![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
Describe the movements of the mandible at the temporomandibular joint and the muscles responsible. What is their innervation?
|
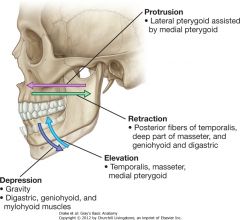
Movements: synovial joints - 2 cavities (lower - rotation, 11-25mm opening; upper - glide, 25-45mm opening)
---protrusion/retraction ---elevation/depression ---bilateral movement: both sides must be coordinated Muscles: of mastication ---Masseter: elevation and protrusion of mandible (superficial)/elevation and retraction (deep); masseteric nerve from mandibular nerve V3 ---Temporalis: elevation and retraction, participates in side to side movements; deep temporal nerve from mandibular nerve V3 ---Medial pterygoid: elevation, protrusion and side to side movements; nerve to medial pterygoid from mandibular nerve V3 ---Lateral pterygoid: protrusion, depression and side to side movement; nerve to lateral pterygoid from mandibular V3 or buccal branch |
|
|
Describe the location and the important neurovascular structures of the infratemporal fossa.
|

Infratemporal fossa:
---inferior to temporal fossa, deep to masseter muscle and underlying ramus of mandible Contents: ---Mandibular nerve/branches: both sensory* and motor 1. First fibers: ---tensor tympani ---tensor veli palatini ---medial pterygoid ---meningeal* 2. Anterior division: ---temporal ---masseter ---lateral pterygoid ---buccal* 3. Posterior division ---lingual (with chorda tympani)* ---inferior alveolar* ---mylohyoid ---auriculotemporal* ---Maxillary artery and branches: major source of blood supply for nasal cavity, lateral wall/roof of oral cavity, teeth and dura mater ---Middle meningeal: supplies dura mater, bone and bone marrow ---Inferior alveolar: passes through mandibular canal with nerve, supplying lower teeth, gums, chin and lip ---small branches: deep auricular, anterior tympanic and accessory meningeal (external acoustic meatus, tympanic membrane, dura mater) ---Deep temporal: usually two, pass into temporal fossa ---Masseteric and buccal arteries follow nerves ---Otic ganglion: parasympathetic ---preganglionic travel with the CN IX glossopharyngeal (lesser petrosal/tympanic nerve) to ganglion ---postganglionic travel along auriculotemporal (branch of V3) to parotid gland |
|
|
Describe the location and important neurovascular structures of the pterygopalatine fossa.
|
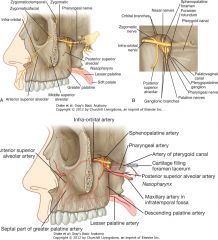
Pterygopalatine:
---space between bones on lateral side immediately posterior to maxilla Contents: ---Maxillary nerve/branches ---Orbital branches ---Greater/lesser palatine nerves: pass through pterygopalatine ganglion ---Nasal nerves ---Pharyngeal nerve: passes posterior from pterygopalatine ganglion ---Zygomatic nerve: two branches (zygomaticotemporal/zygomaticofacial) ---Posterior superior alveolar nerve ---Infra-orbial nerve ---Nerves forming nerve of pterygoid canal: ---Greater petrosal nerve: originates from geniculate ganglion (VII); carries parasympathetic to glands above oral fissure and some taste from soft palate ---Deep petrosal nerves: formed by postganglionic sympathetic fibers originating from superior cervical ganglion (preganglionic from T1 spinal nerve) ---Pterygopalatine ganglion: ---preganglionic travel along CN VII on greater petrosal nerve to ganglion ---postganglionic travel along zygomaticotemporal and lacrimal to lacrimal/nasal glands |
|
|
Describe the muscles that form the floor of the mouth.
|
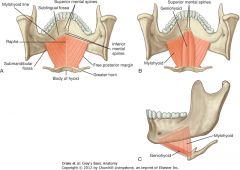
Mylohyoid:
---supports and elevates floor of oral cavity; elevates and pulls forward hyoid bone/larynx during initial stages of swallowing; when hyoid fixed, depresses mandible ---innnervation: nerve to mylohyoid from inferior alveolar branch from mandibular nerve V3 Geniohyoid: ---depresses mandible when hyoid fixed; elevates and pulls hyoid forward when mandible fixed |
|
|
Describe the intrinsic and extrinsic muscles of the tongue, their sensory and motor innervation and how nerve fibers reach the tongue.
|
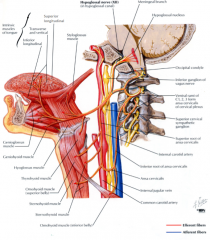
Intrinsic muscles: alter shape of the tongue
---Superior longitudinal: shortens and curls ---Inferior longitudinal: shortens and uncurls; turns it down ---Transverse: narrows and elongates ---Vertical: flattens and widens Extrinsic muscles: ---Genioglossus: protrudes and depresses center ---Hyoglossus: depresses ---Styloglossus: elevates and retracts ---Palatoglossus*: depresses palate, elevates back of tongue Innervation: ---Motor: ---Except to palatoglossus, which is innervated by vagus X, all muscles are innervated by hypoglossus XII ---Sensory: ---anterior 2/3: general sensation - mandibular V3 via lingual nerve; special sense - facial VII via chorda tympani (runs along with lingual) ---posterior 1/3: general/special sense - glossopharyngeal IX |
|
|
Describe the location of the three salivary glands and their emptying mechanism. What is their innervation and its course?
|
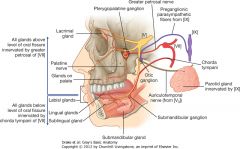
Parotid gland:
---anterior SCM, inferior to ear ---duct penetrates buccinator and opens into oral cavity adjacent to second upper molar ---innervation: parasympathetic - preganglionic travel along glosspharyngeal to otic ganglion where postganglionic travel along auriculotemporal (mandibular V3) Submandibular: ---located along inferior margin of mylohyoid and medial border of mandible ---duct emerges beside base of frenulum of tongue Sublingual: ---smallest, lies lateral to submandibular duct ---drains into openings in sublingual fold ---Innervation: all glands below oral fissure; parasympathetic ---Chorda tympani (VII) - follows lingual nerve, preganglionic synapse with postganglionic in submandibular ganglion and pass directly to glands |
|
|
What structures form the roof of the mouth? Describe the function and innervation of the muscles of the soft palate.
|

