![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
122 Cards in this Set
- Front
- Back
|
Phytohormones |
Plant |
|
|
“True”Hormones |
These are: regulatory actions in the target cells. |
|
|
Neurohormones |
Hormones which are released by neurosecretory cells (modified nerve cells) via |
|
|
Neurotransmitters |
These are released by presynaptic nerve cells |
|
|
Pheromones |
These are a) volatile chemical messengers |
|
|
Parahormones |
Hormone-‐like substances which are not |
|
|
Prohormones |
These can be a) large peptide molecules which may be processed into single or multiple Another definition: hormone precursors. Ex. POMC --> MSH + ACTH |
|
|
Growth Factors |
Hormone-like substances which promote growth of body or brain tissue: e.g., nerve growth factor (NGF) or epidermal growth factor (EGF) |
|
|
Cytokines |
Hormone-like factors released from lymphocytes, macrophages and other cells of the immune system which regulate the activity of the immune system (e.g., Interferon Y and the Interleukins) |
|
|
Vitamins |
Chemicals which regulate metabolism, growth and development in the body. Vitamin D can be synthesized in the body and has many hormone-like properties |
|
|
Definition of a True Hormone |
1. Chemical messenger 2. Synthesized in ductless glands 3. Effective in minute quantities 4. Secreted into the circulatory system; transported into the body through the blood 5. Act at a distance - on receptors of SPECIFIC target cells 6. Physiological/biochemical action on target cell-regulating the action of that cell |
|
|
Examples of Physiological Regulators that are Not Hormones |
CO2, glucose |
|
|
Examples of Neurotransmitters |
Acetylcholine Dopamine Serotonin GABA |
|
|
Neurohormones |
Oxytocin Vasopressin LH-R H CRH Somatostatin |
|
|
Neuropeptides |
Substance P VIP Enkephalins CCK Bombesin Neurotensin
|
|
|
Hormones |
FSH, LH-Gonadosteroids TSH-Thyroid hormones ACTH-Corticosteroids B-Endorphins
|
|
|
Growth Factors |
NGF EGF FGF
|
|
|
Cytokines |
Interferons Interleukins |
|
|
Neuroregulator |
A general term for any chemical messenger which regulates the activity of a nerve cell. They can either be a neurotransmitter or a neuromodulator. |
|
|
Neuromodulators |
A chemical released by a neural, endocrine, or other type of cell and acts on a neuron to modulate its response to a neurotransmitter. One mechanism through which neuromodulators influence neural activity is by altering the permeability of the nerve cell membrane to ions such as sodium or chloride. The modulator can be a true hormone, neurohormone, parahormone or other type of chemical messenger. |
|
|
Neuropeptides |
These are hormones or non-hormone peptides that act as neuromodulators. Examples: ACTH (adrenocoricotropic hormone) and insulin, LH-RH (luteinizing hormone releasing hormone) are all hormone peptides. Examples of non-hormone peptides are bombesin and neurotensin |
|
|
Pituitary |
Master gland of hormones and endocrine. Controlled by the hypothalamis |
|
|
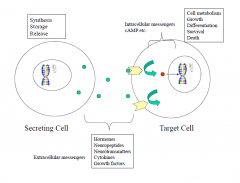
Secreting Cell: Synthesis, Storage, Release Target Cell: Cell Metabolism, Growth, Differentiation, Survival, Death Extracellular Messengers: Hormones, Neuropeptides, Neurotransmitters, Cytokines, Growth factors |
|
|
|
Pineal Gland Functions |
Reproductive Maturation, Body Rhythms |
|
|
Pituitary Gland (Anterior and Posterior) Functions |
A: Hormone secretion by thyroid, adrenal cortex, and gonads; growth. P: Water balance; salt balance. |
|
|
Thyroid functions |
Growth and development, metabolic rate |
|
|
