![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
Name the bones of the lower extremity.
|
Os coxae (pelvis): ilium, ischium, pubis; Femur; Patella; Tibia; Fibula; Tarsals: talus, calcaneus, navicular, cuboid, lateral cuneiform, intermediate cuneiform, medial cuneiform; Metatarsals; Phalanges (proximal, middle, distal)
|
|
|
Describe the structure and movements of the hip joint.
|
Multiaxial ball and socket joing formed from the head of the femur and the acetabulum in the pelvis (where 3 bones fuse); is a synovial articulation, with the membrane extending down to the neck of femur.
Designed form stability and weightbearing at expense of mobility. Acetabulum almost entirely covers head to provide stability and has a cartilaginous collar (labrum) as well as the ligament of the head of femur which attaches from the fovea in the femur to the acetabular fossa; three ligaments reinforce/stabilize joint: iliofemoral (anterior), pubofemoral (anteroinferior), and ischiofemoral (posterior). Movements:flexion/extension, abduction/adduction, medial/lateral rotation, circumduction |
|
|
Describe the structure and movements of the knee joint.
|
Largest synovial joint in body; articulation between femur and tibia, femur and patella. Two menisci (fibrocartilaginous) attach to tibia to provide cushion between bone. Synovial membrane surrounds the articular cavity and the fibrous membrane encloses synovium and is reinforced by ligaments and tendons of muscles.
Major ligaments: ---patellar ligament: extension of quadriceps femoris (below patella) ---Collateral ligaments: stabilize hinge movement, prevent side to side -------fibular (lateral) collateral ligament: attached to lateral femoral epicondyle and fibular head -------tibial (medial) collateral ligament: attached to medial epicondyle and tibia ---Cruciate ligaments: --------Anterior cruciate ligament: attached to anterior tibia and posterior (lateral) femur to prevent femur from sliding back --------Posterior cruciate ligament: attached to posterior tibia and anterior (medial) femur to prevent femur from moving forward. Movements: flexion/extension |
|
|
Describe the structure and movements of the ankle joint.
|
Synovial: involves talus, tibia and fibula; articular surfaces covered by hyaline cartilage and cavity enclosed by synovial membrane and then fibrous membrane. Most stable when dorsiflexed.
Ligaments: ---Medial ligament (4 parts): from medial malleolus to tarsals; tibionavicular, tibiocalcaneal, posterior tibiotalar, anterior tibiotalar ---Lateral ligament (3 parts): from lateral malleolus to tarsals; anterior talofibular, posterior talofibular, calcaneofibular Movement: dorsiflexion/plantarflexion |
|
|
Name the gluteal muscles, their function and innervation and blood supply.
|
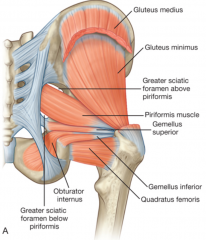
---Piriformis: laterally rotates extended femur at hip; abducts flexed femur at hip (branches from L5-S2)
---Obturator internis: laterally rotates extended femur at hip; abducts flexed femur at hip (nerve to obturator internis (L5-S1)) ---Gemellus superior: laterally rotates extended femur at hip; abducts flexed femur at hip (nerve to obturator internis (L5-S1)) ---Gemellus inferior: laterally rotates extended femur at hip; abducts flexed femur at hip (nerve to quadratus femoris (L5-S1)) ---Quadratus femoris: laterally rotate femur at hip (nerve to quadratus femoris (L5-S1)) ---Gluteus minimus: abducts femur at hip; holds pelvis secure over stance leg, prevents hip drop during gait; medially rotates thigh (superior gluteal nerve (L4-L5)) ---Gluteus medius: abducts femur at hip; holds pelvis secure over stance leg, prevents hip drop during gait; medially rotates thigh (superior gluteal nerve (L4-L5)) ---Gluteus maximus: powerful extensor of flexed femur at hip; lateral stabilizer of hip and knee; laterally rotates/abducts thigh (inferior gluteal nerve (L5-S1)) ---Tensor fascia latae: stabilizes knee in extension (superior gluteal nerve (L4-L5)) Vasculature: ---Arteries: inferior gluteal and superior gluteal (superficial/deep) ---Veins: follow arteries, going to femoral vein |
|
|
Name the muscles of the anterior compartment of the thigh, their functions and innervations and blood supply.