Roof: consists of soft and hard palate
---hard palate is bone; continuous with soft palate posteriorly - acts as valve to close oropharyngeal isthmus or elevate to separate nasopharynx from oropharynx Muscles: ---Tensor veli palatini: tenses soft palate, opens pharyngotympanic tube ---Levator veli palatini: elevates soft palate above neutral ---Palatopharyngeus: depresses soft palate and moves palatopharyngeal arch midline, closing oropharyngeal isthmus; elevates pharynx ---Palatoglossus: depresses palate and moves palatopharyngeal arch midline, closing oropharyngeal isthmus; elevates back of tongue Innervation: ---Except to tensor veli palatini which is innervated by mandibular V3, all palate muscles are vagus X |
|
|
Describe the anatomical organization of the three regions of the nasal cavity, including the medial and lateral walls and the nasal septum.
|
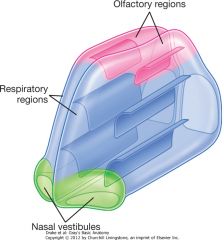
Regions:
---Nasal vestibule: small dilated space just internal to nares lined by skin and contains hair follicles ---Respiratory region: largest portion, has rich neurovascular supply; lined by respiratory epithelium composed of mainly ciliated and mucous cells ---Olfactory region: small, at apex of nasal cavity, lined by olfactory epithelium and contains olfactory receptors Medial wall: separates nasal cavities, is mucous covered portion of nasal septum ---consists of anterior cartilage and posteriorly, vomer and ethmoid bones, with some nasal, frontal, maxillary, palatine, and spheniod bones Lateral wall: formed by bone, cartilage and soft tissue ---consists of ethmoid labyrinth and uncinate process, palatine, sphenoid, lacrimal and maxillary bones and inferior concha |
|
|
Describe the innervation and vascular supply of the nasal cavities.
|
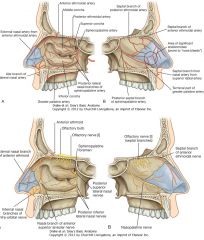
Innervation:
---Olfactory (I): special sense for olfaction; composed of axons from receptors in olfactory epithelium, with bundles synapsing with neurons in olfactory bulb ---Ophthalmic (V1): branches - anterior/posterior ethmoidal nerves (from nasociliary nerve) ---Maxillary (V2): branches - posterior superior medial/lateral nasal nerves, nasopalatine nerve, posterior inferior nasal nerve ---parasympathetic: secretomotor - preganglionic (facial VII) travel along greater petrosal to pterygopalatine ganglion, postganglionic travel along with maxillary V2 ---sympathetic: preganglionic (TI) synapse in superior cervical ganglion, travel along with internal carotid artery and joins deep petrosal nerve, which joins greater petrosal and travels with maxillary V2 Arteries: from both internal and external carotid ---Sphenopalatine: terminal branch of maxillary (external carotid) ---Greater palatine: branch of maxillary (external carotid); anastomoses with sphenopalatine ---Superior labial and lateral nasal arteries: from facial artery (external carotid) ---Anterior and posterior ethmoidal arteries: from ophthalmic artery (internal carotid) Veins: follow arteries, drain into pterygoid plexus of veins or facial vein |
|
|
Describe the location of the paranasal sinuses and where they drain.
|
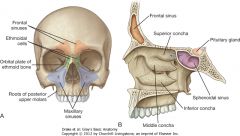
---developed from outgrowths of nasal cavites and eroded into the surrounding bone
---lined by respiratory mucosa (ciliated/mucus secreting) ---opens into nasal cavities ---innervated by branches of trigeminal V Frontal sinus: ---one on each side, most superior and are found in frontal bone under forehead ---drains onto lateral wall of middle meatus through the frontonasal duct Ethmoidal cells: ---on each side, fill ethmoidal labyrinth, medial to orbits and lateral to nasal cavity; formed by variable number of individual air chambers (anterior, posterior, middle) Maxillary sinuses: ---one on each side, largest and fill body of maxillae ---opens into semilunar hiatus (lateral wall of middle nasal meatus) Sphenoidal sinuses: ---one on each side, within body of sphenoid ---opens into roof of nasal cavity through apertures on posterior wall |
|
|
Describe the structure of the eyelid, the consequences of nerve damage and how the conjunctiva is related.
|
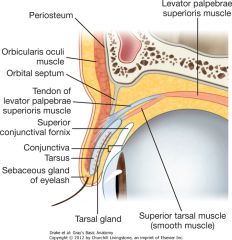
Eyelid:
---Layers: skin, subcutaneous tissue, voluntary muscle, orbital septum, tarsus and conjunctiva ---Voluntary muscle: orbicularis oculi - palpebral portion controls (closes) eyelids; innervated by facial VII ---Orbital septum: extension of periosteum from orbit, attached to tarsus/levator palpebrae superioris ---Tarsus: superior/inferior, provides support for eyelid; levator palpebrae superioris functions within superior tarsus, raises eyelid; superior tarsus also has superior tarsal muscle (smooth muscle), controlled by postganglionic sympathetic ---Conjunctiva: thin membrane, covers posterior surface of eyelid and reflects onto sclera, extending to the junction between sclera/cornea Damage: ---Ptosis: ---loss of innervation of orbicularis oculi (facial VII) leads to inability to close eyelids tightly and lower eyelid droops away, creating spillage of tears ---loss of innervation of levator palpebrae superioris (oculomotor III) leads to inability to open superior eyelid voluntarily (complete ptosis) ---loss of innervation of superior tarsal muscle (sympathetic) leads to constant partial ptosis - Horner's syndrome (caused by lesion in sympathetic trunk in neck): pupillary constriction due to paralysis of dilator pupillary muscle, partial ptosis (drooping of upper eyelid) due to paralysis of superior tarsal muscle |
|
|
Describe the sensory and autonomic innervation of the lacrimal gland and how the nerves reach it. Trace the course of its secretions from gland to nasal cavity.
|
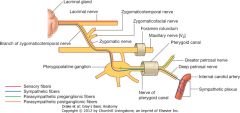
Lacrimal gland:
---Sensory innervation: lacrimal branch of ophthalmic V1 ---Secretomotor (parasympathetic) innervation: stimulate fluid secretion from gland - preganglionic leave CNS via facial nerve VII, enter greater petrosal which becomes nerve of pterygoid canal and joins the pterygopalatine ganglion; postganglionic travel with maxillary V2, follow zygomatic/zygomaticotemporal branches to join lacrimal nerve ---Sympathetic innervation: postganglionic originate in superior cervical ganglion, travel along internal carotid, joining with deep petrosal which becomes nerve to pterygoid canal and passes through pterygopalatine ganglion to eventually join lacrimal nerve Course: Lacrimal apparatus ---tears produced in lacrimal gland in superior lateral corner of eye, with many ducts opening into upper margin of conjunctival sac ---tears are swept medially over eye by blinking and are collected in small openings (lacrimal puncta) one on each upper/lower eyelid near lacrimal lake in medial corner ---puncta lies on small raised mound of tissue (lacrimal papilla) and is opening of small canal (lacrimal canaliculus) that connects with lacrimal sac ---lacrimal sac drains tears via nasolacrimal duct into nasal cavity |
|
|
Describe the extraocular muscles, including their attachments, function and innervation.
|
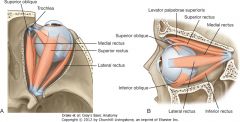
Levator palpebrae superioris:
---attachements: lesser wing of sphenoid to anterior surface of tarsal plate ---function: elevation of upper eyelid ---innervation: oculomotor III Superior rectus: ---attachments: superior part of tendinous ring to anterior half of superior eyeball ---function: elevation, adduction, medial rotation ---innervation: oculomotor III Inferior rectus: ---attachment: inferior part of tendinous ring to anterior half of inferior eyeball ---function: depression, adduction, lateral rotation ---innervation: oculomotor III Medial rectus: ---attachment: medial part of tendinous ring to anterior half of medial eyeball ---function: adduction ---innervation: oculomotor III Lateral rectus: ---attachment: lateral part of tendinous ring to anterior half of lateral eyeball ---function: abduction ---innervation: abducens VI Superior oblique: ---attachment: body of sphenoid, superomedial optic canal to outer posterior/superior portion of eyeball ---function: depression, abduction, medial rotation ---innervation: trochlear IV Inferior oblique: ---attachment: medial floor of orbit/maxilla to outer posterior inferior portion of eyeball ---function: elevation, abduction, lateral rotation ---innervation: oculomotor III |
|
|
Describe how the extraocular muscles are tested clinically.
|