Adrenal glands: Adrenal cortex and adrenal medulla |
Cortex: Salt and carbohydrate metabolism; inflammatory reactions Medulla: Emotional arousal |
|
|
Pancreas Functions |
Sugar Metabolism |
|
|
Gonads Functions |
Body development; maintenance of reproductive organs in adults |
|
|
Pineal Gland Hormone: Melatonin |
-modulates gonadal activity -mediates responses to light -alters pigment coloration |
|
|
Thyroid Hormones: Thyroxin (T4) and Triiodothyronine (T3) |
Regulates cell growth and differentiation, especially bone growth and neuronal growth |
|
|
Thyroid Hormone: Calcitonin |
Lowers blood calcium levels |
|
|
Parathyroid Hormone (PTH) in the Parathyroid |
Raises blood calcium levels |
|
|
Thymus Hormone: Thymosin |
Stimulates lymphocyte production and differentiation (T cells) |
|
|
Heart Hormone: Atrial Natriuretic Factor (ANF) |
Regulates blood pressure, blood volume, and electrolyte balance. |
|
|
Stomach Hormone: |
Stimulates secretion of HCL and increases intestinal motility |
|
|
Duodenum (Small Intestine) Hormones: Secretin Cholecystokinin |
S: Stimulates secretion of pancreatic juices C: Stimulates gall bladder contraction and pancreatic enzyme secretions |
|
|
Pancreas (Islets of Langerhans) Hormones: Insulin (Beta cells) Glucagon (Alpha cells)
|
I: Lowers blood glucose and promotes synthesis of fat and protein G: Increases blood glucose and promotes breakdown of fat and protein |
|
|
Adrenal Cortex Hormones: Glucocorticoids (Cortisol, Corticosterone) Sex steroids |
G: Converts stored fats and proteins into carbohydrates; anti-inflammatory; anti-allergy; anti-immune function M: Increases sodium retention and potassium loss in kidney |
|
|
Adrenal Medulla Hormones: Epinephrine (Adrenaline) Norepinephrine (Noradrenaline) |
E: Increases heart rate, oxygen consumption, and glycogen mobilization N: Increases blood pressure, constricts blood vessels |
|
|
Testis Hormones: (Leydig cells) Androgens (Testosterone) (Sertoli cells) Inhibin |
A: Male sexual characteristics I: Inhibits FSH secretion from pituitary |
|
|
Ovaries Hormones: Follicles - Estrogens Corpus luteum - Progesterone Relaxin |
E: Female sexual characteristics P: Maintains pregnancy; facilitates uterine and breast development. R: Relaxes birth canal and dilates uterine cervix at birth. |
|
|
Placenta Hormones: Human chorionic gonadotropin (HCG) Human Placental lactogen (HPL) Progesterone |
HCG: Maintains progesterone synthesis from ovaries; acts like pituitary LH HPL: Mammary gland growth and development; acts like pituitary LH and prolactin P: Maintains pregnancy |
|
|
Adipose Tissue Hormones: Leptin and Resistin |
L: Regulates hypothalamic control of body weight. Decreases eating and increases energy use. R: Anti-insulin
|
|
|
Neurohypophysis |
-Posterior Pituitary, also called Pars Nervosa -Neural tissue which is an extention of the hypothalamus attached to the hypothalamus by the hypophyseal stalk (the portion of the stalk it is on is the infundibulum) -Neurosecretary cells located on the paraventricular nucleus (PVN) and supraoptic nucleus (SON) of the hypothalamus -These two nuclei manufacture oxytocin and vasopressin |
|
|
Adenohypophysis (True Endocrine Gland) |
Contains anterior lobe (pars distalis), intermediate lobe (pars intermedia) of the pituitary and pars tuberalis (The pars tuberalis is part of the anterior lobe of the pituitary gland, and wraps the pituitary stalk in a highly vascularized sheath) |
|
|
Pars Nervosa |