|
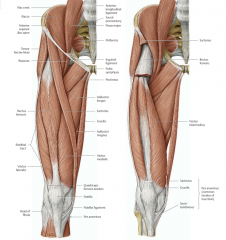
Hip Flexors:
---Psoas major: flexes thigh at hip (anterior rami (L1-L3)) ---Iliacus: flexes thigh at hip (femoral nerve (L2-L3)) ---Quadriceps femoris (4) ------Vastus medialis: extends leg at knee (femoral nerve (L2-L4)) ------Vastus intermedius: extends leg at knee (femoral nerve (L2-L4)) ------Vastus lateralis: extends leg at knee (femoral nerve (L2-L4)) ------Rectus femoris: flexes thigh at hip and extends leg at knee (femoral nerve (L2-L4)) ---Sartorius: flexes thigh at hip and flexes leg at knee (femoral nerve (L2-L3)) Vasculature: ---Arteries: Femoral artery, deep artery of thigh, lateral/medial circumflex femoral arteries, perforating arteries, obturator artery ---Veins: Great saphenous vein to femoral vein |
|
|
Name the muscles of the medial compartment of the thigh, their functions and innervations and blood supply.
|
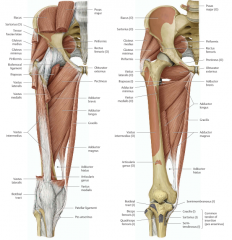
Hip Adductors:
---Gracilis: adducts thigh at hip and flexes leg at knee (obturator nerve (L2-L3)) ---Pectineus: adducts and flexes thigh at hip (femoral nerve (L2-L3)) ---Adductor longus: adducts and medially rotates thigh at hip (obturator nerve (L2-L4)) ---Adductor brevis: adducts thigh at hip (obturator nerve (L2-L3)) ---Adductor magnus: adducts and medially rotates thigh at hip (adductor part: obturator nerve (L2-L3); hamstring part: tibial nerve (L2-L4)) ---Obturator externus: laterally rotates thigh at hip (obturator nerve (L3-L4)) Vasculature: ---Arteries: femoral artery, deep artery of thigh, lateral/medial circumflex arteries, perforating arteries, obturator artery ---Veins: great saphenous vein (from foot) to femoral vein |
|
|
Name the muscles of the posterior compartment of the thigh, their functions and innervations and blood supply.
|
Knee Flexors:
---Biceps femoris: (long head) flexes leg at knee; (short head) extends and laterally rotates thigh at hip and laterally rotates leg at knee (sciatic nerve (L5-S2)) ---Semitendinosus: flexes leg at knee and extends thigh at hip: medially rotates thigh at hip and leg at knee (sciatic nerve (L5-S2)) ---Semimembranosus: flexes leg at knee and extends thigh at hip: medially rotates thigh at hip and leg at knee (sciatic nerve (L5-S2)) Vasculature: ---Arteries: femoral artery, deep artery of thigh, lateral/medial circumflex arteries, perforating arteries, obturator artery ---Veins: great saphenous vein (from foot) to femoral vein |
|
|
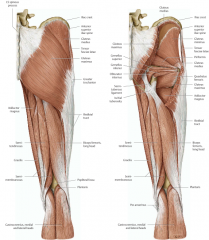
Name the muscles in the anterior compartment of the leg, their functions and innervations and blood supply.