Movement:
---occurs around two main axes (horizontal/vertical) and one minor (anterior/posterior) ---horizontal: elevation/depression ---vertical: abduction/adduction Testing: ---lateral rectus (LR) - CN VI: action - abduction; test - abduction ---medial rectus (MR) - CN III: action - adduction; test - adduction ---Superior rectus (SR) CN III: action - elevation/adduction; test - abduct and look superior (counteract IO) ---Inferior rectus (IR) CN III: action - depression/adduction; test - abduct and look inferior (counteract SO) ---Superior oblique (SO) CN IV: action - depression/abduction; test - adduct and look inferior (counteract IR) ---Inferior oblique (IO) CN III: action - elevation/abduction; test - adduct and look superior (counteract SR) |
|
|
Describe the afferent and efferent components and pathways of the pupillary light reflex.
|

Pupillary light reflex: tests CN II and III/CNS pathways; to test: shine bright light in one eye
---direct pupillary reflex: ipsilateral pupil constricts ---consensual pupillary reflex: contralateral pupil also constricts Pathway: ---afferent: CN II carries info of light intensities into CNS; branches synapse with interneurons in midbrain ---efferent (visceral): midbrain interneurons synapse with preganglionic parasympathetic neurons in midbrain (oculomotor), send axons via CN III to ciliary ganglion; postganglionic enter sclera via short ciliary neres and reach pupillary constrictor muscles of iris |
|
|
Describe the afferent and efferent components and pathways of the pupillary dilation reflex.
|
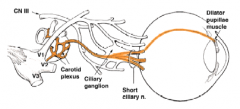
Pupillary dilation reflex: dilation of pupil occurs passively when parasympathetic input (reduction of light intensity) to constrictor is decreased and actively when sympathetic input to dilator is increased (during intense emotion/pain); to test: usually tested passively, seeing dilation after constriction
Pathways: ---preganglionic sympathetics from thoracic spinal cord ascend to superior cervical ganglion and synapse with postganglionics; travel via internal carotid artery through ciliary ganglion and short ciliary nerves to sclera - innervate dilator pupillae muscle in iris |
|
|
Describe the afferent and efferent components and pathways of the accommodation reflex.
|

Accommodation reflex: for near vision, tests integrity of CN II and III; maintains distinct image on retina as object moves closer to eyes
---Contraction of medial rectus in both eyes, causing adduction ---Constriction of pupil to focus light rays on central portion of retina ---Contraction of ciliary muscles in eye to increase convexity of kens to shorten focal length ---to test: hold object away from face, then move toward nose Pathways: ---afferent: CN II carries info about position of object to CNS, branches relay info to parasympathetic and somatic motor of CN III ---efferent (somatic): axons from CN III are carried into orbits and innervate medial rectus and synapse in ciliary ganglion ---efferent (visceral): postganglionic parasympathetics from ciliary ganglion travel into eye through short ciliary nerves to innervate pupillary constrictors and ciliary muscles (regulate tension of suspensory ligaments of lens) |
|
|
Describe the afferent and efferent components and pathways of the corneal (blink) reflex.
|