Two hormones are oxytocin and vasopressin, which are really hypothalamic hormones. They are manufactored in the PVN and SON and transported through the infundibulum in the axons of these neurosecretory cells to the pars nervosa where they are stored in nerve terminals and then released into the inferior hypophyseal artery through which they enter the blood stream. |
|
|
Oxytocin |
Two primary functions: Promotes uterine contractions at time of birth and stimulates milk ejection from the mammary glands during lactation. It also has a number of neuropeptide functions in the brain. |
|
|
Vasopressin (or antidiuretic hormone ADH) |
Acts to raise blood pressure and promote water reabsorption in the kidneys, i.e. it acts as a diuretic. As a central neuropeptide, vasopressin may enhance memory. |
|
|
Neurophysins |
Two large proteins released from the pars nervosa. They are carrier proteins for oxytocin and vasopressin. |
|
|
Pars distalis hormone: Growth hormone (GH) |
Somatotropin = Somatotropin hormone. Promotes protein synthesis and carbohydrate metabolism and growth of bone and muscle by stimulating somatomedins. |
|
|
Pars distalis hormone: Adrenocorticotropic hormone (ACTH) |
Stimulates glucocorticoid secretion from the adrenal cortex |
|
|
Pars distalis hormone: Thyroid stimulating hormone (TSH) |
Thyrotropin: stimulates thyroxine (T4) and triiodothyronine (T3) secretion from the thyroid gland. |
|
|
Pars distalis Hormone: Prolactin (PRL) |
Initiates milk production and secretion in the mammary glands and has many other functions, including stimulating of the gonads. |
|
|
Gonadotropic Hormones: Follicle Stimulating Hormone (FSH) |
Stimulates growth of the primary follicle and estrogen and inhibin secretion from the ovary in females; sperm production and inhibin secretion in the testis of males |
|
|
Gonadotropic Hormones: Luteinizating Hormone (LH) |
Stimulates ovulation, formation of the corpora lutea and progesterone secretion in females; stimulates Leydig (interstitial) cells to secrete androgens in males. |
|
|
Pars Intermedia Hormones: Melanocyte Stimulating Hormone (MSH) |
Stimulates melanophores to darken skin color in amphibia. Some evidence for a similar effect in humans. |
|
|
Pars Intermedia Hormones: Beta endorphin |
Acts as a neurotransmitter in the brain to regulate neurotransmitter release, and possibly as a circulating analgesic. |
|
|
Functions of the hypothalamus |
1. Neuroendocrine |
|
|
Hypothalamus Location |
Between the pituitary and the third ventricle, at the base of the forebrain. It is divided in two by the third ventricle and filled with cerebrospinal fluid |
|
|
Medial basal hypothalamus (also known as the endocrine hypothalamus) |
Since the hypothalamus is full of nerve cell bodies (nuclei), this consists of ventromedial nuceli (VMN), as well as arcuate nuclei and the median eminence. |
|
|
Neurosecretory Cells |
Modified nerve cells which, rather than secreting a neurotransmitter, release a hormone into circulation for neuroendocrine communication. |
|
|
Two types of hypothalamic neurosecretary cells |
1. Magnocellular: Located in the PVN (paraventricular nuclei) and supraoptic nuclei (SON). Consists of two cell types: one that produces oxytocin and one that produces vasopressin. 2. Parvicellular system: The smaller parvicellular neurosecretiry cells are found in the preoptic area, VMN, and arcuate nucleus, as well as various other hypothalamic areas and project to median eminence. This also has a lot of smaller parvicellular cells. These hormones modulate the release of adenohypophyseal hormones and are thus referred to as the "hypophysiotropic hormones". |