|
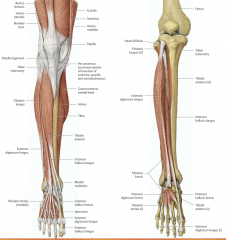
Ankle dorsiflexors:
---Tibialis anterior: dorsiflexion of foot at ankle, inversion of foot; dynamic support of medial arch (deep fibular nerve (L4-L5)) ---Extensor hallicus longus: extension of great toe and dorsiflexion of foot (deep fibular nerve (L5-S1)) ---Extensor digitorum longus: extension of lateral toes and dorsiflexion of foot (deep fibular nerve (L5-S1)) ---Fibularis tertius (variable): dorsiflexion and eversion of foot (deep fibular nerve (L5-S1)) Vasculature: ---Arteries: Anterior tibial artery becomes anterior medial/lateral malleolar arteries ---Veins: deep veins follow arteries |
|
|
Name the muscles in the lateral compartment of the leg, their functions and innervations and blood supply.
|
Primary evertors, weak plantarflexion:
---Fibularis longus: eversion and plantarflexion of foot; supports latera/transverse arches (superficial fibular nerve (L5-S2)) ---Fibularis brevis: eversion of foot (superficial fibular nerve (L5-S2)) Vasculature: ---Arteries: no major arteries pass through, supplied by branches of fibular artery ---Veins: deep veins follow arteries |
|
|
Name the muscles in the posterior compartment of the leg, their functions and innervations and blood supply.
|

Ankle plantarflexors:
---Superficial group: ------Gastrocnemius: plantarflex foot and flex knee (tibial nerve (S1-S2)) ------Plantaris: plantarflex foot and flex knee (tibial nerve (S1-S2)) ------Soleus: plantarflexes foot (tibial nerve (S1-S2)) ---Deep group: ------Popliteus: stabilizes knee (resists lateral rotation of tibia); unlocks knee (laterally rotates femur on tibia) (tibial nerve (L4-S1)) ------Flexor hallicus longus: flexes great toe (active during push off of gait) (tibial nerve (S2-S3)) ------Flexor digitorum longus: flexes lateral toes (tibial nerve (S2-S3)) ------Tibialis posterior: inversion and plantarflexion of foot; support of medial arch (tibial nerve (L4-L5)) Vasculature: ---Arteries: popliteal artery (sural arteries branch off to supply superficial), anterior tibial artery (supplies anterior), posterior tibial artery (supplies lateral/posterior) and branches into circumflex fibular artery (anastomotic for knee) and fibular artery has a perforating branch that anastomoses with anterior tibial artery ---Veins: deep veins follow arteries |
|
|
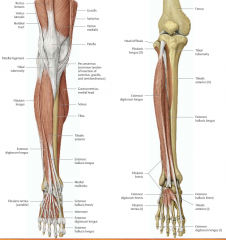
Describe the normal cutaneous innervation of thigh and leg (5 key areas).
|
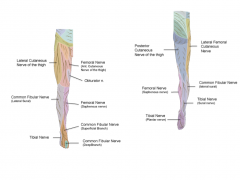
---Obturator nerve: skin over upper medial aspect of thigh (touch medial thigh)
---Femoral nerve: skin over anterior thigh, antermedial knee, medial leg and foot (touch medial malleolus) ---Tibial (sural) nerve: skin on posterolateral side of lower leg, lateral ankle, foot and little toe and sole of foot and toes (touch lateral malleolus) ---Superficial fibular nerve: skin on dorsal foot and toes except for between great and second toes (touch dorsum of foot) ---Deep fibular nerve: skin between great and second toes (touch between first two toes) |
|
|
What is Deep Vein Thrombosis (DVT), where is usually located and what are the consequences?
|
It is a blood clot with in the deep veins of the lower limb and can lead to pulmonary embolus. It is caused by venous stasis, hypercoagulation or endothelial damage to the vein, which cause blood to stagnate behind the cusp of a venous valve. Will present with swelling, decreased blood flow and possibly sharp chest pain exacerbated by deep breathes.
|
|
|
What are varicose veins and how are they formed? What is a common treatment?
|
They are veins that have an abnormal pooling of blood in them due to incompetent valves that allow backflow of blood into superficial veins; they look swollen, twisted and can be painful.