Corneal reflex: not strictly visual reflex, but requires intact afferent/efferent somatic innervation; to test: light touching of cornea/conjunctiva should result in blinking of eyelids
Pathway: ---afferent: information from cornea/conjunctiva travels through branches of ophthalmic V1 to trigeminal ganglion and CNS; some fibers synapse with interneurons in brainstem, which relay info to motor neurons of CN VII ---efferent: motor fibers of CN VII exit skull through stylomastoid foramen; temporal/zygomatic branches innervate orbicularis oculi and mediate blink response to stimulation of cornea/conjunctiva |
|
|
Describe the development of the face.
|

Facial development: mesenchyme covered by ectoderm, lined by endoderm
---Frontonasal prominence: forehead, bridge of nose, medial/lateral nasal prominences ---medial nasal prominence: philtrum of upper lip, crest/tip of nose ---lateral nasal prominence: alae of nose ---Maxillary prominence: cheeks, lateral portion of upper lip ---1st pharyngeal arch (mandibular prominence): lower lip ***grooves between facial prominences smooth out to form "human" appearance around wk 10*** |
|
|
Describe the development of the nose and nasal cavity.
|
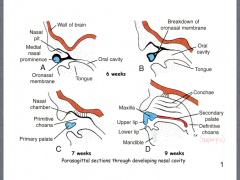
Nasal placode forms in frontonasal prominence
---invagination of placode and accumulation of mesenchyme forming medial/lateral nasal prominences creates nasal pit Nasal cavity: ---oronasal membrane that projects from the medial nasal prominence breaks down, eliminating the separation of the nasal cavity from the oral cavity, creating the primary palate and primitive choana ---During wk 9, primary palate becomes maxilla and the secondary palate is formed, separating the cavities and creating the definitive choana |
|
|
What congenital anomalies can occur during development of the nose?
|
Regulation of induction and errors with sonic hedgehog (excess/not enough) can lead to:
---facial duplication (partial or complete) ---absence of external nose |
|
|
Describe the formation of the eye before the optic cup is formed.
|

Formation:
---occurs by induction of the lens by the optic vesicle ---appears in 22-day embryo as pair of shallow grooves on sides of forebrain (thickening of neural ectoderm) ---as cranial neuropore closes, optic grooves become enclosed inside cranial cavity, forming outpocketings of the forebrain (optic vesicles) ---At 4 wk, optic vesicles bulge laterally from diencephalon of neural tube and contact thickened lens placode ---At wk 5, optic vesicle begins to invaginate to form optic cup and lens placode also invaginates |
|
|
Describe the formation of the eye after optic cup has developed and it's derivatives in the adult eye.
|

Optic cup: 2 layers
---pigmented retina (outer) ---neural retina (inner): forms rods/cones/ganglion Lens: ---vesicle pinches off from surface and becomes solid cellular lens ---at wk 7, processes of ganglion cells in neural retina are growing towards brain within wall of optic stalk to form optic nerve ---eyelids, forming at 6 wk, are beginning to grow towards each other in front of developing cornea; fuse around wk 10 and reopen during third trimester ---By wk 15, choroid, sclera, cornea and extraoculat muscles form from mesenchyme surrounding layers of retina; eyelids have fused and margin of optic cup is growing anterior to lens as iris |
|
|
Describe the development of the optic nerve and retinal arteries.
|
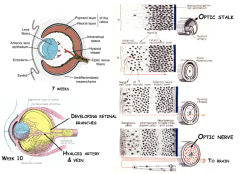
At 7 wk:
---as layers of neural retina develop from inner layer of optic cup, axons of ganglion cells move along surface of retina toward optic stalk ---move through wall of stalk creating optic nerve ---hyaloid artery runs in groove on ventral surface of optic cup and as groove fuses, the artery becomes trapped within the developing optic nerve Artery: ---Hyaloid artery branches from ophthalmic artery and side branches grow over surface of neural retina as it develops ---portion of vessels supplying lens degenerate, leaving hyaloid canal as remnant ---portions supplying retina becomes central artery and vein of retina |
|
|
Describe the structures involved in formation of primary and secondary palates.
|

Primary: forms from first and includes central portion of lip and alveolar bone containing incisors
---formation occurs through union between maxillary, medial/lateral nasal prominences below developing nasal cavity ---forms nasal fin, which disappears, allowing cells of processes to merge Secondary: forms later and includes remainder of hard and soft palate ---ridges of tissue (palatal shelves) grow from medial side of maxillae and lie on either side of tongue; shelves form secondary palate (hard - posterior to primary/all of soft) ---palatal shelves reorient to more horizontal position above tongue (moves down to create space); medial edges fuse with each other and lower surface of nasal septum |
|
|
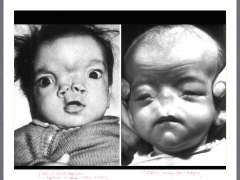
What congenital anomalies occur during the development of the palate?
|

