal layers; also has pampiniform plexus of veins to moderate temperature ---outer fascial layers (internal to external): ---internal spermatic fascia: from transverse fascia of peritoneum ---cremasteric muscle: from internal abdominal oblique muscle; draws testes closer to body (temp regulation) ---external spermatic fascia: from external abdominal oblique muscle ---dartos: from scarpa's fascia; muscle portion moves testes away from body (temp regulation) ---skin |
|
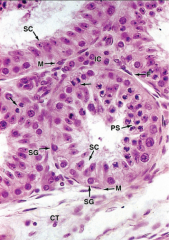
Identify the cells inside and outside the seminiferous tubule and describe the function of the seminiferous tubule.
|
Seminiferous tubules produce spermatozoa
Outside tubule: CT - connective tissue IC - interstitial (Leydig) cells: produce androgens (testosterone) M - myoid cells: contact to move sperm out of tubule F - fibroblasts Inside tubule: lined with specialized stratified epithelium SC - sertoli cells: form columnar epithlial lining, produce MIS, are germ cells of spermatogenic lineage SG - spermatogonia (always located near basement membrane) PS - primary/secondary spermatocytes: undergoing meiosis near lumen (can't differentiate between 1*/2*) |
|
|
Describe the sertoli cells.
|
Found in seminiferous tubules; nourish developing sperm, release protein-rich fluid into lumen to provide blood-sperm barrier, phagotize cytoplasmic residuals of spermatids
---when stimulated by FSH: ---produce and secrete ABP (androgen-binding protein) to stimulate spermatogenesis ---produce/secrete inhibin to inhibit FSH release ---activin to stimulate FSH release |
|
|
Describe spermatogenesis and spermiogenesis.
|
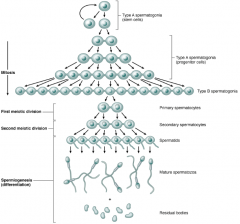
Spermatogenesis begins at puberty:
---starts with spermatogonium (primitive germ cell): gives rise to both new stem cells and type A spermatogonia (progenitor) ---type A spermatogonia undergo mitotic division to become type B spermatogonia, which undergo a final mitotic division to produce primary spermatocytes ---primary spermatocytes replicate their DNA and enter meiosis, becoming secondary spermatocytes after the first meiotic division (both spermatocytes are diploid) ---secondary spermatocytes undergo a second meiotic division and create spermatids (hapliod) Spermiogenesis: final stage of sperm production; no cell division ---formation of acrosome, condensation and elongation of nucleus, development of flagellum (middle piece gains mitochondria) and loss of most cytoplasm ---results in mature spermatozoa |
|
|
Describe Leydig cells.
|
Found in areas between the seminiferous tubules
---produce testosterone under influence of LH (aka ICSH - interstitial cell stimulating hormone) |
|
|
Describe the epididymis and its histology.
|

Receives sperm from testes, continuous with vas deferens
---store sperm in tail until ejaculation ---site where sperm fully mature and become motile Lumen is lined with pseudostratified epithelium with short basal cells (B) and taller principal cells (P) that have long microvili called stereocilia - absorb fluid; surrounded by smooth muscle (stimulated by sympathetic ns) |
|
|
Describe the ductus deferens and its histology.
|
Long tube with three layers of smooth muscle (Inner/Outer - longitudinal/ middle - Circular)
---receive sympathetic stimulation for ejaculation Epithelial lining is pseudostratified, with shorter principal cells; folded to allow expansion during ejaculation |
|
|
Describe the seminal vesicles and their histology.
|
Have very convoluted tubule structure with folded lumen epithelium; surrouned by tough capsule with double layer of smooth muscle (outer - longitudinal/inner - circular)
---receives sympathetic stimulation for ejaculation Epithelium is simple cuboidal/low pseudostratified |
|
|
Describe the prostate gland, its histology and its problem regions.
|

Surrounded by fibrous capsule with thick fibromuscular septum; has two lobes each with dozens of branching tubular glands lined with folded epithelium
---stroma consists of tough collagen with irregular smooth muscle Epithelium is pseudostratified cuboidal to columnar, with loose connective tissue lamina propria Composed of three zones: ---transitional zone: surrounds proximal urethra (transitional epithelium) ---rarely cancerous but is primarily responsible for benign prostatic hypertrophy (BPH), caused by proliferation of cells and enlarges prostate, which occludes the urethra and can push into bladder (bladder may hypertrophy from strain of urination) ---central zone: surrounds ejaculatory ducts, partially surrounds transitional zone ---also indicated in BPH ---peripheral zone: largest, outer zone ---makes up 75% of all cancers |
|
|
Describe the bulbourethral glands and their histology.
|
Pea-sized, composed of tubular glands which ducts converge on single duct; cells are simple columnar
---divided into lobules by fibromuscular septum |
|
|
Describe the histology of erectile tissue and the mechanism of an erection.