Treatment: usually conservative; try to avoid long bouts of standing, wear supportive hose, raise legs when resting/sleeping; if extremely painful, can do surgery. |
|
|
What is compartment syndrome in the leg and what is the anatomical basis? How is it treated?
|
It is an increase in the interstitial fluid pressure within a compartment within the leg that compromises circulation and leads to ischemia (muscle/nerve damage). Signs include swollen, tense compartment; pink color, warmth and pulse over compartment. This is caused by the thick layer of fascia that separates each compartment; fascia does not expand, so the pressure cannot be released.
Treatment: Fasciotomy: cuts are made into the fascia of the affected compartment and the fluid is allowed to drain to relieve pressure. |
|
|
Describe the pathophysiology of osteoarthritis and its clinical signs and symptoms. What are the differences from rheumatoid arthritis?
|
It is a result from aging, as well as wear and tear on a joint, along with a host of other things such as genetics, mechanics and biology, and as cartilage breaks down/wears away, bones rub together.
Signs and symptoms: Joint swelling, with cracking sound during movement, normal movement is painful, limited range of motion and joint tenderness. Rheumatoid arthritis: leads to inflammation of joint, is an autoimmune disease, and affects both joints on both sides of body equally |
|
|
Describe the events that occur at the hip, knee and ankle during the three major phases of the human gait.
|
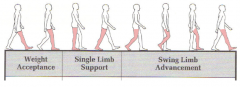
Weight Acceptance: period when weight is rapidly loaded onto limb
---Hip: slightly flexed, hip extensors/abductors are active (eccentric contraction) ---Knee: slightly flexed, quadriceps are active (eccentric contraction) ---Ankle: progressing towards plantarflexion, dorsiflexors active (eccentric contraction) Single Limb Support: period when body progresses over weight bearing limb ---Hip: progresses to extension; initially hip abductors active, then nothing as center of mass moves in front of hip helping to extend it ---Knee: maintains slight flexion; quadriceps initially active, then nothing as center of mass moves in front of knee helping to extend knee ---Ankle: progresses to dorsiflexion; plantarflexors are active (eccentric contraction) Swing Limb Advancement: period when limb is unloaded and swings from behind body to in front of body ---Hip: Flexes; initally hip flexors active, then hamstrings take over (eccentric contraction) and hip adductors active to keep limb close to center ---Knee: Flexes; initially knee flexors active, then quadriceps are active as move towards full extension/heel strike ---Ankle: Plantarflexion moving to neutral ankle; dorsiflexors are active |
|
|
Describe what happens when the superior gluteal nerve is injured; what is the altered gait called?
|
If the superior gluteal nerve is injured, the pelvis drops over the swinging limb; called Trendelenburg's sign, when patient stands on affected side, pelvis tilts inferiorly on opposite side and patient compensates by lurching trunk to affected side to maintain level pelvis
|
|
|
What are the strength tests for the knee?
|
Knee Extensors (quadriceps)/Flexors (hamstrings): test in seated position, knees bent; extend/flex knee against resistance and compare
|
|
|
What are the special tests for the knee?
|
Anterior Knee Pain:
---patellar apprehension test: ------apply firm, laterally directed force toward medial aspect of patella (positive test: apprehension/implies preceding episode of patellar dislocation) ---Patellofemoral grind test: ------knees extended, place thumb on patella, have patient contract quadriceps while pushing downward on patella (positive: pain with movement, or unable to complete test) Ligaments: ---Assess stability; abnormal test=excessive motion ---Valgus stress test (MCL): stabilize thigh and laterally direct ankle to open knee joint on medial side (positive: significant gap on medial side) ---Varus stress test (LCL): stabilize knee and push ankle medially, open knee joint on lateral side (positive: gap on lateral side) ---Lachman test (ACL): stabilize thigh and attempt to move tibia forward (positive: excessive forward motion) ---Anterior Drawer test (ACL): bend knee, sit on foot and pull knee forward (positive: excessive forward motion of tibia)---less sensitive than Lachman's ---Posterior Drawer test (PCL): bend knee, push tibia posteriorly (positive: increase tibial posterior movement) ---Medial/Lateral Meniscus: flex knee (positive: pain) |
|
|
Describe how a muscle fiber is organized in terms of its connective tissue.