Primary palate:
---failure in development and/or breakdown of nasal fin results in cleft lip ---can be caused by vitamin A or steroids Secondary palate: ---cleft palate; problem with fusion of processes Can occur together or separately |
|
|
Describe the general components of blood and its functions.
|

Blood:
---specialized connective tissue normally confined to circulatory system Components: ---Plasma: composed of water, proteins and other solutes ---Erythrocytes: red blood cells ---Buffy coat: composed of platelets and leukocytes Functions: ---transport of CO2 and O2 ---distribution of nutrients ---transportation of waster products ---stabilization of pH and electrolyte concentrations in interstitial fluid ---regulation of body temperature ---immune defense |
|
|
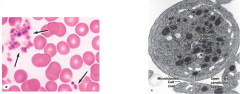
Describe red blood cells, their function and life span, as well as the different blood types.
|
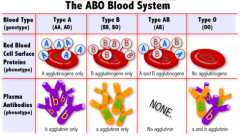
Flexible cell lacking nucleus and organelles - terminally differentiated
Transport O2 and CO2; main contributor to hematocrit (percentage of whole blood occupied by cellular elements): 45-52% for men, 37-48% for women Life span: 120 days - senescent cells removed from circulation by macrophages in spleen, liver, and bone marrow ---Anemia: deficiency of RBC and/or hemoglobin (reflected in CBC as decreased red cell count, decreased hemoglobin and decreased hematocrit) ---blood loss (hemorrhage) ---insufficient production of erythrocytes in bone marrow ---production of erythrocytes with insufficient hemoglobin (iron deficiency) ---accelerated destruction of erythrocytes (less than 120 day life span) Blood types: RBCs have genetically determined cell surface proteins which distinguish blood type (A, B, AB, O) ---Type O=universal donor ---Type AB=universal acceptor Rh blood groups: genetically determined cell surface protein called D-antigen ---D-antigen present=Rh+ (85% of population) ---No D-antigen present=Rh- ---potential problem for Rh- women who conceive Rh+ child |
|
|
Describe platelets, their function and life span.
|
Platelets: fragments of cytoplasmic processes of megakaryocytes in bone marrow
---120,000-300,000 per microliter of blood Function: ---blood clot formation and transporting clotting factors; more than "band-aid" of blood stream, also carry growth factos and other proteins Life span: 10-12 days |
|
|
Describe the white blood cells (leukocytes), their primary functions and life spans.
|
Leukocytes: made in bone marrow and mature in thymus; some seed other lymphoid organs where retain ability to divide and differentiate
---granular and agranular ---6000-10,000 per microliter of blood Function: defense and response to injury ---Leukopenia: low numbers of WBCs (<3 X 10^9/liter) ---Leukocytosis: high numbers of WBCs (11-17 X 10^9/liter) Life span: measure in days |
|
|
Describe neutrophils, their function and histological structure.
|
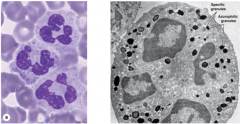
Neutrophils: 60-70% of circulating leukocytes (largest in number)
---granular, and granules don't stain with acidic/basic dyes ---multilobed nucleus, twice as large as RBC ---highly mobile cells usually first to arrive at site of injury Function: ---specialize in engulfing debris and digesting bacteria |
|
|
Describe eosinophils, their function and histological structure.
|
Eosinophils: 2-4% of circulating leukocytes
---granular, granules stain with red acidic dye (eosin) ---bilobed nucleus Function: ---cells that remove foreign materials that have reacted with antibodies (antigen/antibody complexes) ---*rapid increase in numbers in response to parasitic infections* ---source of factors mediating allergic reactions and asthma |
|
|
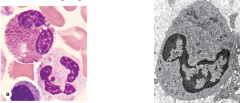
Describe basophils, their function and histological structure.
|

Basophils: <1% of circulating leukocytes (lowest in number)
---granular, granules stain with basic blue dye (hemotoxalyn) ---so many granules, nucleus is obscured Function: ---migrate to sites of injury and cross blood vessel wall ---release histamines to mediate allergic reactions when activiated by antigen binding ---increased numbers observed in hypersensitivity reactions (bronchial asthma and allergic skin reactions) and chronic inflammatory conditions |
|
|
Describe monocytes, their function and histological structure.
|