|
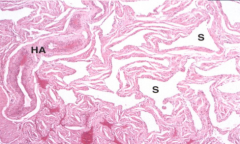
Tissue: variably-shaped endothelium-lined spaces (S-sinusoids) that receive blood from dorsal/deep arteries, which have branches that penetrate to form capillary plexuses or (HA) helical arteries
---in males, composed of corpus cavernosa and corpus spongiosum surrounding urethra ---in females, bulb of vestibule and corpora deep to ischiocavernosus muscle are same erectile tissue Mechanism: stimulated by parasympathetic ns via pelvic splanchnic ---helicine arteries and capillary plexuses from dorsal/deep arteries engorge sinusoids and crimp veins so no drainage of blood ***ejaculation: sympathetic ns stimulates movement of sperm; somatic (pudendal n.) stimulates projectile ejaculation*** |
|
|
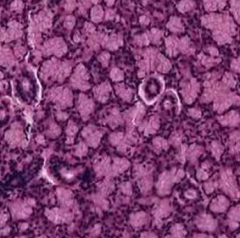
Describe the histological organization of the ovary.
|
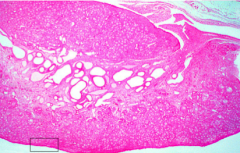
Covered by peritoneum (broad ligament) made of simple cuboidal (usually simple squamous in other peritoneal linings) called germinal epithelium
---deep to epithelium is connective tissue layer, tunica albuginea Have outer cortex (contains oocytes) and inner medulla (contains blood vessels, nerves, lymph) |
|
|
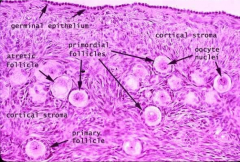
Describe the development of the ovarian follicle.
|

Two separate processes: oogenesis and folliculogenesis
---Before birth: ---1a. Oogonium (stem cell) undergoes mitosis to become primary oocyte and is arrested in prophase I at birth ---1a. Primordial follicle surrounds primary oocyte --After puberty: ---1b. Primordial follicle develops into primary follicle and continues growing ---1b. Primary oocyte still arrested in prophase I ---2b. Oocyte completes meiosis I every month to become secondary oocyte; unless fertilized, remains arrested in metaphase II ---2b. Graafian (vesicular) follicle develops around secondary oocyte; oocyte is ovulated, breaking out of follicle ---3b. If sperm penetrates, meiosis II occurs, creating the ovum (with three final polar bodies) ***many (10-30) oocyte/follicles start the maturation process every month, but only one completes it months later*** |
|
|
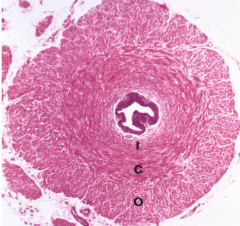
Describe the follicular changes that occur during oocyte development.
|
Primordial follicle (primary oocyte): simple squamous epithelium
Primary follicle (primary oocyte): simple cuboidal epithelium becoming stratified Secondary follicle (primary oocyte): stratified cuboidal epithelium develops antra (fluid-filled spaces) Tertiary follicle (secondary oocyte): merger of antra, eccentric oocyte selected to continue through meiosis Corpus luteum: develops from remnant of follicle cells after oocyte emerges; biochemically active |
|
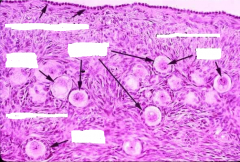
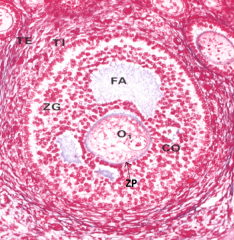
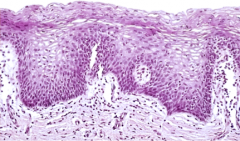
Identify the cells in this slide.
|
|
|
|
Describe the formation of the zona pellucida.
|
Oocyte produces glycoproteins that form a layer between the oocyte and granulosa cells (follicle); microvilli from oocyte and filopodia from granulosa grow into zona pellucida to form gap junctions for communication
|
|
|
Describe the formation of the stroma and the production of its cells and the granulosa cells.
|
Stroma forms theca folliculi, theca externa and collagen and smooth muscle
---theca externa: produces androgen (androstenedione) ---granulosa (follicle) cells: produce estrogen/estradiol FA - follicular antrum O1 - primary oocyte TE - theca externa TI - theca interna/folliculi ZG - granulosum ZP - zona pellucida |
|
|
Describe the difference between primary and secondary oocytes and the types of follicls they are found.
|
Primary oocyte: has gone through mitosis and is arrested in prophase I
---can be found in any of the following: ---primordial follicle, primary follicle, growing follicle and secondary follicle Secondary oocyte: has undergone meiosis I and is arrested in metaphase II ---found in tertiary (Graafian/vesicular) follicle |
|
|
How long are the processes of oogenesis and folliculogenesis?
|
Take place over approximately 1 year
---initial growth phase of 10-30 primordial follicles is extremely slow; can take 8-10 months for primary to become seconday follicle ---change becomes much more swift, until only one oocyte continues through meiosis I and into meiosis II Ovary will have populations of follicles in all stages of transformation |
|
|
Describe the formation and function of the corona radiata.