|
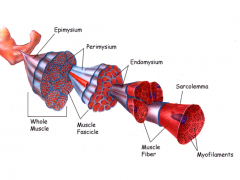
---Epimysium (deep fascia): dense connective tissue that surrounds the entire muscle
---Perimysium: connective tissue that surrounds group of fibers that form fascicle; conveys large blood vessels and nerves into muscle ---Endomysium: delicate connective tissue that surrounds individual fibers |
|
|
Describe the characteristics of a skeletal muscle cell.
|
---Myofibrils are multinucleated cells surrounded by continuous plasma membrane (sarcolemma), which is in turn surrounded by a basal lamina and satellite cells.
---The sarcolemma has finger-like projections into the cytoplasma called T-tubules. ---Running alongside the tubules and the muscle is the sarcoplasmic reticulum, which is a membraneous sac that stores calcium in its terminal cisternae. |
|
|
Describe the sliding filament model.
|

A Sacromere is the basic function unit of the myofibril. It is composed of thick and thin filaments that work together with each other and other sarcomeres to move muscle.
---During contraction, the thick filaments move along the thin, decreasing the length of the sarcomere (reduction in I/H bands); the length of the filaments does not change ---The force (tension) generated during contraction pulls the ends towards each other |
|
|
Describe how energy is converted to mechanical force during muscle contraction.
|
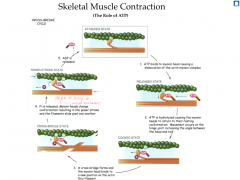
ATP plays an essential role in the contraction and release of the myosin head of the thick filament from the binding site on the thin filament.
|
|
|
Describe the role of calcium in muscle contraction.
|
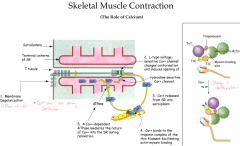
Calcium is needed to change the conformation of the thin filament in order to allow the myosin head to bind to the myosin binding site.
---Calcium is released from the sarcoplasmic reticulum when the membrane is depolarized and it binds to the troponin complex of the thin filament, facilitating actin-myosin binding |
|
|
Identify histological components of a peripheral nerve and ganglion.
|
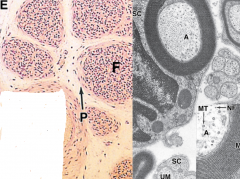
Ganglion is a collection of many axons; peripheral nerves are surrounded by connective tissue sheaths like muscle fibers
---Epineurium: surrounds entire nerve ---Perineurium: surrounds nerve fiber bundles (fascicles) ---Endoneurium: surrounds individual nerve fibers outside myelin sheath |
|
|
Describe the structure and function of the motor end plate.
|
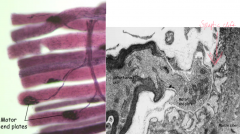
It is where the axon interacts with a muscle fiber; the motor plate releases acetylcholine that binds to receptors that cause membrane depolarization.
---Synaptic clefts are where the infoldings of the sarcolemma interact associate with the axon terminal. |
|
|
What is a motor unit and how does it differ between fine and gross motor control?
|
It is that axon and all the fibers that that axon innervates.