Monocytes: 2-8% of circulating leukocytes
---agranular, characteristic kidney/U-shaped nucleus Function: ---gives rise to macrophages that engulf and kill microorganisms and secrete factors that are important for tissue repair remodeling Two types of macrophages: ---M1: derived from blood monocytes that migrate into tissue in steady state (resident); proliferate in response to inflammation ---M2: derived from blood monocytes that migrate into tissues in response to inflammation ---bacterial phagocytosis, antigen presentation, ingestion of dead cell debris, angiogenesis and ECM production |
|
|
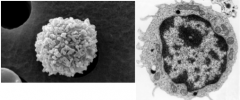
Describe lymphocytes, their function and histological structure.
|
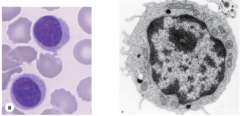
Lymphocytes: 20-30% of circulating leukocytes
---agranular, spherical nuclei that take up most of cell; about the size of RBC ---small number circulate in blood, most in lymphatic tissues ---only leukocyte that can return to blood after leaving blood vessel Function: ---immune defense against microorganisms, foreign/abnormal antigens, cancer cells Three types: ---B lymphocytes: 25-30% of circulating lymphocytes; produced and mature in bone marrow; distributed to connective tissues, epithelia, lymphoid nodules/organs ---humoral - produce antibodies during immune response ---T lymphocytes: 65-75% of circulating lymphocytes; produced in bone marrow, mature in thymus; distributed to connective tissues and lymphoid organs ---Natural Killer (NK) cells: 10-15% of circulating lymphocytes |
|
|
Describe B lymphocytes and their function
|
B lymphocytes:
---IgM on cell surface recognizes antigens ---recognition of antigen leads to cell proliferation and differentiation of cells into plasma cells, which actively secrete antibodies against antigens ---T helper cells aid in activation of B lymphocyte through cytokine production |
|
|
Describe T lymphocytes and their function.
|
T lymphocytes:
---T cell receptor (TCR) on cell surface recognizes antigens/peptides provided by antigen presenting cells (APC), which are usually macrophages though differs cell to cell 3 subclasses: ---Helper T cells (CD4+): produce cytokines that promote differentiation/activation of other immune cells ---Cytotoxic T cells (CD8+): act directly against foreign cells or virus-infected cells ---Regulatory T cells: suppress excessive immune responses |
|
|
Descibe NK cells and their function.
|
NK cells:
---attack and kill virus-infected cells, transplanted cells and cancer cells without previous stimulation |
|
|
Describe the process of hematopoiesis.
|

Sites of hematopoiesis:
---yolk sac of embryo ---liver/spleen during 2nd trimester ---bone marrow during 3rd trimester Depends on presence and activity of specific growth factors/cytokines ---colony-stimulating factors (CSF) *ability to self renew ---myeloid/lymphoid stem cells are multipotent |
|
|
Describe the structural components of lymphoid system.
|

Primary lymphoid organs:
---involved in lymphocyte production and maturation ---bone marrow and thymus Secondary lymphoid organs: ---become populated with mature lymphocytes ---spleen, lymph nodes, tonsils, appendix, Peyer's patches |
|
|
Describe the innate immunity of the lymphoid system.
|
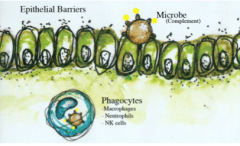
Innate immunity:
---responds rapidly ---non-specific ---does not produce memory cells ---depends on intact epithelial barriers and complement Components: ---physical barriers (skin) ---protective secretions (mucous) ---phagocytic cells (macrophages/neutrophils) ---enzymes (digestive) ---components of complement system that recognize common antigens found on microorganisms ----cytokines produced by phagocytic cells to alter surrounding blood vessels to recruit other immune cells |
|
|
Describe adaptive immunity and its two different components.
|