|
Follicular antrum increases in size and oocyte becomes more eccentric, detaching from surrounding granulosa with halo of cells (corona radiata)
---antrum continues to increase in size until it spans the cortex and pushes against the tunica albuginea Function: ---to protect oocyte and block sperm penetration |
|
|
Describe the process of ovulation.
|
LH and ovarian protease and cytokines weaken an area called the stigma
---at ovulation, oocyte and corona radiata are ejected through weakened tunica albuginea and epithelial covering ---will hopefully be grabbed by fimbrae and pulled into oviduct |
|
|
Describe the formation and function of the corpus luteum.
|
After ovulation, stigma heals over and remaining follicular/thecal cells form corpus luteum
---produces progesterone and estrogen (under influence of LH) ---if implantation takes place, will remain active for 3+ months ---no implantation, starts degenerating after two weeks ---eventually becomes corpus albicans (scar tissue) |
|
|
Describe the uterine tube and its histology.
|
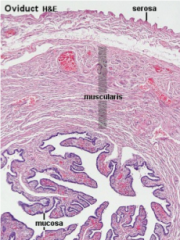
Has three layered structure:
---folded mucosa with ciliated epithelium and lamina propria ---epithelial cells: simple columnar; ciliated cells beat to move oocyte/zygote towards uterus; non-ciliated cells (peg cells) produce nutritive fluid ---muscularis ---may act like sphincter at junction with uterus ---serosa (peritoneum) covering Lumen gets progressively smaller (infundibulum > ampulla > isthmus), mucosa becomes less complicated and muscularis becomes thicker |
|
|
Describe the histological structure of the uterus.
|
Three layers: lumen lined by simple columnar
---endometrium: inner layer; ---stratum basale: next to myometrium, more or less permanent ---stratum functionalis: outer layer; shed monthly during menses ---Two layers: stratum compactus (outer) and stratum spongiosum (inner) ---myometrium: muscular inner layer; multi-layered (stratum muscularis) ---serosa: broad ligament (inferiorly just adventitia) |
|
|
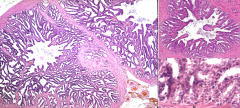
Describe how the structure of the uterus changes during the menstrual cycle.
|
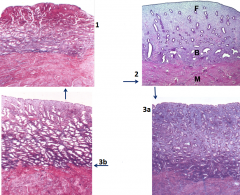
1. Menstrual phase: during first 4-5 days of uterine cycle when the stratum functionalis is shed
2. Proliferative phase: uterus builds itself back up in days 5/6 -14; vessels and glands in basal layer grow into expanding functionalis 3. Luteal/secretory phase: (3a) functionalis develops glands which produce glycogen/glycoprotein secretions in days 15-28; glands start as straight tubes, (3b) then become helical and "saw-toothed" during end of phase 4. If implantation does not occur, cycle starts over |
|
|
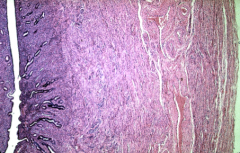
Describe the histological structure of the cervix.
|
Cervix extends into vagina
---lumen: made of mucous secreting simple columnar cells ---junction (transformation zone): abrupt change into stratified squamous cells of vagina ---often site where papilloma virus enters; can lie dormant or may immediately affect cells |
|
|
Describe the histological formation of the vagina.
|
Fibromuscular canal with three layers:
---stratified squamous epithelial mucosa ---produces glycogen which is anaerobically broken down by bacteria to form lactic acid; pH of vagina is 3.5-4.5 (important defense mechanism) ---muscularis ---adventitia |
|
|
Describe the structure of the female breast.
|
Have varying amounts of fatty and fibrous connective tissue
---some fibrous tissue is organized into dense strands (suspensory ligaments) ---originate from epimysium of platysma and pectoral muscles and run between lobes to attach to dermis ---fibrous tissue also surrounds lobes, with the fat dispersed cutanously around the lobes ---amount of glandular tissue is similar in all women; size varies by amount of adipose tissue Divided into 15-25 lobes, which have their own ducts and may converge before reaching the nipple; there are 4-20 lactiferous openings in the nipple ---then divide into lobules, which are formed from clusters of alveoli ---alveoli have a common, central duct and are formed by cells that produce milk |
|
|
Describe the changes that occur in a lactating breast and identify the histological differences between a lactating and non-lactating breast.
|
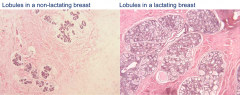
Breasts respond to cyclic release of estrogen, which acts on ducts, and progesterone, which acts on alveoli
---ducts and alveoli enlarge and surrounding tissues become edematous If implantation occurs, alveolar cells increase, ducts grow and branch and more alveoli develop ---estrogen/progesterone are important in regulating breast development along with prolactin/other hormones including lactogen from placenta and glucocorticoids from adrenal Late in pregnancy: alveoli produce colostrum, protein-rich with vitamin A electrolytes and antibodies ---first "milk" secreted after birth ---milk produced both by merocrine (protein portion) and apocrine (lipid) secretions Ducts change from stratified cuboidal to columnar around ovulation Oxytocin from neurohypophysis is important in stimulating the myoepithelium around the alveoli/ducts to release and propel milk |

