![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
|
Cells involved in acute inflamation
|
granulocyte, leukocyte, macrophage
|
|
|
granulocyte
|
any blood cell containg specific granules (e.g. neutrophils, eosinophils, basophils)
|
|
|
leukocyte
|
a colorless blood cell capable of ameboid movement (e.g. lymphocytes, monocytes, granulocytes)
|
|
|
macrophage
|
large phagocytic mononuclear cell
|
|
|
Complications of biomaterial-tissue interactions
|
alters physiological process such as inflammation, immunity, and blood coagulation
Change in physiological system comprises host defense mechanisms |
|
|
Neutrophils
|
most common one, segmented nuclei connected by thin strands of chromatin
first to appear at injury site Functions -cells become sticky -stick to capillary endothelium -penetrate between the endothelial cells -move into the surrounding damaged tissue -emigration begins minutes to hours after injury and may continue for as long as 24 hr Activates when engages foreign particles |
|
|
Eosinophils
|
bi-lobed nucleus
|
|
|
Basophils
|
least common, large cytoplasmic granules which obscure the nucleus
|
|
|
Monocytes
|
the largest one, deeply indented or U-shaped nucleus
|
|
|
4 sign of acute inflamation
|
rubor (redness)
Tumor (swelling) Calor (heat) Dolor (pain) |
|
|
functions of inflammatory response
|
-Delivery of effector molecules and cells to the sites of infection
-The formation of a physical barrier to the spread of the tissue damage or infection -Wound healing and tissue repair |
|
|
Tumor (swelling)
|
Increases pressure and inhibits blood flow (normal conditions = low permability tight endothelim- slow fluid flow and small molecules permeate lymphatic vessels drain away fluid) Increased permeability in inflammation allows for larger molecules to move into tissue at a greater rate Increased fluid influx not promptly balanced by the lymphatic system |
|
|
Rubor (redness)
|
Erythrocytes rush to the injury area and accumulate there
|
|
|
Calor (heat)
|
Increased cellular metabolic activity (Good)
Possible generation of pyrogens which are known to cause systemic fever. Local disturbance of fluid flow |
|
|
Dolor (pain)
|
From edema and kinins
local edema may activate local deep pain receptors kinins act directly on nerve ends to produce pain sensations |
|
|
Steps of Inflammatory Response
|
1) Damage tissues release histamine, which increases blood flow to the area
2)Histamines cause capillaries to leak, releasing phagocytes and clotting factors into the wound 3)Phagocytes engulf bacteria, dead cells, and cellular debris 4)Platelets move out of the capillary to seal the wounded area RBCS bring O2 and ATP to fight bacteria |
|
|
Acute Inflammation process
|
Initial stage = rapid dilation of capillaries and increase permeabiliy in their endothelial cell linings
Dilation leads to an increase in blood entry into the capillary bed -foreign protein or material>coagulation factor> kinins>dilation and endothelial permeation -loss of plasma through the capillary wall -platelets and erythrocytes become sticky -blood flows slower and sludgy |
|
|
Acute Inflammation Cell Process
|
First neutrophils predominate for several days and then are replace by monocytes.
The Monocytes neutrophils because neutrophils are short lived, limited emigration, chemotactic factors for neutrophils are not active in late stages of inflamation Monocyte emigration continues for days to weeks Monocytes differentiate into macrophages which are very long lived |
|
|
Successful response to acute inflammation
|
reduction in local tissue mass and fluid (edema)
dead cells removed by neutrophils and macrophages engulfment and degradation of biomaterial may or may not occur |
|
|
Chronic Inflammation
|
Follows the acute inflammatory stage, b/c persistent inflammatory stimuli
(chemical and physical properties of biomaterials, Motion in the implant site) is confined to implant site |
|
|
Characteristics of Chronic Inflammation
|
-presence of macrophages, monocytes, and lymphocytes
-proliferation of blood vessels and connective tissue -No exudates (a mass of cells) |
|
|
Function of macrophages
|
produce great number of biologically active products
-proteases to degrade molecules -Chemotactic factors -growth promoting factors -cytokines |
|
|
Growth Factors
|
Essential for
the growth of fibroblasts and blood vessels and the regeneration of endothelial cells Stimulate the production of a wide variety of cless Initiate cell migration and differentiation tissue remodeling and wound healing |
|
|
Granulation Tissue
|
hallmark of healing inflammation
pink, soft granular appearance |
|
|
Angiogenesis
|
-proliferation, maturation, and organization of endothelial cells into capillary tubes
-Budding or sprouting of preexisitng vessels -Formation of new small blood vessels |
|
|
Wound healing response (primary union)
|
Wouund healing response is dependent on the extent of injury
wound healing by primary union -wound edges approximated by surgical sutures -without significant bacterial contamination -clean surgical incisions -minimal loss of tissues |
|
|
Wound healing response (secondary union)
|
-large tissue defect