Adaptive immunity:
---responds slowly ---specific ---has immunological memory ---depends on B and T lymphocytes to mount immune response Humoral immunity: ---mediated by B lymphocytes; relies on antibodies produced by plasma cells in response to soluble antigen Cellular immunity: ---mediated by T lymphocytes; secrete cytokines that act on other immune cells, attack foreign cells, infected cells and some tumor cells; occurs intracellular ---Helper T cells use class II MHC molecules; Cytotoxic T cells use class I MHC molecules ---both types of immune response are activated at same time when foreign epitopes are recognized |
|
|
Describe bone marrow as a lymphoid organ and its histological structure.
|
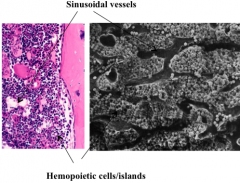
Bone marrow:
---primary organ ---origin and maturation of B lymphocytes; origin of T lymphocytes Contains: ---sinusoidal vessels and hemopoietic cells/islands (progenitor cells) |
|
|
Describe the thymus as a lymphoid organ, its histological structure and T lymphocyte maturation process.
|
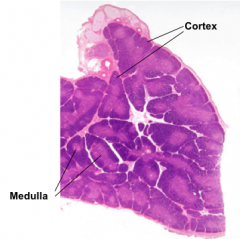
Thymus:
---located in superior mediastinum ---originates early in embryo, reaches peak development during youth and then begins to atrophy Cortex: composed of T lymphoblasts (thymocytes) in stroma of epithelial reticular cells; immature Medulla: composed of reticular cells and mature T lymphocytes Maturation: ---lymphoblasts in cortex undergo thymic selection ---lymphoblasts develop TCRs and are presented with antigens by reticular cells and other APCs ---those cells that do not recognize peptides at all undergo apoptosis: positive selection (80% of total) ---those cells that recognize self-peptides also undergo apoptosis: negative selection (17% of total) ---selected cells (3%) migrate into medulla and enter blood circulation; seed secondary lymphoid organs |
|
|
Describe lymph nodes and their histological structure.
|

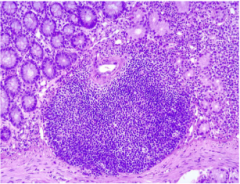
Lymph nodes:
---secondary lymphoid organs; surrounded by capsule with own blood supply - lymph enters afferent vessel ---is site of lymphocyte proliferation (B cells in germinal centers) as well as transformation of B cells to plasma cells ---lymph that leaves node is often enriched in antibodies ---Cortex: contains primarily B lymphocytes; lymphoid nodules with/without germinal centers; many other cell types (macrophages, reticular cells, APCs) ---Paracortex: no precise boundaries, no B cell lymphoid nodules; primarily T cells ---Medulla: medullary cords are extensions of paracortex containing primarily activated B cells and plasma cells; medullary sinuses that deliver lymph to efferent lymphatic vessel All lymph formed in tissues must pass through at least one lymph node before entering venous blood stream Lymph contains: ---soluble antigens ---microorganisms ---macrophages and APCs with internalized antigens ---all are presented to B lymphocytes, T helper cells and cytotoxic T cells |
|
|
Describe the lymph nodes and their histological structure.
|

Lymph nodes:
---secondary lymphoid organs; surrounded by capsule with own blood supply - lymph enters afferent vessel ---is site of lymphocyte proliferation (B cells in germinal centers) as well as transformation of B cells to plasma cells ---lymph that leaves node is often enriched in antibodies ---Cortex: contains primarily B lymphocytes; lymphoid nodules with/without germinal centers; many other cell types (macrophages, reticular cells, APCs) ---Paracortex: no precise boundaries, no B cell lymphoid nodules; primarily T cells ---Medulla: medullary cords are extensions of paracortex containing primarily activated B cells and plasma cells; medullary sinuses that deliver lymph to efferent lymphatic vessel All lymph formed in tissues must pass through at least one lymph node before entering venous blood stream Lymph contains: ---soluble antigens ---microorganisms ---macrophages and APCs with internalized antigens ---all are presented to B lymphocytes, T helper cells and cytotoxic T cells |
|
|
Describe the spleen and its histological structure.
|

Spleen:
---secondary lymphoid organ; two components: Red pulp: ---composed of vascular sinuses, macrophages, RBCs and plasma cells, lymphocytes (splenic cords of Bilroth) ---destruction of defective/aged erythrocytes and platelets ---promotion of monocyte differentiation into tissue macrophages White pulp: ---composed of lymphoid nodules (B cells) with germinal center (light staining) and marginal zone (dark staining) ---periarteriolar lymphoid sheaths consist of layer of T cells around central artery ---site of antigen-dependent differentiation/activation of T and B lymphocytes |
|
|
Describe the tonsils and their histological structure.
|
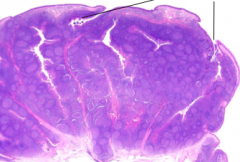
Tonsils:
---secondary organs; partially encapsulated aggregates of lymphoid nodules that guard entrance to oral and nasal pharynx against airborne/ingested antigens Tonsilar crypts: ---invaginations of stratified squamous non-keritinized epithelium |
|
|
Describe the mucosa-associated lymphoid tissue and it histological structure.
|
---secondary organ; non-encapsulated infiltration of lymphocytes, APCs and plasma cells into mucosa of gastrointestinal, respiratory and urinary tracts (all open to external environment)
|