---Muscles that require fine motor control have fewer fibers per motor unit (small motor units) ---Large muscles used for gross/powerful movements have several hundred fibers per motor unit (large motor units) |
|
|
Describe the structure and function of a muscle spindle.
|

Muscle spindles are found within the belly of muscles and run parallel with the main muscle fibers; it senses muscle length and changes in length
---If a muscle is stretched, the spindle cause the stretching muscle to contract and the antagonistic muscle to relax |
|
|
Describe the structure and function of the golgi tendon organ.
|
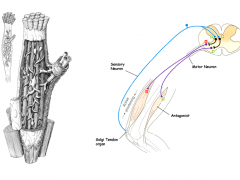
Golgi tendon organs lie within tendons near muscle-tendon junctions and measure the force generated by a muscle by measuring the tension in its tendon; prevents over-contraction of a muscle
---It inhibits the contracting muscle and stimulates the antagonistic muscle to counteract the over-contraction |
|
|
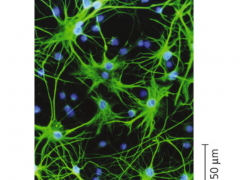
Describe the basic structure of a neuron.
|

A neuron is responsible for the transmission of impulses
---generally lose ability to divide after differentiation Composition: ---Cell Body (perikaryon): includes the nucleus and cytoplasm of neuron; receives impulses (+/-) from other neurons; rough endoplasmic reticulum is prominent (Nissl bodies) ---Dendrites: (input portion) short branches from the cell body; receive nerve impulses from other neurons; involved with neuronal plasticity (through interaction with other dendrites) ---Axon: (output portion) usually one per neuron (can be very long); originate from swelling called axon hillock; has bidirectional transport and forms synapses with other neurons, muscle cells and gland cells Morphology: ---Multipolar: one axon and several dendrites (most are) ---Bipolar: one axon and one dendrite (retina, olfactory mucosa, and cochlea of inner ear) ---Unipolar/pseudounipolar: one process coming off perikaryon (spinal ganglia such as DRG and most cranial ganglia) |
|
|
Describe the structure and function of an astrocyte.
|
It is a neuroglial cell that has processes that physically interact with blood vessels to regulate local blood flow in the CNS; regulates micro-environment of neurons by scavenging ions, neurotransmitters and metabolites; may also play a role in formation of scar tissue in response to CNS injury
|
|
|
Describe the structure and function of ependymal cells.
|
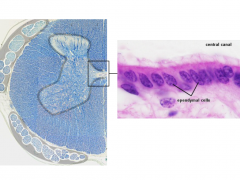
They are neuroglial cells that line the fluid-filled (CSF) cavities of the brain and spinal cord; play a role in production, transport and circulation of CSF
---have cilia to facilitate movement |
|
|
Describe the structure and function of oligodendrocytes and schwann cells.
|
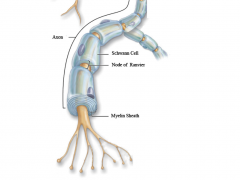
Both are neuroglial cells that wrap tightly around axons to form the myelin sheath; oligodendrocytes are found in the CNS and schwann cells are found in the PNS
---myelin sheath protects and insulates axons, maintains their micro-environment and enables them to regenerate and re-establish connection with receptors/effectors ---increase speed of electrical signal travelling down axon through nodes of ranvier |
|
|
Describe the structure and function of satellite cells.
|

They are neuroglial cells that surround cell bodies of neurons in ganglia; are modified schwann cells and their role is to maintain the micro-environment and provide insulation for the ganglion cells
|
|
|
Describe the development of the skull.
|

Skull is formed from two parts:
---Neurocranium: surrounds the brain; derived from neural crest cells (exception) and paraxial mesoderm ------flat bones develop via intramembranous ossification ------skull base develops via endochondral ossification ---Viscerocranium: composes the face bones; derived from neural crest cells in pharyngeal arches (except laryngeal cartilage which is from mesoderm) ------most is formed by intramembranous ossification Pink: intramembranous ossification (neural crest cells) Dark blue: endochondral ossification (mesoderm) |
|
|
What is the significance of sutures and fontanelles?