|
|
Three criteria definition for hypothalamix hypophyseal hormones |
a) hormone must be present at the median eminence of the hypothalamus b) is present in higher levels in the hypophyseal portal blood than in the rest of the circulatory system c) the level of the hormone in the hypophyseal portal blood is correlated with the secretory rate of particular adenohypophyseal hormones |
|
|
Afferent systems |
Cortical Visceral Olfactory Visual Somatosensory Auditory Limbic |
|
|
Efferent Systems |
Median Eminence (parvicellular) Posterior Pituitary (magnocellular) Sympathetic and parasympathetic preganglionic cell groups in the spinal cord and stem cell Amygdala, other cortical/subcortical regions for behavioural responses |
|
|
Paraventricular nuclei (PVN) |
-Synthesis of oxytocin, vasopressin and neurophysins from the |
|
|
Lateral Hypothalamus (LH) |
-Control of hunger |
|
|
Dorsomedial nuclei (DMN) |
-Synthesis of TRH, CRH and somatostatin |
|
|
Ventromedial nuclei (VMN) |
-Synthesis of GH-RH, somatostatin, CRH, PRF and TRH |
|
|
Hypothalamic Hypophysiotropic Releasing Hormones |
1. Thyrotropin Releasing hormone (TRH) = TSH=RH |
|
|
Hypothalamic Hypophysiotropic Paired releasing and inhibiting hormones |
4. Growth Hormone Releasing Hormone (GH-RH) |
|
|
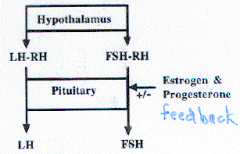
Two Gonadotropin theory |
|
|
|
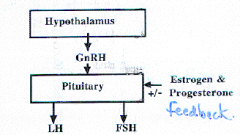
One gonadotropin theory |
|
|
|
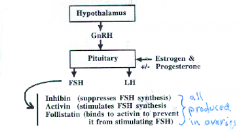
The current theory |
|
|
|
Luteinizing Hormone |
a) stimulates ovulation and secretion of testosterone b) stimulates FSH secretion c) initiates milk production d) hastens menstruation in women e) is produced by corpus luteum |
|
|
Complexities of Hypothalamic - Pituitary Interaction |
1. There is not a 1:1 correspondence between hypothalamic and pituitary hormones 2. Pituitary hormones feed back to alter the release of hypothalamic hormones 3. Hypothalamic hormones are released in other parts of the brain areas (extra-hypothalamic secretion) |
|
|
Eight criteria of a true neurotransmitter |
1. Substance must be present in presynaptic neurons 2. Neurotransmitter precursors and synthetic enzymes must be present in the neuron 3. Stimulation of nerve afferents (dendrites) should cause the release of substance in physiologically significant amounts 4. Effects of direct application of the substance to the synapse should be identical to those produced by stimulating nerve afferents 5. Specific receptors that interact with the substance should be present in close proximity to the presynaptic neurons 6. Interaction of the substance with its receptors should induce changes in postsynaptic membrane permeability leading to excitatory or inhibitory postsynaptic potentials in the postsynaptic cell 7. Specific inactivating mechanisms should exist which stop interactions of the substance with its receptor in a physiologically reasonable time frame 8. Interventions at postsynaptic sites using agonist drugs should mimic the action of the transmitter and antagonists should block its effects |
|
|
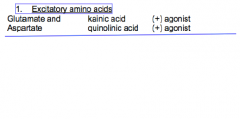
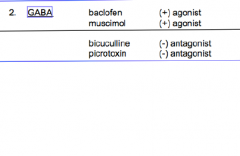
Amino acid transmitters: Excitatory Inhibitory |
E: Aspartic acid Glutamic acid I: GABA, glycine |
|
|
Cholinergic Neurotransmitter |
Acetylcholine (ACh) |
|
|
Monoamine neurotransmitters: Adrenergic (catecholamines) Indoleamine Other |
A: Dopamine, Norepinephrine, Epinephrine I: Serotonin O: Histamine |
|
|
Peptide transmitters |
Substance P Somatostatin Neurotensin Cholecystokinin Enkephalins, endorphins |