-extensive loss of cells and tissue -the original architecture not reconstituted -large amounts of granulation tissue formed -larger areas of fibrosis or scar formation |
|
|
Signs of Infection
|
smelly, pink, yellow, brown or green
|
|
|
Cells involved in Foreign Body Reaction
|
macrophages, mutinucleated foreign body giant cells, fibroblasts, capillaries
(are at interface of implant for lifetime of implant) |
|
|
Fibrous Encapsulation
|
occur at the end stage of healing response (four or more weeks after implantation)
encapsulation thickness depends on the chemical activity of the material and thickness increases with increase relative motion between implant and the tissue encapsulation thicker over sharp edges |
|
|
What causes foreign body giant cells
|
production of small paricles by corrosion, depolymerization, dissolution or wear
|
|
|
FBR with implant with smooth and flat surfaces
|
encapsulation layer of macrophages one to two cells thick
|
|
|
FBR with implant with relatively rough surfaces
|
composed of multiple layers of macrophages and foreign body giant cells at the surface
|
|
|
FBR with implant with rough surfacs
|
macrophages and foreign body giant cells with varying degrees of granulation tissue
|
|
|
Delayed infection
|
happens witin 3 mons; slow development of introperative bacterial contamination
|
|
|
Late infection
|
months to years after surgery in sites of no prior history of infection
may be caused by transport and seeding of blood-borne bacteria from an established infection at a remote site |
|
|
Interaction mechanism for non-toxic releases
|
are reabsorbed
or stimulaes inflammation or enhances infections |
|
|
Interaction mechanism for no-toxic and non-absorbalbe
|
are encapsulated
|
|
|
Other interactions
|
highly interactive bonding to tissues (natural materials)
toxi substances |
|
|
Sequence of Host Rxn
|
Injury from an implantation process
Blood-material interactions Acute inflamation Chronic inflamation Granulation tissue Foreign body reaction- immune response Fibrosis/fibrous capsule development |
|
|
Local Host Rxns
|
-blood-biomaterial interactions
-modification of normal healing -Infection -Edema -Tumorigenesis |
|
|
Blood-biomaterial interactions
|
protein adsorption, coagulaiton, fibrinolysis, platelet activation, leukocyte adhesion, and hemolysis
|
|
|
Systemic Host Rxns
|
-Hypersensitivity
Thrombus, embolization -Fever -Pain |
|
|
Irritation
|
feeling of discomfort, sore and mild to moderate pain
|
|
|
Itching
|
surface phenomenon, chemical of physical incompatibility
|
|
|
Inflammation
|
a process of defensive response, much more severe response than irritation, redness, heat, swelling, and pain
|
|
|
Necrosis
|
tissue death
|
|
|
Pyrogenicity
|
tendency to trigger fever
|
|
|
sensitiation
|
a delay reaction, immunologically mediated allergies
|
|
|
mutagenicity
|
tendency to produce genetic mutation
|
|
|
Effects of Host on Implant
|
-mechanical-physical effect such as fatigue, corrosion, abrasive wear, micro-cracking, degeneration and dissolution
-biological effects such as adsorption of substances from tissues, enzymatic degradation, and calcification -Inflammation acute and chronic response |
|
|
Physiological events in inflammatory response
|
-vasoconstriction of vessels leading away from site
-vasodilation of vessel to the site -leucocytes slows down blood flow and adhere to vascular endothelium -leucocytes attach to vascular endothelium and increase expression of adhsion -increased permeability -influx of phagocytic cells into tissue |
|
|
Phagocytes movement
|
1) Neutrophils enters blood from bone marrow
2) Margination 3) Passes through capillaries (diapedesis) 4) Positive chemotaxis |
|
|
Margination
|
adherence of the cells to the endothelial wall
|
|
|
diapediesis
|
emigration between the capillary endothelial cells into the tissue
|
|
|
chemotaxis
|
chemically directed migration through the tissue to the site of the inflammatory response
|
|
|
Pus formation
|
accumulation of dead cells, digested materials, and fluid
|
|
|
Chemical mediators of Inflammation
|
histamine
-released by diff cell types -stimulates vasodialtion and inc. permeability lipid-derived chemical mediators chemokines other mediators: nitric oxide, peroxide, and oxygen radicals |
|
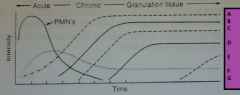
Relationship between intensity and time in inflammation process |
A: Macrophages
B: Neovascularization C:Foreign body giant cells D:Fibroblasts E: Fibrosis F: Mononuclear G: leukocytes |
|
|
lipid-derived chemical mediators
|
cell membrane phospholipids are hydrolyzed by phospholipases at a fairly high rate during inflamation
|
|
|
Prostaglandin
|
lipid-derived chemical mediator that increases vasodilation and vascular permeability and serves as chemoattractant for neutrophils
|
|
|
Leukotrienes
|
lipid-derived chemical mediator that increases smooth muscel contraction, serves as chemoattractant for neutrophils
|
|
|
Platelet-activating factors
|
lipid-derived chemical mediators that causes platelet aggregation and serve as chemoattractant for neutrophils
|
|
|
chemokines
|
major regulators of leukocyte traffic and help to attract leucocytes to the actual site of inflammation
|
|
|
Pro-inflammatory cytokines
|
ers increased hematopoiesis in the bone marrow, leading to leukocytosis
|