|
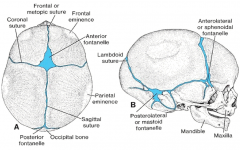
Fontanelles are where sutures meet and sutures allow the flat bones of the skull to deform during childbirth and expand during childhood
---Anterior fontanelle: closes around 18-24 months ---Posterior fontanelle: closes around 3-6 months ---Mature suture closure: around 12 years and complete fusion can continue until 30s |
|
|
What are some common developmental defects that can occur during skull development?
|
---Cranioshisis: Failure of the cranial neuropore to close, which results in failure of the cranial vault to form and the brain is eroded by amniotic fluid (fatal)
---Craniosynostosis: premature closure of one or more sutures; 1/2500 births; results in head asymmetries (most common in the sagittal suture (scaphocephaly) leading to a narrow, elongated football-like shape to the skull) |
|
|
Describe the step of limb development.
|

Limb development is an example of embryonic induction; upper limb buds appear first, lower limbs second
---Initiation begins at ~4 weeks from the lateral plate mesoderm ------intermediate mesoderm produces FGF8, which induces FGF10 in lateral plate mesoderm, which induces the ectoderm to form AER, which produces FGF8 and FGF4, which in turn maintain FGF10 ---AER promotes outgrowth of limb bud ---ZPA regulates the development of the limb bud along the cranial/caudal axis (differentiates thumb from pinkie) |
|
|
What is the apical ectodermal ridge and what role does it play in limb development?
|

AER is a ridge of thickened cells along the outer edge of the limb bud and it interacts with the underlying cells to promote outgrowth of the limb bud along the proximal/distal axis
---maintains proliferation of underlying mesenchyme (progress zone) through production of FGF8/FGF4 ---as limb elongates, cells leave progress zone and are no longer under the influence of AER; cells stop dividing and differentiate into cartilage and bone (moves from proximal to distal pattern) Cell Death: ---selective loss of AER facilitates formation of digits through apoptosis (programmed cell death) ---loss of AER reduces amount of FGF in the interdigital spaces, leading to cell death and cessation of cell proliferation in these areas |
|
|
What is the zone of polarizing activity (ZPA) and what is its role in limb development?
|
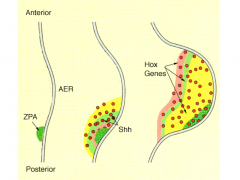
ZPA is a specialized mass of cells in the base of the limb bud that regulates development along the cranial/caudal axis
---induced by FGF8 from AER and helps to maintain structure/function of AER through production of Sonic hedgehog (Shh) ---Shh establishes gradient of Homeobox (Hox) gene expression across the developing limb and defines the pattern of differentiation from the thumb to the pinkie ------transplantation of the ZPA/implantation of Shh to anterior limb bud results in formation of extra digits (polydactyly) |
|
|
How and where does intramembranous ossification occur?
|
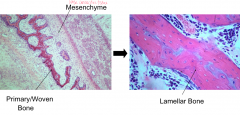
Location: involved in the formation of the flat bones of the skull and bones of the face
Development: mesenchyme cells differentiate into osteoblasts and produce primary/woven bone; the woven bone is then remodelled into lamellar bone |
|
|
How and where does endochondral ossification occur?
|

Location: involved in the formation of long bones, vertebral column, pelvis, sternum and base of skull
Development: mesenchyme cells differentiate into chondroblasts, which produce a cartilage model of future bone ---cartilage becomes vascularized and is replaced by bone matrix ---cartilage remains on surface of epiphysis as articular cartilage and in epiphyseal plate, regulating growth in length |
|
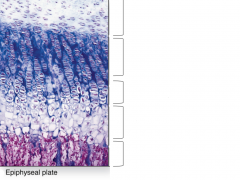
What is the epiphyseal plate and what are its histological layers?