|
|
Putative neurotransmitters |
Endogenous benzodiazepines Prostaglandins |
|
|
Free radicals |
Nitric Oxide (NO) |
|
|
Five functions of synaptic vesicles |
1. Axonal transport of transmitter 2. Storage of transmitter 3. Completion of transmitter synthesis 4. Protect transmitter from deactivation 5. Release of transmitter by exocytosis |
|
|
Amino acids necessary for transmission synthesis |
Acetylcholine <- choline Catecholamines <- tyrosine Serotonin <- tryptophan |
|
|
Glutamate and aspartate (EAAs) receptors |
A1 (NMDA), A2, A3, A4 Located on the brain and binds to glutamate and aspartate |
|
|
GABA receptors (IAAs) |
(Types A and B) Located on postsynaptic nerves (A type) and may regulate the release of neurotransmitters (B type) |
|
|
Cholinergic Receptors |
Muscarinic (M1 and M2) Located on pre and postsynaptic neurons in the parasympathetic nervous system, corpus striatum, hindbrain, hypothalamus, cerebellum, heart and stomach and brain. |
|
|
Nicotinic (N1 and N2) |
Located on skeletal muscles at neuromuscular junctions and in autonomic ganglia and brain |
|
|
Adrenergic Receptors a. Dopamine (D1 and D5) D2 D3 and D4 |
D1 and D5: Located in parathyroid gland and brain (cortex and limbic system); stimulates cyclic AMP production D2: Located in brain (limbic system) and anterior pituitary; inhibits cyclic AMP synthesis D3 and D4: Located in the limbic system and the cortex |
|
|
Adrenergic Receptors: Norepinephrine and epinephrine -Alpha adrenergic (a1 and a2) -Beta adrenergic (B1 and B2) |
A: Located on postsynaptic cells in heart and brain a1 and presynaptic cells in pancreas, duodenum, and brain a2. Causes contraction of smooth muscle (a1) B: Located in heart, lung, and brain. Stimulate the contraction of heart muscle and relax smooth muscle of intestine and lungs. Activates adenylate cyclase. |
|
|
Serotonin Receptors (5-HT1, 5-HT2, 5-HT3) |
Located in brain and circulatory system & to regulate contractions of blood vessels. 5-HT2 receptors in brain regulate behavioural effects of serotonin. 5-HT3 seems to be important in the vomiting reflex. |
|
|
Histamine Receptors (H1 and H2) |
Mediate bronchial constriction in lungs (H1) and gastric secretion in stomach (H2). Also occur in muscle, cardiovascular system, brain, and immune system. |
|
|
Opiate receptors: Mu |
In brain and spinal cord to regulate pain; implicated in analgesia; morphine selective |
|
|
Opiate receptors: Delta
|
Located in limbic system of brain; may mediate epilepsy and rewarded behaviour; selective for enkephalins |
|
|
Opiate receptors: Kappa (K) |
Located in cerebral cortex; mediate sedative analgesia; selective for dynorphin |
|
|
Opiate receptors: Sigma Epsilon
|
S: Located in hippocampus; mediates psychomimetic opiate effects E: B-endorphin sedative |
|
|
Benzodiazepine Receptors |
Type 1: Located on postsynaptic cells Type 2: Located on presynaptic cells GABA receptors: Benzodiazepine receptors are also part of the GABA receptor complex |
|
|
Neurotransmitters and deactivating enzymes |
1. GABA: GABA-transaminase (GABA-T) 2. Acetylcholine: Acetylcholinesterase (cholinesterase) 3. Catecholamines: monoamine oxidase, catecol-O-methyltransferase (COMT) 4. Serotonin: monoamine oxidase 5. Histamine: histaminase 6: Neuropeptides: peptidases |
|
|
Cholinergic pathways |
Through the basal forebrain (nucleus basalis, medial septal nucleus of diagonal band), hippocampus, fornix, cerebellum, pedunculopontine nucleus and laterodorsal tegmental nucleus. |
|
|
Dopaminergic Pathways |
Mesolimbocortical: ventral tegmental area to nucleus accumbens, cortex, and hippocampus Mesostriatal: substantia nigra to striatum |
|
|
Noradrenergic pathways |
Locus coerulus, lateral tegmental area, cerebellum, to spinal cord |
|
|
Serotonergic pathways |
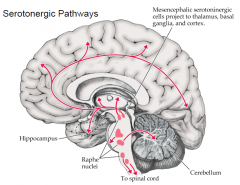
|
|
|
GABA |
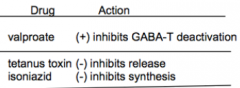
|
|
|
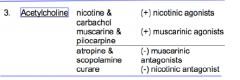
Acetylcholine |
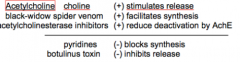
|
|
|
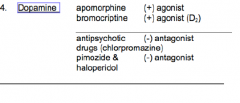
Dopamine |
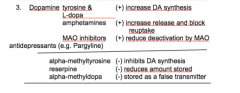
|
|
|
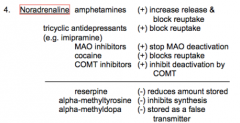
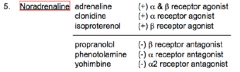
Noradrenaline |
|
|
|
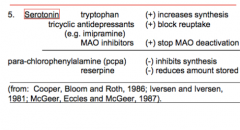
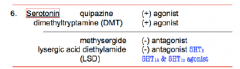
Serotonin |
|
|
|
Excitatory amino acids |
|
|
|
GABA |
|
|
|
Acetylcholine |
|
|
|
Dopamine |
|
|
|
Noradrenaline |
|
|
|
Serotonin |
|
|
|
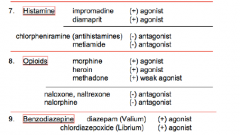
Histamines, opioids, benzos |
|
|
|
Four ways which neurotransmitters (nerves) act to regulate hypothalamic hormones |
1. Through a synapse in the neural pathway carrying sensory input or input from other brain regions (indirect) 2. A direct synapse of axons from extra-hypothalamic neurons to neuroendocrine cells, on cell body or dendrite 3. A direct synapse on axons of the neurosecretory cell 4. Neurotransmitters can be released into hypophyseal portal veins and act directly on the pituitary gland (e.g. dopamine) |
|
|
Complications in the study of the neurotransmitter control of hypothalamic hormone release |
1. Multiple NT interactions may be necessary to stimulate hypothalamic hormone release 2. The neuroendocrine response depends on the presence or absence of other hormones 3. Drugs used to alter NT levels may not be specific in their actions 4. Anesthesia along with the neurotransmitter may cause a different effect 5. In vivo and in vitro give different results 6. There are potential species differences in endocrine responses 7. Sex differences in endocrine responses 8. Psychological factors such as stress may alter neuroendocrine responses 9. Multiple hypothalamic-pituitary interactions may affect neuropeptide responses 10. Hypothalamic control of pituitary hormones is not 1:1 |
|
|
Some problems in the use of drugs to study effects of neurotransmitters in hormone release. |
1. Two drugs with same actions may have different endocrine effects by binding to different receptors 2. Different doses of the same drug may have different effects on hormone release 3. Different routes of drug administration may result in different effects of a drug on hormone release |
|
|
Psychotropic drugs |
-Alter levels of NT and thus disturb the neuroendocrine system -L-dopa leads to decreased prolactin secretion and increased GH output -antipsychotics lead to increased prolactin secretion -Antidepressents (tricyclics and MAOI) modulate GH and ACTH secretion via increasing serotonin levels |
|
|
Problems with definitions |
1. it is difficult to distinguish among true hormones, neurotransmitters, and neuropeptides 2. Release of hypothalamic hormones depends on many factors: multiple NT interactions hormone feedback "emotions" neuropeptides 3. Hypothalamic control of pituitary hormones is complicated by NT release (dopamine) one hypothalamic hormone can affect one or more pituitary hormone |
|
|
Pulsatile secretion versus tonic |
Pulsatile: If a bunch of neurotransmitters take a while to be released, they need to take time to be created so a bunch get secreted at once. Tonic: a bunch get made and secreted at once |