|
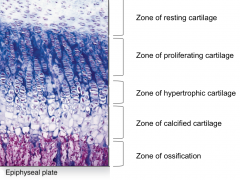
It is a cartilagenous structure near the end of bones that is responsible for the growth in length of long bones
---proliferation occurs at epiphyseal side and replacement by bone occurs at the diaphyseal side ---epiphyseal plate remains the same width and bone continues to grow as long as rate of cell division equals rate of cell death/ossification ---stays active until ~20yrs |
|
|
Describe the development of skeletal muscle.
|
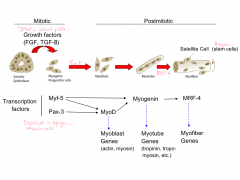
Paraxial mesoderm is organized into segments (somitomeres) most of which eventually condense into somites; somites differentiate into sclerotome (bone), myotome (muscle) and dermatome (dermis)
Myotomes: become split into dorsal epimere and ventral hypomere ---Epimere: develops extensor muscles of vertebral column ---Hypomere develops into limb and body wall muscles (flexors/extensors) ------forms a dorsal condensation (limbs) which become extensor muscles; and ventral condensation which become flexor muscles Molecular Regulation: both mitotic and postmitotic ---somitic epithelium is affected by growth factors produced by the somatic lateral plate and produce myogenic progenitor cells, which in turn express transcription factors that facilitate muscle development |
|
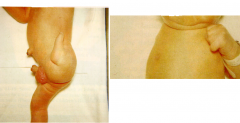
What is the name of this congenital anomaly of the limb and where did the problem occur in the developmental pathway?
|
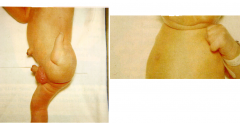
Reduction defects:
---Meromelia: part of a limb is missing ---Amelia: the entire limb is missing Caused by problems with the AER, as the limb bud did not proliferate/no outgrowth of limb bud |
|

What is the name of this congenital anomaly of the limbs and where did the problem occur in the developmental pathway?
|
Duplication defect:
---Polydactyly: extra limb elements are present Caused by a problem with ZPA, transplanted into anterior limb bud |
|

What is the name of this congenital anomaly of the limbs and where did the problem occur in the developmental pathway?
|
Dysplasia:
---Syndactyly: malformation of parts of the limb Caused by lack of apoptosis, cell death did not occur where it should have and limbs became fused |
|
|
What causes limb defects and when do they usually occur during development?
|
Critical period for limb development is from 24-36 days
---most defects are of multifactorial etiology (genetics, physical and teratogenic factors) |
|
|
What is the collateral circulation around the hip joint?
|
Cruciate anastomosis:
---inferior gluteal artery, medial femoral circumflex artery, lateral femoral circumflex artery, first perforating branch of profundus femoris artery |
|
|
What is the collateral circulation around the head of the femur?
|
Trochanteric anastomosis:
---superior gluteal artery, inferior gluteal artery, medial femoral cirumflex artery, lateral femoral circumflex artery |
|
|
What is the collateral circulation around the knee joint?
|
Genicular anastomosis:
---superior lateral genicular artery, inferior lateral genicular artery, superior medial genicular artery, inferior medial genicular artery, descending genicular artery (from femoral artery), descending branch of the lateral femoral circumflex artery, anterior tibial recurrent artery |
|
|
What are the spinal cord segments for the femoral nerve?
|
L2-L4
|
|
|
What are the spinal cord segments for the obturator nerve?
|
L2-L4
|
|
|
What are the spinal cord segments for the tibial nerve?
|
L4-S3
|
|
|
What are the spinal cord segments for the common fibular nerve?
|
L4-S2
|
|
|
Describe the structure and function of microglia.
|
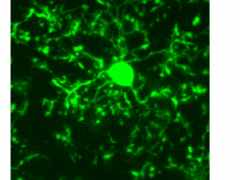
Specialized immune cells found only in brain that can detect damaged or unhealthy neurons
---phagocytic and defend against invading pathogens |

